Abstract
We report a case of common bile duct (CBD) cancer, successfully managed with pancreaticoduodenectomy, in a patient with isolated levocardia, malrotation, and situs ambiguous (without splenic anomalies). A 59-year-old male patient was referred to Chung-Ang University Hospital with epigastric pain and jaundice. CT and MRI revealed distal CBD cancer without significant lymphadenopathy. Multiple abdominal anatomic anomalies were identified preoperatively, whereas no anatomic anomalies were detected within the chest. The patient had a right-sided stomach and spleen, liver at the midline, several vascular variations around the celiac axis, and intestinal malrotation, but the inferior vena cava and portal vein were normal. A pancreaticoduodenectomy was performed to treat the cancer. The postoperative course was favorable, and the patient was started on combined chemotherapy and radiotherapy 15 days after the surgery. In this case study, we report that pylorus preserving pancreaticoduodenectomy was successful for distal CBD cancer in a patient with rare situs anomalies.
Situs solitus refers to the normal positioning of the thoracic and abdominal organs, while situs inversus is a congenital condition resulting in the reversal of internal organs from the right to the left side of the body [1,2]. Situs ambiguous is defined as the abnormal arrangement of the thoracic and abdominal organs, which are not clearly lateralized [3]. Congenital heart disease affects 50%-100% of patients with situs ambiguous [4]. Isolated levocardia is a rare complication of situs anomaly, in which thoracic situs solitus is noted along with dextro-positioning of the abdominal viscera such as situs inversus or situs ambiguous. Splenic and cardiac defects commonly accompany levocardia.
We recently encountered a patient with a rare form of situs ambiguous including the following: (1) isolated levocardia with a specific distribution of abdominal viscera, (2) malrotation of the intestines, and (3) a lack of splenic or cardiac anomalies. The anatomic anomalies of the patient were detected during preoperative imaging studies for possible common bile duct (CBD) cancer requiring a pancreaticoduodenectomy. Despite the rising incidence, cholangiocarcinoma is one of the most uncommon malignancies, and concomitant cholangiocarcinoma with situs ambiguous is even rarer. To our knowledge, pancreaticoduodenectomy in a patient with isolated levocardia, intestinal malrotation, and situs ambiguous without splenic defects, has not been previously reported. Here, we report the case of a patient in whom pylorus preserving pancreaticoduodenectomy was successful in the setting of rare situs anomalies.
A 59-year-old male patient presented with epigastric pain and jaundice. With the exception of diabetes mellitus, the patient had no significant past medical, surgical, or family history as well as no prior hospitalizations. During physical examination, the patient was alert and afebrile, although he was jaundiced, as evidenced by icteric sclera. Abdominal examination revealed epigastric pain without tenderness. Abdominal inspection revealed no evidence of distension or palpable masses.
AST/ALT and total bilirubin/direct bilirubin levels were elevated (251/415 IU/L [normal, <34/40 IU/L] and 9.7/7.9 mg/dL [normal, <1.3/0.4 mg/dL]). In addition, marked elevations in the levels of ALP and γ-GT were noted (2,466 IU/L [104 IU/L < normal < 338 IU/L] and 949 IU/L [5 IU/L < normal < 55 IU/L]). The levels of serum tumor marker CA 19-9 were also elevated (205.0 U/mL [normal, <27 U/mL]).
CT scan revealed segmental concentric wall thickening in the suprapancreatic CBD, with biliary tree dilatation and abnormal intra-abdominal organ positioning. We determined that the liver was located in the middle of the upper abdomen, and that the gallbladder was in the middle of the upper abdomen. The inferior vena cava and portal vein showed nonspecific changes. The spleen was located in the right upper quadrant. In addition, the locations of the stomach and pancreas were reversed (Fig. 1). As a chest radiograph showed no specific abnormalities, a diagnosis of isolated levocardia with situs ambiguous was confirmed.
For additional information on the concentric wall thickening in the suprapancreatic CBD, MRI, and PET CT were performed. Both imaging modalities suggested the presence of a focal cancerous lesion of the distal CBD, without significant lymphadenopathy. Therefore, we decided to carry out a surgical exploration based on the radiographic findings that were suggestive of distal CBD cancer.
Upon opening the peritoneum, we noticed that the intraabdominal organs were not in their normal locations. The right liver lobe was located in the upper right-hand quadrant of the abdominal cavity, resting just below the right diaphragm, and the gall bladder was just beneath the right liver lobe, as was previously known. The left lobe of the liver was as large as the right lobe, and its anatomical segment was not clearly separated. The stomach and spleen were located in the upper right-hand quadrant of the abdomen under the right liver lobe, but there appeared to be no splenic defects or anomalies. Additionally, the stomach and first part of the duodenum were reversed and faced the left side. We were able to distinguish the first and second part of the duodenum; however, after the third part, the duodenum and jejunum were not clearly identified because the ligament of Treitz was absent. This indicated that the third and fourth parts of the duodenum were located in the peritoneal space, rather than retroperitoneally. The head of the pancreas was found on the second portion of the duodenum, and the uncinate process had not developed. The body of the pancreas was behind the stomach, and the tail was oriented toward the upper right-hand abdominal quadrant leading to the spleen. The small intestine was completely pushed to the right side of the abdomen, and the large intestine was present on the left side of the abdomen. Interestingly, the ascending colon was found to be a freely movable structure, because it was not fixed by the gastrocolic or duodenocolic ligaments (Fig. 2).
After omentectomy, cholecystectomy, and dissection around the CBD had been successfully performed, the margin of the proximal bile duct was found just below the hepatic duct bifurcation. Mobilization of the pancreas head and duodenum from the portal vein was carried out with a reverse-Kocher maneuver. The duodenum was subsequently transected, and the stomach was moved upward to allow for an easier approach to the pancreas. Pancreaticoduodenectomy was performed with end-to-end pancreaticojejunostomy, end-to-side duodenojejunostomy, and end-to-side hepaticojejunostomy (Fig. 3).
The total operation time was 605 minutes, and the estimated intraoperative blood loss was 200 mL. Histopathology revealed a moderately differentiated adenocarcinoma of the CBD, and the tumor was classified as T3N0M0 stage IIA according to the TNM staging system of the American Joint Committee on Cancer. There was invasion into the pancreas and duodenum, but no involvement of the CBD, pancreatic, or duodenal resection margins. In addition, no metastasis was noted in the lymph nodes, which were removed intraoperatively.
The patient recovered without major complications. Seven days after surgery, a follow-up abdominopelvic CT scan was performed that showed no abnormalities. Fifteen days after the operation, the patient was started on combined chemotherapy and radiotherapy.
Situs inversus is a condition in which the internal organs are reversed or mirrored from their normal positions. The incidence of situs inversus is approximately 1 in 10,000 [2]. The abnormal location of organs and vessels in a manner that is not clearly lateralized is known as situs ambiguous, which has an estimated incidence of at least 1 in 40,000 live births [5]. Situs anomaly accompanied by isolated levocardia, malrotation, and situs ambiguous, but without splenic or cardiac malformations, is extremely rare. A review of previous medical literature revealed only 12 reported cases of isolated levocardia without splenic or cardiac anomalies [6,7], and 5 reported cases of isolated levocardia with intestinal malrotation [7,8,9].
Cholangiocarcinoma is also not a common malignancy of the gastrointestinal tract and has a reported incidence in the United States of 1 or 2 per 100,000 patients [10]. In this patient, all the unusual conditions discussed here as well as cholangiocarcinoma, were present-making this case even rarer. To the best of our knowledge, this report is the first to demonstrate the performance of a pancreaticoduodenectomy in a patient with isolated levocardia, intestinal malrotation, and situs ambiguous without splenic malformations (literature search conducted through PubMed).
During the surgery, the surgeon stood on the right side of the patient as usual, and the surgical procedure was performed in the standard order of a pylorus preserving pancreaticoduodenectomy. A number of important findings during the surgery deserve additional attention.
Firstly, anatomical variations of the vessels of the celiac trunk and superior mesenteric artery (SMA) were found. In this patient, the right gastric artery, normally derived from the common hepatic artery (CHA), arose directly from the celiac trunk (Fig. 4). In addition, the CHA and gastroepiploic artery originated from the SMA (Fig. 5). Specifically, the CHA was derived from the SMA at the inferior border of the pancreas and ran along the anterior surface of the pancreas to the liver. The course of the CHA was just above the neck of the pancreas, and was close to the resection margin; hence, extra care was taken while skeletonizing the CHA. After the resected pancreas head and duodenum were out of the way, repositioning of the skeletonized CHA presented a challenge. The proximal jejunum of the pancreaticojejunostomy was constricted, and the intraluminal passage of the proximal jejunum could easily have been disturbed by the position of the CHA. Therefore, we decided to place the CHA under the proximal jejunum, and performed the pancreaticojejunostomy (Fig. 3).
Secondly, the head of the pancreas only covered the anterior wall of the portal vein, indicating that the uncinate process was absent. Most surgeons take great care while detaching the head of the pancreas from the inferior vena cava with the Kocher maneuver. Because the head of the pancreas was smaller than that of a normal pancreas, a Kocher maneuver could be easily performed. In addition, more than half of the pancreas was located in the peritoneal cavity, rather than the retroperitoneum, making it convenient to dissect the head of the pancreas.
Thirdly, malpositioning of the intestines due to congenital gut malrotation made proper identification of the visceral anatomy time consuming and difficult, leading to an extended operation time. However, it offered surgical benefits in other ways. For example, the duodenojejunal and hepatic flexures, which consist of the ligament of Treitz and the gastrocolic and duodenocolic ligaments, were absent. Therefore, some surgical procedures could be omitted, such as the creation of a window in the mesocolic attachment of the duodenum, using an extensive Kocher maneuver and pulling the jejunal loop into the right upper abdomen through the mesocolic window.
In conclusion, careful identification of anatomical anomalies using radiological imaging tools such as CT should be conducted prior to surgery in cases of situs ambiguous. Intestinal malrotation itself does not disrupt the surgical procedure, and its presence may be beneficial when attempting to reposition the proximal jejunum for anastomosis. Therefore, despite the rarity, if careful preoperative preparation and intraoperative examination of abdominal organs are carried out, a pancreaticoduodenectomy can be safely and successfully performed in a patient with isolated levocardia, intestinal malrotation, and situs ambiguous, who does not have splenic malformations.
Figures and Tables
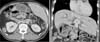 | Fig. 1CT scan demonstrating a mass in the suprapancreatic common bile duct and abnormal positioning of intra-abdominal organs. Ao, aorta; Gb, gallbladder; H, heart; L, liver; P, pancreas; PV, portal vein; Sp, spleen; St, stomach; TM, tumor mass. |
 | Fig. 2Schematic diagram of perioperative findings. Medial displacement of the liver but normally sided gallbladder and biliary duct, reversed pancreas and spleen, totally left-sided small intestine, and totally right-sided large intestine. C, colon; Gb, gallbladder; L, liver; P, pancreas; Sp, spleen; St, stomach. |
 | Fig. 3Intraoperative photography after reconstruction. Common hepatic artery was positioned under the pancreaticojejunostomy. CBD, common bile duct; P, pancreas; St, stomach. |
References
1. Fulcher AS, Turner MA. Abdominal manifestations of situs anomalies in adults. Radiographics. 2002; 22:1439–1456.
2. Douard R, Feldman A, Bargy F, Loric S, Delmas V. Anomalies of lateralization in man: a case of total situs inversus. Surg Radiol Anat. 2000; 22:293–297.
3. Peeters H, Devriendt K. Human laterality disorders. Eur J Med Genet. 2006; 49:349–362.
4. Peoples WM, Moller JH, Edwards JE. Polysplenia: a review of 146 cases. Pediatr Cardiol. 1983; 4:129–137.
5. Rose V, Izukawa T, Moes CA. Syndromes of asplenia and polysplenia. A review of cardiac and non-cardiac malformations in 60 cases withspecial reference to diagnosis and prognosis. Br Heart J. 1975; 37:840–852.
6. Chacko KA, Krishnaswami S, Sukumar IP, Cherian G. Isolated levocardia: two cases with abdominal situs inversus, thoracic situs solitus, and normal circulation. Am Heart J. 1983; 106(1 Pt 1):155–159.
7. Beaudoin S, Seror O, Fayad F, Grapin C, Sellier N. A case of malrotation and situs ambiguus. Surg Radiol Anat. 1999; 21:143–145.
8. de Reus HD, Heckman J, von der Hal I. A rare combination of congenital disorders in a 5-year-old girl. Levocardia with situs inversus abdominalis and duodenal obstruction caused by malrotation and an intraluminal diverticulum. Tijdschr Gastroenterol. 1969; 12:58–92.
9. Budhiraja S, Singh G, Miglani HP, Mitra SK. Neonatal intestinal obstruction with isolated levocardia. J Pediatr Surg. 2000; 35:1115–1116.
10. Carriaga MT, Henson DE. Liver, gallbladder, extrahepatic bile ducts, and pancreas. Cancer. 1995; 75:1 Suppl. 171–190.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download