Abstract
Purpose
We evaluated the adequacy and feasibility of a tumescent solution containing lidocaine and bupivacaine for inguinal hernia repairs.
Methods
The medical records of 146 consecutive inguinal hernia patients with 157 hernia repairs using the tumescent local anesthesia technique performed by a single surgeon between September 2009 and December 2013 were retrospectively reviewed.
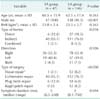
Although local anesthesia for inguinal hernia repair has been described since the beginning of the last century, it was not until the 1950s that the routine use of local anesthesia for inguinal herniorrhaphy gained acceptance [1]. As the method of operation has changed over time, the anesthesia method has also varied. Although past reports have provided evidence of the safety and efficacy of local anesthesia for hernia [2,3], it is not widely performed. Sanjay and Woodward [3] reported that only 15% of doctors in Wales, United Kingdom usually perform hernia operations using local anesthesia. However, many hernia centers have reported that most operations are performed under local anesthesia [4,5,6]. In some reports that were published in Korea, the reported rate of hernia surgery using local anesthesia varies widely, from 0% to 100% [7,8,9,10,11] (Table 1). Specifically, although local anesthesia was reported to be effective for pain and safety, most of the subjects in those studies were either patients who had risk associated with general anesthesia or spinal anesthesia or were elderly. However, the choice of anesthetic technique should be based on the type and extent of the surgical procedure, concomitant medical disease and the effects of anesthetic agents on organ function [12]. The aim of this study was to analyze the feasibility and safety of routine use of the tumescent local anesthetic (TLA) technique.
The medical records of 146 patients who had undergone inguinal hernia repair operation by single surgeon (D.G.S.) at Seoul Medical Center between September 2009 and December 2013 were retrospectively reviewed, and the data were compared with 47 inguinal hernia operations performed under spinal anesthesia between 2004 and 2008. There was no definite indication for local anesthesia during inguinal hernia surgery. However, relative contraindications of local anesthesia during inguinal hernia surgery were (1) age <20 years old, (2) suspected strangulation, (3) multiple recurring inguinal hernias, (4) lack of patient cooperation (patient refused local anesthesia or was physically or mentally unstable), (5) a need or plan for other combined surgery, and (6) lidocaine allergy or severely decreased liver function.
Tumescent local anesthesia infiltration technique: Infiltration anesthesia was performed by the surgeon with 1% lidocaine skin infiltration to achieve rapid local anesthesia at the incision line. A 5-cm transverse skin incision was made, and the skin was opened. A TLA solution (2% lidocaine 10 mL + 0.5% bupivacaine 10 mL + 0.1% epinephrine HCl 0.1 mL mixed with 80-mL normal saline made 100-mL TLA) was prepared just before surgery by the scrub nurse and injected from the subcutaneous tissue to the fascia layer after skin anesthesia. Then TLA solution was then injected step by step. Sedation was provided with small doses of midazolam. Intraoperative monitoring of heart rate and blood pressure and verbal contact between the patient and the surgeon were maintained during local anesthesia.
Operation technique used: standardized surgical techniques were used according to the type of hernia. A high ligation was only performed in six young patients. Six cases of Bassini repair were performed for small indirect hernias. Lichtenstein repairs were performed for medium to large indirect inguinal hernias in 112 cases. Ten cases of modified plug-mesh repair were performed for direct and pantaloon hernias. Twelve cases of modified Kugel patch repairs were performed for large direct inguinal hernias. The size of the hernia defect was measured according to the surgeon's fingertip width. (small hernia, less than the one fingertip width; medium, one to two fingertip width; large, more than two fingertip width).
We reviewed the patients' clinical characteristics (age, body mass index, type of hernia, direction, operation type, symptom duration and comorbidity state) and operative results. We conducted telephone interviews to collect information about recurrence.
Regarding the statistical analysis, continuous variables (age, body mass index [BMI], symptom duration) were dichotomized using the mean value of each variable. The chi-square test or Fisher exact test and independent 2-tailed t-tests were used to compare the clinicopathological parameters and surgical outcomes between the spinal anesthesia group and the local anesthesia group wherever appropriate. Values were expressed as the mean (standard deviation, SD) or median (range) as appropriate. Probabilities of less than 0.05 were considered significant. All the data collected from the database were analyzed using SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA).
A total of 146 adult hernia patients with 157 hernia repairs were examined. Four operations were performed for recurrent hernias. There was no conversion from local anesthesia to spinal or general anesthesia. The mean age was 62.5 ± 17.4 years. Data related to the general characteristics of the hernia patients (age, gender, BMI, type of hernia, direction, symptom duration and comorbidity) are presented in Tables 2, 3. Among the 146 cases, 111 (76%) were indirect-type hernias, 78 (53.4%) were right side, and 57 (39%) were left side. The most common comorbidities were hypertension (52 patients, 35.6%), benign prostate hyperplasia (45 patients, 30.8%), constipation (32 patients, 21.9%), diabetes mellitus (16 patients, 11%) and chronic lung disease (15 patients, 10.2%). At a mean follow-up of 24 ± 14 months, there were four recurrences (2.5%) among the 146 patients. The success rate of telephone contact was 87.6% (128/146 cases). The other patients (28 cases) were reviewed only via their outpatient follow-up chart records.
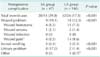
The mean operation time was 61.4 ± 16.4 minutes, which was shorter than the operation time of the spinal anesthesia group (85.7 ± 25.5 minutes, P < 0.001). The mean length of hospital stay was 2.63 ± 1.8 days, which was also shorter than that of the spinal anesthesia group (4.9 ± 1.8 days, P < 0.001).
A total of 32 postoperative complications occurred in 26 patients (17.8%). Wound problems were the most common postoperative complication. Twenty-seven events (wound pain, 14 cases; wound hematoma, 11 cases; wound seroma, 2 cases) occurred in 23 patients (15.7%). Other complications included scrotal swelling (3 cases, 2.1%) and postoperative voiding difficulty (2 cases, 1.4%). There was no case of wound infection. Postoperative voiding difficulty occurred significantly more frequently in the spinal anesthesia group (8 cases, 17%) compared with the local anesthesia group (2 cases, 1.4%; P < 0.001) (Table 4). The postoperative one-day mean ± SD visual analogue scale score was 3.88 ± 1.53; it significantly decreased to 1.69 ± 1.41 at seventh postoperative day (P < 0.001).
After the tension-free technique was first introduced by Lichtenstein, diverse tension free surgical procedures for inguinal hernia evolved, including prolene hernia system repair, direct and indirect Kugel patch repair and laparoscopic herniorrhaphy. It is difficult to conclude which method is suitable for inguinal hernia treatment, but it seems to be easy and reasonable to discuss which anesthetic technique is suitable for open inguinal hernia surgery. Lawrence et al. [13] reported that laparoscopic hernia repair appears to be an expensive option; however, the local anesthesia technique has a short learning curve that requires simple training. The technique is easy to learn and apply, and it is an economic option for open anterior repairs. Therefore, every surgeon should be capable of not only performing current repair methods but also applying local anesthesia successfully in his/her daily practice.
Previously established operative advantages of the local anesthesia technique include reduced bleeding (when adrenaline-containing solutions are used), easier dissection because of the separation of tissue planes by local anesthetic infiltration (hydrodissection) and the ability to assess the adequacy of the hernia repair by asking a conscious patient to perform a Valsalva maneuver if necessary [14].
The single surgeon selected the same anesthetic method (usually spinal anesthesia) that the other surgeons used when he started working at this hospital in 2004. Most of the inguinal hernia repairs performed under general or spinal anesthesia were performed between 2004 and 2008; we started to perform inguinal hernia surgery under local anesthesia for adult patients since 2008. However, we began performing inguinal hernia repair using the TLA solution technique in September 2009, when the single surgeon in this study returned to work after finishing studying abroad. From September 2009 to December 2013, we performed 146 consecutive adult inguinal hernia operations under local anesthesia using the TLA solution, with no conversion to spinal or general anesthesia and didn't experience any other side effect of the local anesthetic drugs. During that period, eight cases were performed under spinal or general anesthesia because of other combined surgeries (two cases), lack of patient cooperation (five cases) and recurrence case (one case who had already undergone both inguinal hernia operations twice).
Recently, many local anesthetic techniques have evolved. Tumescent local anesthesia provides anesthesia over wide areas of skin and subcutaneous tissue via the direct infiltration of large volumes of dilute local anesthetic solution. Compare to conventional local anesthesia, it also provides excellent analgesia during surgery. Diluted anesthetics reduce the potential for lidocaine toxicity and it provides long-lasting analgesia postoperatively than conventional local anesthesia [15]. A step-by-step infiltration technique under direct surgical view seems to be safer than a percutaneous inguinal block for patients undergoing inguinal hernia repair because cadaveric dissection studies have suggested that inguinal block may cause femoral nerve injury [16,17].
Gultekin et al. [18] reported that local anesthesia reduced postoperative pain but did not lengthen the operation time. In our study, we found that the operation time was significantly shorter in the local anesthetic (LA) group than in the spinal anesthetic (SA) group (SA: 85.7 ± 25.5 minutes vs. LA: 64.5 ± 17.6 minutes, P < 0.05). We experienced eight cases of hernia recurrence; four cases among 47 spinal anesthesia cases (8.5%) and four cases among 157 local anesthesia cases (2.5%, P < 0.05). However, most of the local anesthesia surgeries were performed in the latter half of the study period (2009 to 2013). We can guess that the increasing number of the surgeon's cases might have affected the differences in operation time and recurrence rate between the two groups.
Sanjay and Woodward [3] reported that patients who underwent surgery under local anesthesia had lower postoperative analgesia requirements (P < 0.05) and a lower incidence of urinary retention compared with the general anesthesia (GA) group (GA: five patients, 2.4% vs. LA: two patients, 0.5%; P < 0.05). We also found that postoperative voiding difficulty was significantly more common in the SA group (eight patients, 17%) than in the LA group (two patients, 1.3%; P < 0.001).
In the past, we did not perform hernia repair under local anesthesia. As we have reported, general anesthesia was performed for 25 cases (20.6%), and spinal anesthesia was used for 97 cases (79.5%) among the 122 adult hernia patients in 2004 [7]. However, after 2008, we began to perform hernia surgery under local anesthesia, and the TLA solution injection technique has been used since September 2009. The mean length of hospital stay for this hospital was reduced from 6.8 days in 1989 to 4.8 days in 2004, and in this study, we found that the mean length of hospital stay was only 2.7 ± 1.5 days in the LA group. In the past, the patient was usually admitted before the operation day, and we started feeding on postoperative day one. Patients who underwent spinal anesthesia had to stay in bed for one day; if they could walk on postoperative day two, they could be discharged. Thus, a typical hospital stay lasted three to five days. However, during the local anesthetic method era, patients were admitted just before the operation started and were usually able to eat just after surgery. There were no strict discharge criteria for inguinal hernia patients. We always ask about the patient's intentions after surgery, and if the patient agrees, he or she can be discharged on the operation day. However, most patients want to be discharged on postoperative day one. That is one reason why the mean length of hospital stay is shorter when the local anesthesia method is used compared with spinal or general anesthesia.
Regarding medical costs, there are many reports about the cost-effectiveness of local anesthesia during hernia surgery in Western countries [19,20,21]. In our study, we found that the total mean ± standard deviation fee-for-service charge for the local anesthesia group was lower compared with the spinal anesthesia group (SA: 923,310 ± 269,847 Korean won [KRW] vs. LA: 786,963 ± 236,721 KRW, P < 0.001; Data not shown here).
Although local anesthesia is believed to be beneficial in many regards, some patient characteristics make it dangerous to perform; for example, if the patient has a lidocaine allergy, uncontrolled (no pacemaker) arrhythmias, psychological problems or fear of surgery or is too young to endure the surgical stress. Additionally, if strangulation is suspected or in some complicated cases, local anesthesia is not indicated.
As Amid et al. [22] has reported, bilateral inguinal hernia repair under local anesthesia is a safe procedure. In our study, there were 11 bilateral inguinal hernia cases in the LA group, and the mean operation time was 98.6 ± 13.5 minutes. This time was slightly longer than for unilateral repair (64.5 ± 17.6 minutes), but there were no intra- or postoperative complications in the bilateral inguinal hernia repair group.
Kehlet and Bay-Nielsen [23] reviewed the Danish Hernia Database of approximately 43,123 patients between 1998 and 2005. The data were analyzed in relation to the type of inguinal hernia and whether it was repaired in a public hospital or by private hernia surgeons. The use of local anesthesia was followed by higher reoperation rates compared with general or regional anesthesia after the repair of direct, but not indirect, hernias in hospitals. However, reoperation rates after both direct and indirect hernia repairs were lower among private hernia surgeons with the uniform use of local anesthesia compared with reoperations following primary surgery in hospitals. Thus, the authors concluded that surgical experience and hernia type may be important factors for reoperation independent of the type of anesthesia used. However, the authors mentioned that when inguinal hernia repair is performed in general hospitals, local anesthesia may be a risk factor for recurrence after the primary repair of a direct hernia. Although local anesthesia provides maximum comfort for the patients in selected institutions, its use may result in discomfort to the patient and surgeon when the procedure is not performed properly. Inexperience with the local anesthetic technique can cause both discomfort to patients and an increased recurrence rate.
These findings indicate that before selecting the type of anesthetic method to use for inguinal hernia repair, it is necessary to have more evidence about which type of hernia repair technique is safer, offers a lower recurrence rate and is less affected by surgical skill. With that information, we can apply the proper anesthetic technique to that surgery. Each surgical technique and anesthetic method may have its advantages and disadvantages.
In conclusion, if local anesthesia using TLA solution is used appropriately in open anterior inguinal hernia repair by a skilled surgeon, it may reduce operation time and hospital stay and decrease postoperative complications.
Figures and Tables
References
1. Farquharson EL. Early ambulation; with special reference to herniorrhaphy as an outpatient procedure. Lancet. 1955; 269:517–519.
2. Gultekin FA, Kurukahvecioglu O, Karamercan A, Ege B, Ersoy E, Tatlicioglu E. A prospective comparison of local and spinal anesthesia for inguinal hernia repair. Hernia. 2007; 11:153–156.
3. Sanjay P, Woodward A. Inguinal hernia repair: local or general anaesthesia? Ann R Coll Surg Engl. 2007; 89:497–503.
4. Amid PK, Shulman AG, Lichtenstein IL. Local anesthesia for inguinal hernia repair step-by-step procedure. Ann Surg. 1994; 220:735–737.
5. Welsh DR, Alexander MA. The Shouldice repair. Surg Clin North Am. 1993; 73:451–469.
6. Kark AE, Kurzer M, Waters KJ. Tension-free mesh hernia repair: review of 1098 cases using local anaesthesia in a day unit. Ann R Coll Surg Engl. 1995; 77:299–304.
7. Yang JH, Park SS, Yoon J, Kim IM. A comparison of three methods of hernioplasty for adult inguinal hernia: Bassini repair versus lichtenstein repair versus Mesh-Plug repair. J Korean Surg Soc. 2004; 67:314–319.
8. Min HS, Shin DW, Kim ID, Kim KH, Suh BS, Kim SW, et al. Comparison between lichtenstein and prolene hernia system (PHS) in anterior tension-free, inguinal & femoral hernioplasty. J Korean Surg Soc. 2006; 71:39–42.
9. Lee TG, Park JS, Lee SI, Choi YS, Park DJ, Han HS, et al. The state of patient satisfaction after hernioplasty on an ambulatory basis. J Korean Surg Soc. 2007; 73:53–59.
10. Kim HJ, Ryu HS, Hur YH, Kim JC, Kim SK, Park CY. Inguinal hernia repair under local anesthesia in octogenarians. J Korean Surg Soc. 2009; 77:338–343.
11. Lee WI, Kim HS, Ryu BY, Kim HK, Lee JW, Choi YH, et al. Clinical analysis of inguinal hernia in adult using prolene hernia system. J Korean Surg Soc. 2010; 79:137–142.
12. Callesen T, Bech K, Kehlet H. The feasibility, safety and cost of infiltration anaesthesia for hernia repair. Hvidovre Hospital Hernia Group. Anaesthesia. 1998; 53:31–35.
13. Lawrence K, McWhinnie D, Goodwin A, Gray A, Gordon J, Storie J, et al. An economic evaluation of laparoscopic versus open inguinal hernia repair. J Public Health Med. 1996; 18:41–48.
14. Nyhus LM, Condon RE. Hernia. 3rd ed. Philadelphia: Lippincott;1989.
15. Narita M, Sakano S, Okamoto S, Uemoto S, Yamamoto M. Tumescent local anesthesia in inguinal herniorrhaphy with a PROLENE hernia system: original technique and results. Am J Surg. 2009; 198:e27–e31.
16. Amid PK, Shulman AG, Lichtenstein IL. A five-step technique for local anesthesia in inguinal hernia repair. Chirurg. 1994; 65:388–390.
17. Kulacoglu H, Ergul Z, Esmer AF, Sen T, Akkaya T, Elhan A. Percutaneous ilioinguinal-iliohypogastric nerve block or step-by-step local infiltration anesthesia for inguinal hernia repair: what cadaveric dissection says. J Korean Surg Soc. 2011; 81:408–413.
18. Gultekin FA, Kurukahvecioglu O, Karamercan A, Ege B, Ersoy E, Tatlicioglu E. A prospective comparison of local and spinal anesthesia for inguinal hernia repair. Hernia. 2007; 11:153–156.
19. Fenoglio ME, Bermas HR, Haun WE, Moore JT. Inguinal hernia repair: results using an open preperitoneal approach. Hernia. 2005; 9:160–161.
20. Nordin P, Zetterstrom H, Carlsson P, Nilsson E. Cost-effectiveness analysis of local, regional and general anaesthesia for inguinal hernia repair using data from a randomized clinical trial. Br J Surg. 2007; 94:500–505.
21. Liem MS, Halsema JA, van der, Schrijvers AJ, van Vroonhoven TJ. Cost-effectiveness of extraperitoneal laparoscopic inguinal hernia repair: a randomized comparison with conventional herniorrhaphy. Coala trial group. Ann Surg. 1997; 226:668–675.
22. Amid PK, Shulman AG, Lichtenstein IL. Simultaneous repair of bilateral inguinal hernias under local anesthesia. Ann Surg. 1996; 223:249–252.
23. Kehlet H, Bay-Nielsen M. Local anaesthesia as a risk factor for recurrence after groin hernia repair. Hernia. 2008; 12:507–509.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download