Abstract
Purpose
Surgical site infection (SSI) after open abdominal surgery is still a frequently reported nosocomial infection. To reduce the incidence of SSI, triclosan-coated sutures with antiseptic activity (Vicryl Plus) were developed. The aim of this study was to analyze the effect of Vicryl Plus on SSI after gastric cancer surgery via midline laparotomy.
Methods
A total of 916 patients who underwent gastric cancer surgery at Samsung Medical Center between December 2009 and September 2011 were prospectively collected. We examined the occurrence of SSI (primary endpoint), assessments of wound healing (secondary endpoint). They were evaluated postoperatively on days 3, 7, and 30.
Results
Of the 916 patients, 122 were excluded postoperatively by screening (out of the study protocol, adverse events, etc.). The remaining 794 patients were enrolled and monitored postoperatively. The cumulative SSI incidence was 11 cases (1.39%; 95% confidence interval [CI], 0.77-2.50) on day 30. Seromas were most frequently detected in wound healing assessments, with a cumulative incidence of 147 cases (18.51%; 95% CI, 15.98-21.39) on day 30.
Surgical site infection (SSI) is still a frequent type of nosocomial infection, accounting for about 15% of the total number of nosocomial infections [1]. More specifically, it is reported that 4%-17% of midline laparotomy patients suffer from SSI [2,3]. Although many people underestimate SSI as something of minimal importance during wound healing, SSI may generate psychological, physical and financial stress to patients, and in some cases, even pose as a threat to their lives [4,5]. There have been strong efforts to reduce the rate of SSI. One of the major breakthroughs in SSI research is the appropriate use of antibiotics before and after operation [6]. As the use of prophylactic antibiotics has recently been proven to be effective in preventing SSI, these drugs are widely and increasingly used, and have contributed to decreasing the incidence of SSI along with the help of improved medical technology [7]. Despite the reduced rate of SSIs thanks to the proper utilization of antibiotics, many patients still suffer from SSIs. In recent years, in attempts to further reduce SSIs, researchers took a topical approach with a new focus on incisions. As most postoperative SSIs occur in incised areas [5], there have been several studies on using sutures coated with antibiotic materials. As a result, a triclosan-coated suture (Vicryl Plus, Ethicon Inc., Somerville, NJ, USA), which is antibacterial, was developed. Although the antibiotic effect of Vicryl Plus has been reported and recognized through in vitro experiments and animal testing [8,9], research studies involving human subjects have not been sufficient to make a case. Past studies with humans have mostly investigated different types of operations or involved a small number of subjects, making them insufficient to prove the efficacy of the sutures [10,11,12].
Gastric cancer surgery is one of the most frequently performed surgeries in Korea [13]. According to the classification of surgery wounds from the US Centers for Disease Control and Prevention (CDC), gastric cancer surgery falls into class II (clean-contaminated). In typical class II surgeries, SSI rates are reportedly 5%-15% [5,6]. In the case of a planned and prepared gastrectomy (i.e., laparotomy), the rate remarkably drops to lower than 5%. However, for cancer patients who suffer from SSIs, the infection can cause them more serious psychological and financial damage than it does to patients with other diseases, and can delay postoperative adjuvant therapy, bringing deadly outcomes to patients.
In this light, researchers of this study took an objective approach to find the efficacy of triclosan-coated sutures in SSI after gastric cancer surgery via midline laparotomy, a commonly performed procedure in Korea.
This prospective study enrolled a total of 916 patients who underwent curative radical gastrectomy for the treatment of gastric cancer at the Samsung Medical Center from December 2009 to September 2011. The number of target subjects was calculated based on the data released by the Korean Nosocomial Infection Surveillance System (KONIS); the overall rate of SSI in gastric surgery was about 4% according to the data [14]. The SSI rate of equivalence was expected on postoperative day 30, and the sample size of 825 patients was calculated with ±1.4% width of 95% confidence interval (CI). This number was increased to 916 patients in this study, taking into account an estimated rate of 10% loss of patients in screening.
Surgeries were performed by five experienced surgeons, who reached an agreement (protocol) on how to suture the abdominal wound. SSIs were detected through surveillance until day 30. The study was deliberated by the executive office of Institutional Review Board of Samsung Medical Center. All subjects participated in the study with prior written consent. Patients 18 years of age or older who were planning to receive surgery after being diagnosed with gastric cancer were eligible for enrollment. All patients were treated in compliance with the critical pathway (CP) of the hospital before and after the operation. According to the standards of the CP, patients received bowel preparation on the last day before the operation and were administered prophylactic antibiotics on the day of the operation and the next day after the operation. Cafotetan-the 2nd generation cephalosporin-was used as the prophylactic antibiotic. It was only injected once within one hour and once within 24 hours after the operation, in accordance with the guidelines of the US National Surgical Infection Prevention.
The following cases were excluded from the study: (1) patients with wounds infected before the operation; (2) those who had to take other antibiotics during the follow-up period; (3) those with systemic diseases which might interfere with the clinician's judgment of the results of the clinical study (American Society of Anesthesiologists [ASA] score > 3); (4) those who were difficult to follow up; (5) those with a past medical history of abdominal surgery; and (6) those in whom the abdominal wound was closed by a different method other than the agreed technique.
Prophylactic antibiotics were administered to all patients within one hour after the start of the operation. Surgical areas were shaved just before the operation only in required cases and were aseptically scrubbed with chlorhexidine (5%, soap). For the skin, an upper midline laparotomy was made with a scalpel, and the other layers down to the peritoneal cavity were incised by diathermy. During gastric cancer surgery, gentle handling was needed to prevent wounds from being infected by bowel contents. Triclosan-coated sutures (Vicryl Plus) were used to close the wound by a two-layer and a continuous technique. In doing so, interrupted sutures at the intervals of 3 to 5 cm helped to prevent continuous sutures from being weakened or from breaking. The skin, after stapling, was covered with an aseptic dressing. Prophylactic antibiotics were administered once more within 24 hours after the completion of surgery, while analgesics by intravenous injection were administered for a few days to reduce pain in the surgical area.
While patient-related factors including age, sex, weight, body mass index (BMI), smoking history, and underlying diseases were collected from past medical records or questionnaires during the preoperative period, surgery-related factors such as length of surgery, periods of hospitalization, SSI occurrence, and assessments of wound healing were collected prospectively.
By definition, SSI is a type of infection that occurs in the surgical site within 30 days after operation or within one year if an implant is in place; SSI categorizes the infection into three groups (superficial and deep incisional SSIs and organspace SSI) according to the information from the US CDC [5]. The definition and classification of SSI are shown in Table 1. Patients in the present study were followed up postoperatively and observed up to day 30. In cases of poorly healed wounds and the presence of discharge for a long period, or in cases when proper antibiotics should have been used for treatment, bacterial cultivation was chosen. One of the major risk factors of SSIs is the National Nosocomial Infections Surveillance (NNIS) system risk index score. This index, which was developed by the CDC, predicts and scores the SSI risk for each type of surgery [15]. One point is given each to the case of an ASA score higher than 3, the case of wound class III and IV, and the case of surgery time longer than the standard time (T) for the type of surgery, making the total score in the range from 0 to 3. Standard surgery time is calculated based on the 75th percentile of the length of surgeries surveyed by NNIS for each type of surgery. For gastric surgery, the standard time is three hours. In this study, ASA scores ranged from 1 to 2, and all of patients fell into wound class II. Therefore, the NNIS risk index score was determined as either 0 or 1 in this cohort of patients.
For assessments of wound healing, the clinicians postoperatively evaluated erythema, edema, wound dehiscence, seroma, pus discharge, local heating and tenderness, which were recorded on each of the case report forms (answered with either "yes" or "no"). These results were reaffirmed by other surgeons to give objectivity.
The occurrence of SSI and assessments of wound healing were evaluated postoperatively by the clinicians and patients for a total of three times (on days 3, 7, and 30). Evaluation was made during hospitalization on days 3 and 7, and as an outpatient on day 30.
For the primary endpoint, we examined SSI rates up to day 30 after the operation. Evaluation was made under the categories of superficial and deep incisional SSIs and organspace SSI depending on the site and the extent of infection. When superficial and deep incisional SSIs were found together, they were categorized under deep incisional SSI. Thus, we postoperatively examined the number of infected patients and accumulated infection rates on days 3, 7, and 30 according to the SSI categorization. We also checked how the infected group and the noninfected group were associated with age, BMI, smoking history, existence of comorbidity, operation time, and length of hospital stay. As for the secondary endpoint, we examined the assessments of wound healing up to day 30 after the operation. For each variable of wound healing, frequency and accumulative rates were evaluated.
For the subjects who were eliminated during the study, the Kaplan-Meier product limit method was used to calculate SSI rates and occurrence rates of wound healing variables. The cumulative occurrence rates until day 30 and 95% CI were calculated. In order to make comparisons between the group with infection and the group without infection, the Mann-Whitney test was applied for continuous variables, and the Fisher exact test for categorical variables. IBM SPSS Statistics ver. 20.0 (IBM Co., Armonk, NY, USA) was used for data analysis, and a significance level of 0.05 was used.
The intention and purpose of this study were explained to the patients scheduled for gastric cancer surgery. The patients who voluntarily agreed to participate were collected for the study. Of the 916 patients, 122 were excluded by screening, and the remaining 794 patients were enrolled in the study. During postoperative surveillance on days 3, 7, and 30, eight patients dropped out (Table 2, Fig. 1).
SSIs started to occur after postoperative day 3, and the cumulative number of infected patients until day 30 was 11. Out of the 11 patients, the numbers for the categories of superficial and deep incisional SSIs and organ-space SSI were 8, 2, and 1, respectively. In terms of surgery time of each category, there was no apparent association with infection, while the length of hospitalization was found to be longer in the infected group (Table 3). The cumulative infection rates for the superficial and deep incisional SSIs and organ-space SSIs were 1.01%, 0.25%, and 0.13%, respectively. Therefore, the total cumulative infection rate was 1.39% (95% CI, 0.77-2.50) (Table 4). Most of the ten patients with superficial and deep incisional SSIs were clinically diagnosed as they exhibited symptoms including pus, erythema, pain and fever. Meanwhile, one patient with organspace SSI was diagnosed by computerized tomography as the patient was suspected of intra-abdominal infection through the surgical site. Bacteria were cultivated from four patients among those with SSIs. As a result, causative organisms were isolated from two patients. Most patients improved through conservative treatment, while two patients with deep incisional SSI improved after second surgery for fascial defect.
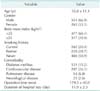
After examining whether the groups with and without infection were associated with demographic and clinical factors, we found no statistical significance with age, BMI, smoking history, existence of comorbidity, operation time and NNIS risk factors, while there was a significant difference with the length of hospital stay (16.6 ± 7.1 days vs. 11.8 ± 2.1 days, P = 0.004) (Table 5).
For the postoperative evaluation of wound healing until day 30, seroma occurred most frequently in 147 patients, with a cumulative occurrence rate of 18.51% (95% CI, 15.98-21.39), and tenderness (12.10%), erythema (6.42%) and wound dehiscence (4.91%) followed in decreasing order. Purulent discharge had the lowest rate with six patients (0.76%) (Table 6). For most variables, the occurrence rate changed between day 3 and day 7 after the operation, while showing no distinct difference between day 7 and day 30. Each wound healing assessment alone had no direct association with actual cases of SSI occurrence, except for purulent discharge. In patients suspected of SSI with signs such as tenderness, edema, erythema, or heating, the surgeons temporarily opened the incised area to check whether it was true or not. In those cases, most patients had noninfective fluid such as seroma or fat necrosis.
In this clinical study, a total of eight patients (0.87%) had adverse symptoms, four in postoperative day 3 and four during the surveillance period between day 3 and day 30, and they dropped-out from the study. These eight subjects required other antibiotics and additional treatment due to significant adverse symptoms, and had to be hospitalized for a longer time. Of the eight patients, six had respiratory problems such as atelectasis, pleural effusion and pneumonia, while two had noncomplicated fluid collection in the intra-abdominal cavity after the operation. However, all of these symptoms were caused by general anesthesia or gastrectomy. No symptom was directly related to triclosan-coated sutures.
Poor wound healing and SSI are among the most common complications of laparotomy. These are critical issues, as they not only increase medical costs due to the need of additional wound healing and antibiotics along with longer hospitalization, but also result in higher morbidity rates and death rates for high-risk patients [4,16]. In this regard, the focus of the present study was on the effect of triclosan-coated suture (Vicryl Plus) on SSIs and wound healing when it was used for abdominal suturing in gastric cancer surgery.
SSI is influenced by many intrinsic and extrinsic factors [4,5,15]. Patient related factors include age, sex, BMI, existence of comorbidity, medical history and habits (e.g., smoking). In addition, factors regarding surgery are depilation, skin sterilization, ventilation of the operation room, operation time, refined and aseptic operative techniques, and the proper use of antibiotics. As it is difficult to modify or standardize patient-related factors, past clinical studies on how to reduce SSIs have mainly been focused on surgery-related factors. One of the most frequently used methods involves the use of triclosan-coated sutures. There have been studies on sutures and SSI occurrence over the past several years. Sutures are known to increase the susceptibility of organs to infection and carry bacteria to surgical areas [17,18]. In other words, if bacteria, that are attached to the surface of the suture, first cause contamination, the local defense mechanisms of the surgical area will break down [19]. Precisely speaking, it is not the suture that causes infection. However, as bacteria can gather and proliferate on the suture, even a small number of bacteria on the suture is capable of causing infection [20]. For this reason, studies on antimicrobial sutures have been done in an effort to prevent sutures from causing infection. The study on the effect of triclosan-coated sutures on infections through in vitro experiements and animal testing found that triclosan-coated sutures were very effective in preventing bacteria from attaching to the suture [8,18]. Also, some recent clinical studies have reported that the antimicrobial coating of the suture helped to reduce postoperative inflammatory reactions and assisted in the wound healing process [21].
This study was an investigator-driven prospective study, performed at a single center-Samsung Medical Center. Accordingly, every process starting from collection of patients and surgery to pre- and postoperative procedures was compiled with the protocol to obtain more objective SSI rates for the use of triclosan-coated sutures in midline laparotomy. As all the study participants were diagnosed with the same disease-gastric cancer-and had the NNIS risk index score in the range from 0 to 1, confounding variables were kept to a minimum in this study, which gave more reliability to the results of the SSI rates. Past studies indicated that SSIs increased the rate of morbidity, the length of hospitalization and, consequently, economic damages [16,22]. In this study, the increase of the length of hospitalization was found to be statistically significant in the group with infection and thought to result in financial losses. Not only that, but hospitals will have a lower inpatient turnover ratio and patients will lose working days (decreased productivity). So consequently, massive additional social costs can be incurred because of SSIs.
Although purulent drainage, bacterial culture and signs of infection (fever, pain or tenderness, swelling, redness and heating sense) are important in making a diagnosis of SSI, perceptive and accurate observation of them by a clinician is crucial. Therefore, diagnoses of SSI were reconfirmed by two more clinicians when it was uncertain. The results of this study indicated that the only single assessment (erythema, edema, wound dehiscence, seroma, local heating, and tenderness) had no direct association with SSIs, except for purulent discharge. As diagnosis by a clinician appears to be critical, surgeons should have enough knowledge and experience to be able to detect SSIs correctly. As a result of this study, because most SSIs were superficial and occurred between day 3 and day 7 after surgery, early detection and treatment of SSIs are considered really important.
This prospective study had certain limitations. The biggest limitation is the one-armed study design. Nevertheless, our results are still significant as a preliminary study revealing that SSI rates using triclosan-coated sutures were greatly decreased to 1.39% in gastric cancer patients, compared with the historical data. Although this study can be shown to have better results than other studies due to low NNIS risk index scores of enrolled patients, the results of this study appear to be encouraging, especially when compared to the national reports such as NNIS and KONIS, in which the SSI rates of gastric surgery ranged from about 2.5% to 6.4% in the same NNIS scores [14,15]. Another limitation was the relatively small number of patients with infection, compared to the number of patients without infection, which made it difficult to perform a statistical analysis. Also, because the study relied too much on clinical diagnosis in patients with infection or those suspected of infection, the frequency of bacterial cultivation was low, and thus objective data from analysis of causative organisms, for example, were not sufficiently obtained. Although there are the aforementioned limitations in our study, those results are considered reliable and valuable because of the standardization of diseases and operative procedures in a relatively large number of patients together with the prospective trial.
We believe that this study presented an achievement by confirming that the use of triclosan-coated sutures (Vicryl Plus) in midline laparotomy can reduce SSIs. Triclosan-coated sutures may be one of the most effective antimicrobial agents developed to date and they are expected to greatly contribute to decreasing SSIs if combined with refined and aseptic surgery techniques and the proper use of prophylactic antibiotics. Furthermore, more studies are required to find the exact mechanisms between sutures and wound healing. Also, a wider range of studies on sutures will be needed due to the possibility of emergence of antimicrobial resistant bacteria in the future.
In summary, this study shows that the use of triclosan-coated sutures for abdominal wall closure can reduce the number of SSIs in gastric cancer surgery. This might help to decrease the length of hospital stay for patients undergoing gastric cancer surgery.
Figures and Tables
Table 3
Frequency of surgical site infection and clinical data, according to type of infection (n = 794)

Table 4
Cumulative surgical site infection rates during follow-up period, according to type of infection (n = 794)
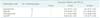
Table 5
Comparable data between infected and noninfected group

Values are presented as mean ± standard deviation or number (%).
T75, 75th percentile of the average duration for the procedure, 3 hours for gastric surgery; NNIS, National Nosocomial infections Surveillance System.
a)Comorbidity includes one or more of the diabetes, cardiovascular, and pulmonary disease. b)Duration of operation > T75 means
NNIS risk index is one point. c)P-values are based on the Fisher exact test or Mann-Whitney test.
References
1. Emori TG, Gaynes RP. An overview of nosocomial infections, including the role of the microbiology laboratory. Clin Microbiol Rev. 1993; 6:428–442.
2. Israelsson LA, Jonsson T, Knutsson A. Suture technique and wound healing in midline laparotomy incisions. Eur J Surg. 1996; 162:605–609.
3. Franchi M, Ghezzi F, Benedetti-Panici PL, Melpignano M, Fallo L, Tateo S, et al. A multicentre collaborative study on the use of cold scalpel and electrocautery for midline abdominal incision. Am J Surg. 2001; 181:128–132.
4. Engemann JJ, Carmeli Y, Cosgrove SE, Fowler VG, Bronstein MZ, Trivette SL, et al. Adverse clinical and economic outcomes attributable to methicillin resistance among patients with Staphylococcus aureus surgical site infection. Clin Infect Dis. 2003; 36:592–598.
5. Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR. Guideline for Prevention of Surgical Site Infection, 1999. Centers for Disease Control and Prevention (CDC) Hospital Infection Control Practices Advisory Committee. Am J Infect Control. 1999; 27:97–132.
6. Nichols RL. Preventing surgical site infections. Clin Med Res. 2004; 2:115–118.
7. Bratzler DW, Houck PM, Richards C, Steele L, Dellinger EP, Fry DE, et al. Use of antimicrobial prophylaxis for major surgery: baseline results from the National Surgical Infection Prevention Project. Arch Surg. 2005; 140:174–182.
8. Rothenburger S, Spangler D, Bhende S, Burkley D. In vitro antimicrobial evaluation of Coated VICRYL* Plus Antibacterial Suture (coated polyglactin 910 with triclosan) using zone of inhibition assays. Surg Infect (Larchmt). 2002; 3:Suppl 1. S79–S87.
9. Gomez-Alonso A, Garcia-Criado FJ, Parreno-Manchado FC, García-Sanchez JE, García-Sanchez E, Parreno-Manchado A, et al. Study of the efficacy of Coated VICRYL Plus Antibacterial suture (coated Polyglactin 910 suture with Triclosan) in two animal models of general surgery. J Infect. 2007; 54:82–88.
10. Mingmalairak C, Ungbhakorn P, Paocharoen V. Efficacy of antimicrobial coating suture coated polyglactin 910 with tricosan (Vicryl plus) compared with polyglactin 910 (Vicryl) in reduced surgical site infection of appendicitis, double blind randomized control trial, preliminary safety report. J Med Assoc Thai. 2009; 92:770–775.
11. Justinger C, Schuld J, Sperling J, Kollmar O, Richter S, Schilling MK. Triclosan-coated sutures reduce wound infections after hepatobiliary surgery--a prospective non-randomized clinical pathway driven study. Langenbecks Arch Surg. 2011; 396:845–850.
12. Justinger C, Moussavian MR, Schlueter C, Kopp B, Kollmar O, Schilling MK. Antibacterial [corrected] coating of abdominal closure sutures and wound infection. Surgery. 2009; 145:330–334.
13. National Health Insurance Corporation. Statistics on major surgical procedures in Korea, 2009 [Internet]. Seoul: National Health Insurance Corporation;c2011. cited 2010 Dec 24. Available from: http://www.nhic.or.kr.
14. Kim ES, Kim HB, Song KH, Kim YK, Kim HH, Jin HY, et al. Prospective nationwide surveillance of surgical site infections after gastric surgery and risk factor analysis in the Korean Nosocomial Infections Surveillance System (KONIS). Infect Control Hosp Epidemiol. 2012; 33:572–580.
15. National Nosocomial Infections Surveillance System. National Nosocomial Infections Surveillance (NNIS) System Report, data summary from January 1992 through June 2004, issued October 2004. Am J Infect Control. 2004; 32:470–485.
16. Galal I, El-Hindawy K. Impact of using triclosan-antibacterial sutures on incidence of surgical site infection. Am J Surg. 2011; 202:133–138.
17. Katz S, Izhar M, Mirelman D. Bacterial adherence to surgical sutures. A possible factor in suture induced infection. Ann Surg. 1981; 194:35–41.
18. Edmiston CE, Seabrook GR, Goheen MP, Krepel CJ, Johnson CP, Lewis BD, et al. Bacterial adherence to surgical sutures: can antibacterial-coated sutures reduce the risk of microbial contamination? J Am Coll Surg. 2006; 203:481–489.
19. Uff CR, Scott AD, Pockley AG, Phillips RK. Influence of soluble suture factors on in vitro macrophage function. Biomaterials. 1995; 16:355–360.
20. Fiss EM, Rule KL, Vikesland PJ. Formation of chloroform and other chlorinated byproducts by chlorination of triclosancontaining antibacterial products. Environ Sci Technol. 2007; 41:2387–2394.
21. Rasic Z, Schwarz D, Adam VN, Sever M, Lojo N, Rasic D, et al. Efficacy of antimicrobial triclosan-coated polyglactin 910 (Vicryl* Plus) suture for closure of the abdominal wall after colorectal surgery. Coll Antropol. 2011; 35:439–443.
22. Zhan C, Miller MR. Excess length of stay, charges, and mortality attributable to medical injuries during hospitalization. JAMA. 2003; 290:1868–1874.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download