Abstract
Polyarteritis nodosa (PAN) is a systemic necrotizing vasculitis of small- and medium-sized arteries in multiorgan systems. PAN may affect the gastrointestinal tract in 14%-65% of patients, but rarely involves the biliary tract and liver. We describe a patient without underlying disease who was diagnosed with PAN during resection of the gallbladder and liver.
Polyarteritis nodosa (PAN) is a systemic vasculitis that commonly involves the skin, kidneys, nerves, and gastrointestinal tract. The clinical presentation of PAN commonly consists of symptoms arising from affected organs [1]. However, there are no diagnostic serologic tests; consequently, the diagnosis of PAN is based on specific histologic studies of biopsied organs. Although there are reports of gallbladder involvement, intrahepatic biliary duct involvement is rarely reported [2]. We report the case of a patient presenting with left intrahepatic duct dilatation with hepatolithiasis, as detected on abdominal CT without evidence of systemic disease, diagnosed histologically with PAN.
A 53-year-old man presented with poor oral intake for a month, and a fever that had lasted for 5 days. His medical history consisted of a local hospital admission 5 days previous due to cholangitis with associated fever. Treatment consisted of antibiotics; an abdominal ultrasonography showed left intrahepatic duct dilatation. When the patient presented at the hospital, he had no abnormal findings on serologic and immunologic tests. In addition, tumor markers-CEA and CA 19-9 were negative. He did not have a history of hepatitis B or C. Abdominal CT scan and magnetic resonance cholangiopancreatography were requested to investigate hepatobiliary abnormalities. The investigations demonstrated focal dilatations of the left intrahepatic duct with narrowing suggesting a biliary stricture, cholangiocarcinoma or chronic cholecystitis (Figs. 1, 2). After a trial of conservative care, which included nutritional support and antibiotics, he underwent a laparotomy (left hepatectomy and cholecystectomy) for diagnostic and therapeutic purposes. The resected liver showed intrahepatic duct dilatation with hepatolithiasis without any evidence of cancer. During the postoperative recovery period, the patient complained of progressively worsening foot numbness. In addition, the final pathology report of the resected liver and gallbladder noted transmural inflammation and fibrosis in small-to-medium sized arteries (Figs. 3, 4), and transmural infiltration in the small artery by mononuclear cells, neutrophils, and eosinophils, accompanied by fibrinoid necrosis; all consistent with PAN (Fig. 5). The patient was transferred to rheumatology and treated with prednisolone. Thereafter, the foot numbness disappeared and prednisolone maintenance therapy was continued. Following discharge, the patient was transferred to the rheumatology department's outpatient care.
PAN is a systemic necrotizing vasculitis of small- and medium-sized arteries in multiple organ systems, but is rare. Deposition of antigen-antibody complexes in the vessel walls leads to inflammation, edema and eventually necrosis of the tunica intima and media. It is characterized by fibrinoid necrosis and predominant polymorphonuclear leukocyte infiltration [3]. PAN may affect several organs such as the skin, kidneys, nervous system, and gastrointestinal tract. Gastrointestinal involvement occurs in 14%-65% of patients with PAN, where in the small bowel or gallbladder is most commonly affected. Among them, liver involvement occurs in 16%-56% of patients [2]. Symptoms of PAN depend on the extent of organ involvement. For example, symptoms of PAN in the liver range from no symptoms to aggressive manifestations. Signs and symptoms include cirrhosis, hepatitis, ruptured aneurysm, hepatic failure, and nodular hyperplasia of the liver [4,5]. Hence the diagnosis of liver involvement is very difficult because there are no significant clinical manifestations or known markers. Although some reports suggest hepatic arteriography and hepatobiliary scintigraphy, for diagnosis, tissue biopsies of involved organs and histologic examination are usually needed to confirm the diagnosis of PAN [6]. There are many reports of PAN diagnosed during surgery for conditions such as acalculous cholecystitis, cirrhosis, and hepatic cystic lesions. However, to the authors' knowledge, there is no report of PAN diagnosed through hepatectomy for hepatolithiasis. In our case, the patient presented with dilatation of intrahepatic bile duct associated with hepatolithiasis. The patient's symptoms did not suggest PAN, while abnormal immunologic and serologic tests did. We therefore performed hepatectomy to differentiate cholangiocarcinoma. During the postoperative period, the patient complained of progressively worsening foot numbness. We attempted to find the cause of the patient's neurological symptoms, and ultimately diagnosed the patient with neurological involvement of PAN based on the pathology of the resected liver that was compatible with a diagnosis of PAN. In conclusion, health care providers should consider PAN in patients who have no underlying disease or risk factors for hepatolithiasis
Figures and Tables
Fig. 1
Contrast enhanced abdominal CT shows focal left intrahepatic duct dilatation with some narrowing portions (arrows).
Fig. 2
(A) T2-weighted magnetic resonance image shows focal left intrahepatic duct dilatation. (B) Enhanced T1-weighted magnetic resonance image showed no abnormal enhanced lesion in liver. (C) Magnetic resonance cholangiopancreatography shows focal left intrahepatic duct dilatation with luminal narrowing (white arrows).

Fig. 3
A large portal tract expanded with distended bile ducts due to hepatolithiasis. Shown above are small-to-medium sized arteries with transmural inflammation and/or transmural fibrosis (arrows) (H&E, ×10).

Fig. 4
In this microphotograph, one small artery shows transmural inflammation (A) and one medium artery shows transmural fibrosis with thickening of the wall (B). All other arteries are normal in appearance (H&E, ×40).
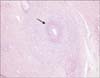
Fig. 5
At higher magnification of Fig. 2A, transmural infiltration of small artery by mononuclear cells, neutrophils, and eosinophils is accompanied by fibrinoid necrosis (arrow) (H&E, ×200).
References
1. Parangi S, Oz MC, Blume RS, Bixon R, Laffey KJ, Perzin KH, et al. Hepatobiliary complications of polyarteritis nodosa. Arch Surg. 1991; 126:909–912.
2. Ebert EC, Hagspiel KD, Nagar M, Schlesinger N. Gastrointestinal involvement in polyarteritis nodosa. Clin Gastroenterol Hepatol. 2008; 6:960–966.
3. Lightfoot RW Jr, Michel BA, Bloch DA, Hunder GG, Zvaifler NJ, McShane DJ, et al. The American College of Rheumatology 1990 criteria for the classification of polyarteritis nodosa. Arthritis Rheum. 1990; 33:1088–1093.
4. Guma M, Lorenzo-Zuniga V, Olive A, Perendreu J, Bechini J, Domenech E, et al. Occult liver involvement by polyarteritis nodosa. Clin Rheumatol. 2002; 21:184–186.
5. Abraham S, Begum S, Isenberg D. Hepatic manifestations of autoimmune rheumatic diseases. Ann Rheum Dis. 2004; 63:123–129.
6. Kitzing B, O'Toole S, Waugh A, Clayton J, McGill N, Allman KC. Hepatobiliary scintigraphy in vasculitis of the gallbladder as a manifestation of polyarteritis nodosa: a case report. Cases J. 2009; 2:9300.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download