Abstract
Purpose
The use of abdominal computed tomography (ACT) utilization is increasing to a remarkable extent in the pediatric Emergency Department (ED), but the clinical benefit of increased use of ACT for pediatric surgical patients remains uncertain.
Methods
A retrospective review was conducted to investigate if, for patients who had visited pediatric ED during the last 5 years, increasing utilization of ACT would increase the detection rate of acute appendicitis, increase the detection rate of surgical conditions other than appendicitis, and decrease the hospital admission rate for surgical conditions.
Results
During the study period, there were 37,918 ED visits; of these, 3,274 (8.6%) were for abdominal pain, 844 (2.2%) had ACT performed. The annual proportional increase of the ACT was statistically significant (1.56% to 2.46%, P = 0.00), but the detection rate of acute appendicitis (3.3% to 5.1%) or other surgical conditions (1.7% to 2.8%) showed no statistically significant changes. Hospital admission rates (5.6% to 6.8%) also showed no significant changes during the study period.
Due to its convenience, readiness, and diagnostic accuracy, abdominal computed tomography (ACT) is now becoming the most important diagnostic imaging modality for traumatic or nontraumatic abdominal pain in the adult Emergency Department (ED) [1]. In the pediatric ED, the amount of ACT utilization is also increasing, although the increase is not as pronounced as in the adult ED [2,3]. However, for acute appendicitis, which is the most common and important surgical condition seen in the pediatric ED, it has been proved that increasing the utilization of ACT neither decreases the negative appendectomy rate nor decreases the perforation rate [4,5,6]. Moreover, it is unclear whether increasing ACT use among undifferentiated pediatric patients with abdominal pain results in improved healthcare delivery. Therefore, we need a more concrete scientific basis to support the practice of increasing the utilization of ACT in the pediatric population despite the increased risk of radiation exposure, or we must balance the benefit of CT with the risk of radiation exposure.
Using acute appendicitis as an index disease in the pediatric ED, with other surgical conditions as supplements, we posed three questions to verify the relationship between the increasing utilization of ACT in the pediatric ED and outcomes in caring for pediatric surgical patients.
(1) Does increasing utilization of ACT increase the detection rate of acute appendicitis?
(2) Does increasing utilization of ACT increase the detection rate of surgical conditions other than appendicitis?
(3) Does increasing utilization of ACT decrease the overall admission rate for surgical conditions?
Between January 2009 and December 2013, the medical records of patients aged 18 or below who underwent ACT in the pediatric ED were reviewed retrospectively. Annual visits to the ED, annual visits for abdominal pain over the same period were also checked and the annual rate and trends of ACT were measured. Patients were classified into four groups according to the results of ACT: group 1, no abnormal findings; group 2, consistent with or suspicion of acute appendicitis; group 3, surgical conditions other than appendicitis; group 4, medical conditions. The clinical impression of each patient before the ACT was categorized as an acute appendicitis or not. ACTs performed under the clinical impression of acute appendicitis were also divided into the same four groups. The detection rate of acute appendicitis was determined by the rate of pathologically-proven appendicitis over the number of ED visits for abdominal pain. Surgical conditions other than appendicitis were defined as conditions which mandated prompt operative management or conditions referred to pediatric surgeons for clinical decision-making. The detection rate of group 3 patients was determined by the number of patients with surgical conditions other than appendicitis over the number of ED visits for abdominal pain. The admission rate was determined by confirming the final health status of the patients after ED evaluation. To control selection bias, patients who underwent ultrasonography (USG) at the ED for the same period were also reviewed. All statistical comparisons were made using the chi-square test and the significance was assigned for all at P < 0.05.
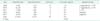
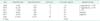
Overall, 844 ACTs were performed on 3,274 visits for abdominal pain during total 37,918 ED visits over the study period. Compared to the increase of total ED visits, the annual proportional increase of the ACT outpaced that of ED visits for abdominal pain, and the increase was statistically significant (trend P = 0.464 vs. trend P = 0.000, respectively) (Table 1). During the same period, 18 USGs were performed for the same population, and the annual decrease was statistically significant (P = 0.001) (Table 2). Of the 844 ACTs, male patients were 428 (50.7%) and female patients were 416 (49.3%), and mean age at presentation to ED was 12.8 years (range, 7 months-18 years). Normal ACTs comprised the largest portion (group 1), followed by various medical conditions (group 4) and acute appendicitis (group 2). Of the 66 surgical conditions other than appendicitis (group 3), traumatic solid organ injury and ovarian cystic complications comprised over the half of the cases. Among the 66 patients who had surgical conditions other than appendicitis, 14 patients (21.2%) underwent urgent invasive intervention and the remaining patients were managed with observation or planned operation. For ACTs performed under the impression of appendicitis (n = 591), normal findings or various medical conditions comprised over the half of the cases. Details on the patient demographics are listed in Table 3.
Our data showed that the annual increase in ACT was most pronouncedly influenced by the ACTs taken under the clinical impression of acute appendicitis. Nonetheless, the detection rate against the number of visits for abdominal pain showed no significant increase, reaching a peak in 2011 at 6.5% and declining since then to 5.1% in 2013 (P = 0.126). Our data does not support that increasing utilization of ACT increases the detection rate of acute appendicitis.
The incidence of surgical conditions other than appendicitis increased nearly three folds during the study period, but the detection rate remained steady at near 2% during the same period except in 2013. Statistically, however, the annual detection rate remained unchanged (P = 0.083). Our data does not support that increasing utilization of ACT increases the detection rate of surgical conditions other than acute appendicitis.
The admission for overall surgical conditions, including acute appendicitis, increased two folds during the study period, and the admission rate showed somewhat of a decrease after 2011, from 8.3% at 2011 to 6.8% at 2013. However, these changes had no statistical significance (P = 0.311). Our data does not support that increasing utilization of ACT decreases the admission rate for overall surgical conditions.
The detailed data pertaining to the questions above are summarized in Table 4.
Regarding the increasing utilization of ACT and surgical outcomes in the pediatric ED, this study aimed at investigating some questions which it appeared would give obvious and straightforward answers. However, this was not the case. The answers implied that great majority of ACTs performed in pediatric ED, in fact, add little clinical benefit and rather impose a burden of radiation hazard, which could otherwise be avoided. The pediatric population is more sensitive than the adult population to the harmful effects of radiation, and Brenner et al. [7] has estimated that, in approximately 600,000 abdominal and head CT performed per year in children, 500 of these children would ultimately die from radiation-induced cancer. The potential cancer risk persists into adulthood, declining to an "adult plateau" at approximately the age of 35 years. Many factors have been known to contribute to the overutilization of CT in the pediatric ED despite this overt risk; these include physicians' lack of awareness of radiation hazard in relatively bigger children, diagnostic requests from consultants in an effort to expedite care, and an absence of clinical decision rules (CDRs) [8,9,10]. In addition to these factors, we can speculate as to other factors which would contribute to the increasing utilization of ACT in our center. Unlike many tertiary care centers where a large proportion of patients visit the ED with diagnosis already confirmed at a low-level care center, most of the visits to secondary care centers are new patients and require primary evaluation including blood tests and radiological evaluations. These characteristics of secondary care centers might have contributed to the relatively high rate of ACT in our center, averaging about 2.5%, compared to that of tertiary care centers which average near 1.7% [3]. The recent dramatic increase in pediatric ED visits might also have contributed to the overutilization of ACT, by compelling ED physicians to rely on CT evaluation to expedite patient care.
As mentioned earlier in this paper, the negative appendectomy rate or complicated appendicitis rate has not changed after increased use of CT scanning, and although not included here, our data also showed the same results. Instead, we measured the detection rate of acute appendicitis to see if the increased use of ACT for right lower abdominal pain would result in an increased detection of acute appendicitis. However, assuming the total ED visits as a general population and the incidence of pediatric appendicitis is relatively constant, it is somewhat axiomatic to state that liberal use of ACT would not increase the detection rate of appendicitis and our data proved this. Requesting ED physicians and consulting surgeons alike should acknowledge that the belief that performing more CTs results in more detection of appendicitis, is wooly thinking and false. Except for an acute appendicitis which has long served as an index of surgical disease in the pediatric ED, only a few studies have paid attention to whether abdominal conditions other than appendicitis could benefit from increased utilization of ACT. Fahimi et al. [11] showed that frequent use of CT for pediatric abdominal pain has not improved the detection of underlying conditions requiring invasive interventions. Pines [12] reported that despite a more than doubling in CT use, there was no increase in detection rates for diverticulitis and gall bladder disease in children. We have encountered various surgical conditions during the study period, and have also noted that these conditions have not been detected more frequently despite the increasing use of ACT. Moreover, most of the cases were observed or managed with planned surgery and urgent invasive intervention was needed only in three cases of 32 traumatic solid organ injuries. All of these experiences indicate that the increasing use of ACT had little clinical impact, which suggests the need for some guidelines to restrict unnecessary CT or to select less harmful imaging modalities.
CDRs are decision-making tools for specific disease processes containing variables from the history, physical examination or simple diagnostic tests to help clinicians make bedside diagnostic and therapeutic decisions [13,14]. In this study, ACTs performed for the diagnosis of appendicitis failed to reveal the presence of any surgical diseases in more than half of the cases, thus suggesting the need for clinical tools assessing the likelihood of appendicitis. Samuel [15] has developed a pediatric appendicitis score (PAS) system, in which the equivocal range of a PAS of 3-6 benefitted most from diagnostic imaging tests [16]. Kharbanda et al. [17] developed CDRs to identify children at low risk of appendicitis, and defined those children who could be observed or discharged safely without any imaging tests as those with scores of ≤5. By applying the CDRs, CT utilization has fallen by 20% in those institutions with high rates of CT utilization [18]. In regard to surgical conditions other than appendicitis, in this study, about half of these cases were solid organ injuries following blunt trauma, but only three patients required urgent operation and the rest were simply observed. The Pediatric Emergency Care Applied Research Network has developed a predictive rule, which although it has not passed the external validation yet, identifies children at very low risk for intra-abdominal injuries for whom ACT could be rendered unnecessary [19]. These CDRs are currently not routinely used in our ED, and we expect that routine application of these assessing tools would reduce unnecessary CT scans and their accompanying radiation hazard.
Hospital admission is one of the important patient outcomes affecting overall hospital costs. One could easily expect that the use of CT would effectively rule out a pathological condition and decrease diagnostic uncertainty, allowing for discharge rather than hospital admission for observation. However, there have been some reports showing that, particularly in the field of pediatrics, the hospital admission rate for abdominal pain has not diminished despite the frequent use of ACT [11,12]. Similar to these previous reports, the admission rate for surgical conditions has not diminished during the study period, implying that CT may improve diagnostic accuracy in medical care but is not associated with better outcomes.
Although not covered in depth in this paper, of the various medical conditions, most common diagnosis was gastroenteritis, mainly affecting the ileum and colon. Noninfectious gastroenteritis has been associated with an increased likelihood of receiving a higher radiation-associated imaging procedure [20]. Current guidelines regarding diagnosis and treatment of gastroenteritis vary, but they focus primarily on dehydration assessment and fluid resuscitation, and diagnostic imaging is not recommended as a modality of clinical assessment [21]. Carefully performed physical examination could relatively easily discriminate these medical conditions from the surgical abdomen, thereby avoiding unnecessary CT examinations.
This study had intended only for the patients who underwent the CT evaluation, and a significant problem of selection bias could be suggested. As the USG has been known to be as valuable test as the CT in the diagnosis of various surgical conditions and especially preferred examination for younger children [22], excluding the patients who had undergone USG from the analysis could raise such a problem. However, as shown in Table 2, significant reduction occurred in the use of USG during the study period and the absolute number of USG usage is minimal, our results might not be biased significantly.
In conclusion, we have posed three seemingly plausible questions regarding the increasing utilization of ACT and the outcome of pediatric surgical patient care. Contrary to expectations, increasing use of ACT has not resulted in improved outcomes in caring for surgical patients visiting the pediatric ED. Attention to the radiation hazards in a pediatric population, CDR-based practice in specific clinical conditions, and close cooperation between ED physicians and surgical consultants might be three key elements needed to reduce unnecessary ACT and to protect pediatric patients from high-dose radiation.
Figures and Tables
Table 3
Patient demographics

ACT, abdominal computed tomography; SCOA, surgical conditions other than appendicitis.
*Consistent with or suspicious of appendicitis. †2 Postappendectomy abscess, 1 intussusception, 1 small bowel strangulation, 1 choledochal cyst, 1 acute cholecystitis, 1 hirschsprung's disease. ‡ACTs performed under the clinical impression of acute appendicitis.
References
1. Broder J, Warshauer DM. Increasing utilization of computed tomography in the adult emergency department, 2000-2005. Emerg Radiol. 2006; 13:25–30.
2. Korley FK, Pham JC, Kirsch TD. Use of advanced radiology during visits to US emergency departments for injury-related conditions, 1998-2007. JAMA. 2010; 304:1465–1471.
3. Broder J, Fordham LA, Warshauer DM. Increasing utilization of computed tomography in the pediatric emergency department, 2000-2006. Emerg Radiol. 2007; 14:227–232.
4. McDonald GP, Pendarvis DP, Wilmoth R, Daley BJ. Influence of preoperative computed tomography on patients undergoing appendectomy. Am Surg. 2001; 67:1017–1021.
5. Partrick DA, Janik JE, Janik JS, Bensard DD, Karrer FM. Increased CT scan utilization does not improve the diagnostic accuracy of appendicitis in children. J Pediatr Surg. 2003; 38:659–662.
6. Martin AE, Vollman D, Adler B, Caniano DA. CT scans may not reduce the negative appendectomy rate in children. J Pediatr Surg. 2004; 39:886–890. discussion 886-90.
7. Brenner D, Elliston C, Hall E, Berdon W. Estimated risks of radiation-induced fatal cancer from pediatric CT. AJR Am J Roentgenol. 2001; 176:289–296.
8. Lee CI, Haims AH, Monico EP, Brink JA, Forman HP. Diagnostic CT scans: assessment of patient, physician, and radiologist awareness of radiation dose and possible risks. Radiology. 2004; 231:393–398.
9. Broder JS. CT utilization: the emergency department perspective. Pediatr Radiol. 2008; 38:Suppl 4. S664–S669.
10. Stiell IG, Bennett C. Implementation of clinical decision rules in the emergency department. Acad Emerg Med. 2007; 14:955–959.
11. Fahimi J, Herring A, Harries A, Gonzales R, Alter H. Computed tomography use among children presenting to emergency departments with abdominal pain. Pediatrics. 2012; 130:e1069–e1075.
12. Pines JM. Trends in the rates of radiography use and important diagnoses in emergency department patients with abdominal pain. Med Care. 2009; 47:782–786.
13. Laupacis A, Sekar N, Stiell IG. Clinical prediction rules. A review and suggested modifications of methodological standards. JAMA. 1997; 277:488–494.
14. Stiell IG, Wells GA. Methodologic standards for the development of clinical decision rules in emergency medicine. Ann Emerg Med. 1999; 33:437–447.
15. Samuel M. Pediatric appendicitis score. J Pediatr Surg. 2002; 37:877–881.
16. Goldman RD, Carter S, Stephens D, Antoon R, Mounstephen W, Langer JC. Prospective validation of the pediatric appendicitis score. J Pediatr. 2008; 153:278–282.
17. Kharbanda AB, Taylor GA, Fishman SJ, Bachur RG. A clinical decision rule to identify children at low risk for appendicitis. Pediatrics. 2005; 116:709–716.
18. Macias CG, Sahouria JJ. The appropriate use of CT: quality improvement and clinical decision-making in pediatric emergency medicine. Pediatr Radiol. 2011; 41:Suppl 2. 498–504.
19. Holmes JF, Lillis K, Monroe D, Borgialli D, Kerrey BT, Mahajan P, et al. Identifying children at very low risk of clinically important blunt abdominal injuries. Ann Emerg Med. 2013; 62:107–116.e2.
20. van den Berg J, Berger MY. Guidelines on acute gastroenteritis in children: a critical appraisal of their quality and applicability in primary care. BMC Fam Pract. 2011; 12:134.
21. Zolotor AJ, Randolph GD, Johnson JK, Wegner S, Edwards L, Powell C, et al. Effectiveness of a practice-based, multimodal quality improvement intervention for gastroenteritis within a Medicaid managed care network. Pediatrics. 2007; 120:e644–e650.
22. Antevil JL, Rivera L, Langenberg BJ, Hahm G, Favata MA, Brown CV. Computed tomography-based clinical diagnostic pathway for acute appendicitis: prospective validation. J Am Coll Surg. 2006; 203:849–856.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download