Abstract
Purpose
The present pilot study was conducted to detect putative cancer stem cell (CSC) from the hepatic portal system and peripheral blood in the colorectal cancer patients and to compare them to healthy donor and diverticulitis patients.
Methods
Laboratory study was performed to identify the expression of cell surface markers, epithelial cell adhesion molecule (EpCAM), cytokeratin (CK) 18, CK20, CD44, and CD133, on several colon cancer cell lines. Clinical pilot study was conducted to detect putative circulating CSC as EpCAM+CD133+ cell in colorectal cancer (n = 10), diverticulitis (n = 5), and four healthy donors, by using flow cytometry. Blood was drawn from the hepatic portal system and peripheral vein.
Results
On laboratory study, EpCAM was expressed in whole colon cancer cell lines, and CD44 and CD133 were simultaneously expressed in 50% of the cell lines with stemness phenotype, but CK18 and CK20 were not expressed in most of the cell lines. On clinical study, the mean EpCAM+CD133+ cell counts of 11.6/105 in the hepatic portal system were somewhat lower than 15.4/105 in peripheral vein (P = 0.241). As for diverticulitis patients, EpCAM+CD133+ cells were also detected to have steeper dropped to near zero, after the surgery.
Conclusion
The numbers of putative CSC were not statistically different between the detection sites of the portal vein and peripheral vein in the colon cancer patients. Therefore, we may not have benefitted by getting the cells from the hepatic portal system. In addition, the CD133+EpCAM+ cells in the colon cancer patients might contain normal stem cells from cancer inflammation similar to diverticulitis.
Colorectal cancer is the third most common cancer in the world, and the mortality rate is also the third highest [1,2]. Circulating tumor cells (CTC) from the primary cancer can play an important role in distant metastasis via hematogenous spread [3]. Most CTCs are destroyed by the physical suppression of harsh environment in the circulatory system and the attack of immune cells. However, a little amount of CTC can survive, migrate to distant organs, and lead to metastasis [4]. In particular, the cancer stem cells (CSC) among CTC are known to be responsible for distant metastasis, which accounts for about 2.5% of the tumor cells [5]. The CSC can engage not only in cancer initiating, but also in resisting traditional chemoradiation therapy. Therefore, elevation of circulating CSC in the blood can be related to an unfavorable prognosis for colorectal cancer patients [6]. Nevertheless, the definite features and the detection methods of circulating CSC have not yet been clarified [7].
To date, the flow cytometry and real-time reverse transcription polymerase chain reaction (RT-PCR) with several biomarkers have been used for the detection of circulating CSC. There is no identification method more reliable than others. The CellSearch system, approved by Food and Drug Administration, has been utilized for CTC detection, whereas there is a lack of more reliable detection method for circulating CSC [8]. Currently, the combination of biomarkers using CD133, epithelial cell adhesion molecule (EpCAM), Lgr-5, etc., has been investigated to precisely detect actual CSCs [7].
It is still very challenging to detect circulating CSC by current detection techniques, due to its rareness [5]. Circulating CSC might be expected to exist and detected more in the hepatic portal system than in the peripheral blood, due to direct drainage of the blood from colon cancer. However, there have been few studies on CSC detection methods of using blood in the hepatic portal system.
The present pilot study was conducted to detect putative CSC by using CD133 and EpCAM, known as the stem cell biomarker, from the hepatic portal system in the colorectal cancer patients, and to verify the diagnostic value by comparing to the cell counts from the peripheral blood. In addition, the authors compared them to healthy donor and diverticulitis patients, to weigh cancer-specificity of the method by stem cell biomarker.
First, a laboratory study was conducted with several colon cancer cell lines to identify the expression pattern of cell surface markers. HCT-116, HT-29, SNU-C1, and SNU-C5 were utilized as colon cancer cell lines. In addition, EpCAM, cytokeratin (CK) 18, CK20, CD44, and CD133 were used as cell surface markers. All biomarkers were analyzed by using flow cytometry.
Subsequently, we conducted a prospective clinical pilot study of 10 adult patients who underwent radical colorectal resection for colorectal cancer from May 2012 to October 2012. There were 5 diverticulitis patients, who underwent colon resection, and 4 healthy donors in the control groups. The study was approved by Institutional Review Board of Pusan National University Yangsan Hospital. Written informed consent, regarding the use of biological specimens for investigational purposes, was obtained from all patients. The patients with following conditions were excluded from this study: undergoing emergent operation due to colonic obstruction or perforation, receiving preoperative concurrent chemo-radiation therapy, having other accompanying malignant tumor, requiring palliative surgery, and refusing to participate in the study. The pathologic stages were categorized based on the American Joint Committee on Cancer, 7th edition.
The authors hypothesized that CD133+EpCAM+ cells among the mononuclear cells (peripheral blood-derived mononuclear cells, PBMCs) derived from peripheral blood might be the putative circulating CSCs. The CD133+EpCAM+ cells were detected in the blood samples from the peripheral vein and the hepatic portal system. The blood was drawn from the hepatic portal system during the surgery and from the peripheral vein one day before the surgery, during the surgery, and fifth day after the surgery. We approached the hepatic portal system by the inferior mesenteric vein in the case of rectosigmoid colon cancer, and by the ileocolic vein in the case of ascending colon cancer. The blood was drawn by using a venous catheter after extracting colonic tissue through the minilaparotomy site. Each blood sample was immediately brought to the research laboratory. The authors used density gradient separation, using Ficoll procedure, as enrichment method to extract PBMCs. We also utilized flow cytometry with CD133 and EpCAM staining as an identification method, thereafter.
The patient's peripheral blood was placed into Dulbecco's phosphate-buffered saline at the ratio of 1:2, and it was transferred into Ficoll-paque PLUS (GE Healthcare Bio-Sciences AB, Uppsala, Sweden) to isolate the mononuclear cells. After the centrifugation, a buffy coat layer containing mononuclear cells was transferred to a new tube to be washed by 2mM EDTA/phosphate buffered saline (PBS). To deplete the red blood cells, RBC lysis solution (QIAGEN, Venlo, The Netherland) was added, mixed gently, and incubated at room temperature for 10 minutes, and it was washed by using 2mM EDTA/PBS.
To detect CD133 and EpCAM double positive CSC, the isolated mononuclear cells were incubated with FcR blocking reagents, and the mixture was stained using anti-EpCAM FITC (BD biosciences, San Jose, CA, USA) and anti-CD133/1(AC133) PE (Miltenyi Biotec GmbH, Bergisch Gladbach, Germany) antibodies for 30 minutes at 4℃. The expressions of CD133 and EpCAM were quantitatively measured by FACS Calibur (BD biosciences) and analyzed by CellQuest software (BD biosciences).
The paired T test was used to compare the two sets of measurements. The Wilcoxon signed-rank test was used to compare the means of the abnormally distributed paired variables. P value of less than 0.05 was considered statistically significant. For the analyses, IBM SPSS Statistics ver. 21.0 (IBM Co., Armonk, NY, USA) statistical analysis software was used.
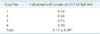
EpCAM expressed in whole colon cancer cell lines is shown on Table 1. Unexpectedly, CK18 was not expressed in any colon cancer cell lines, and CK20 was expressed weakly in only one colon cancer cell line. CD44 and CD133 were simultaneously expressed in 50% outs of the colon cancer cell lines.
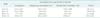
The characteristics of the study group and the control groups are described in Table 2. In the group of healthy donors, CD133+EpCAM+ cells were not detected in all cases (Table 3). For the group of colorectal cancer patients, Table 4 presents CD133+EpCAM+ cell count according to each case. The mean preoperative CD133+EpCAM+ cell count was 11.5 per 105 of PBMCs. All cases had more than one cell, except for the case 3, and over 5 cells were identified in 80% of the cases. The average of CD133+EpCAM+ cell counts, in the blood samples taken during the operation, were 15.4/105 PBMCs and 11.6/105 PBMCs in the peripheral blood and portal vein, respectively; and these values were not different with statistical significance (P = 0.241). Unexpectedly, the average CD133+EpCAM+ cell counts were higher in the peripheral vein than in the hepatic portal system, according to the blood samples taken during the operation. The mean CD133+EpCAM+ cell counts decreased on the 7th day after the operation, compared to during the surgery, and the difference was statistically significant (P = 0.022). In the stage IV colon cancer patients, the mean cell counts after the surgery was maintained at the level of preoperative state, unlike the other stages. In overall, the cell counts were much higher in the stage IV than in the other stages (Table 5).
In the diverticulitis patients, much more CD133+EpCAM+ cells were detected before the surgery, compared to the colo rectal cancer patients (Table 6). There was only a small difference in the cell counts of the blood from peripheral vein, between before the surgery and during the surgery (P = 0.138). However, the intraoperative cell counts from the portal vein were significantly lower compared to the peripheral vein (12.8/105 PBMCs vs. 120.5/105 PBMCs, P = 0.043). Finally, the calculated CD133+EpCAM+ cell counts dropped near to zero on the 5th day after the operation.
The box plot clearly shows the changes in CD133+EpCAM+ cell counts of the study group and the control group (Figs. 1, 2). In addition, Figs. 3 and 4 indicates the flow of the cell counts with lines. The CD133+EpCAM+ cells decreased in both group, and diverticulitis patient group showed sharper decrease over time compared to the colorectal patient group.
CSC is a specific small population that can initiate tumor growth and sustain self-renewal. It is related to distant metastasis of colorectal cancer or tumor recurrence, and may resist traditional chemotherapy and radiotherapy [5]. The currently used promising detection methods for CSC are based on stem cell specific biomarker. It has been reported that some biomarkers such as CD133, CD44, CD24, CD166, Lgr-5, aldehyde dehydrogenase 1, and EpCAM are effective and useful for the detection of CSC. The combination of these can be more valuable in identifying CSC [7].
CD133 was first discovered as a biomarker for normal human hematopoietic stem cell, which was known as prominin-1 [9]. It is believed to be an indicator of tumor initiating cell and one of the key stem cell surface markers of colorectal cancer. The mechanism has not been revealed concretely hitherto. It is thought to play a role in contact formation from cell to cell or from cell to matrix. In particular, CD133 cell is proficient in interacting with carcinoma associated fibroblast. Thus, it is more tumorigenic and invasive. Although there have been controversies surrounding the CD133 cell representing CSC, the CD133 is the most promising biomarker for CSC [10]. There have been studies reporting that high CD133+ cells in the blood were associated with unfavorable prognosis of colorectal cancer patients [9,11].
EpCAM was first described as antigen-generating specific antibodies after immunization of mice with colorectal cancer cells [12]. Some normal epithelia and malignant cells can overexpress EpCAM which can be expressed not only in epithelial cells but in various tissue stem cells and precursors [12,13]. Later in 2008, it was identified as a marker for human embryonic stem cells, and it has been known as a tumor initiating marker. It is thought to target Wnt/b-catenin signaling pathway which is key pathway in CSC and normal adult stem cells [14].
According to our laboratory study, EpCAM was expressed in all colon cancer cell lines, and 50% was in CD133 and CD44. Both CD44 and CD133 are useful biomarkers for the detection of stem cell. Therefore, it is speculated that stem cell-like phenotype may be predominant in the cell lines commonly expressed by CD44 and CD133. Unexpectedly, cytokeratins such as CK18 and CK20, which are known as a significant biomarkers related to colon cancer, were expressed in just a small portion of below 25% of the cell lines. Finally, to isolate putative CSC, we combined CD133 which has been known as one of the most significant biomarker for CSC until now, and EpCAM which was strongly associated with colon cancer cell lines in the study. We examined the differences in putative CSC counts according to the detection sites of the hepatic portal system vs. peripheral vein. In addition, we compared CD133+EpCAM+ cell counts of colorectal cancer patients to diverticulitis patients, and categorized by the preoperative, intraoperative, and postoperative periods.
The intraoperative CD133+EpCAM+ cell counts were not statistically different between the peripheral vein and the hepatic portal system. When we designed the study, we assumed to detect more putative CSCs from the hepatic portal system. Unexpectedly, the study showed that they were not significantly different; but, the peripheral vein rather contained more CD133+EpCAM+ cells than the hepatic portal system. Therefore, we may not have benefitted from obtaining cells from the hepatic portal system. There have been studies on detecting the difference between mesenteric vein and peripheral vein by using putative CTC. Park et al. [15] observed that the expression rates in CEA and CK20 mRNA, which are known as biomarkers for CTC, did not greatly differ between the peripheral vein and the inferior mesenteric vein, and this was similar to our results. However, in contrast to our experiment, Koch et al. [16] reported of significantly higher detection rate for putative CTC in mesenteric vein than in peripheral vein, by using CK20 RT-PCR.
Putative CSC numbers of peripheral vein were not statistically different between the preoperative and the intraoperative periods. On the contrary, they were significantly decreased after the surgery, which is probably because the origins were removed. However, most of them did not reach to zero. The results suggest that a few CSCs steadily escaped into vascular system over a long time, and they might be accumulated in the blood vessel. It was definitely distinct from the colonic diverticulitis patients in this study.
Surprisingly, CD133+EpCAM+ cells were detected much more in the diverticulitis patients of control group. Perforated diverticulitis requiring surgery can cause severe inflammation of the bowel wall. It may trigger intestinal stem cell, located in the crypt base, to spur out into the blood vessel. Furthermore, the cell counts were ten times higher in the peripheral vein than in the hepatic portal system. The results were quite distinct from the colon cancer patients, in which the cell counts were at most 1.5 times higher. As for diverticulitis, stem cells located in colonic crypt may sprout out into the blood vessel, especially under an acute inflammation. After surgery, the source of the inflammation is removed. Few studies on the comparison of CSC between colorectal cancer and benign colonic disease have been found in the literature. Pantel et al. [17] have reported that cell search system could detect pseudo-CTCs in the benign colonic disease. Hardingham et al. [18] also showed the similar result to Pantel et al. [17], by using RT-PCR. Both of them speculated that the reason was inflammation induced by benign colonic disease, which was similar to our result.
Going back to the colorectal cancer patients, it can be considered that a part of CD133+EpCAM+ cells in the colorectal cancer patients may be normal stem cells instead of putative CSCs, as in the diverticulitis patients [19]. The normal stem cells in the colonic crypt might have been peeled off and spilled, with inflammation caused by cancer cells similar to benign colonic disease. Therefore, it is essential to evolve examination techniques to achieve a definite method that can clearly distinguish the circulating CSC from the normal stem cell.
According to this study, CSC detection method using CD133 and EpCAM has several limitations to be adopted as a specific marker for CSC. There were false positives in detecting CD133+EpCAM+ cells in the colonic diverticulitis. However, CD133+EpCAM+ cell counts were remarkably different between the colon cancer patients and the healthy donors. Furthermore, the cell variations among the preoperative, intraoperative, and postoperative state were quite distinct between the cancer patients and the diverticulitis patients. These indicate that the method has a certain value in detecting CSC, even though the CSC cannot be distinguished definitely from the normal stem cell through this detection method. If more valuable detection methods are developed after further investigation, it can greatly help by providing a tailored treatment and better prognosis.
The primary limitation of this study is the small sample size as a pilot study. However, we drew blood four times for each patient, so blood samples were extracted and evaluated in a total of about fifty times. Furthermore, we reasonably consider that our study provides appropriate method for consistency and reproducibility, because the results from the study groups were consistent according to study group. Another limitation of this study is that the detected CD133+EpCAM+ cells could be not confirmed as CSC, by using cytomorphologic evaluation with confocal microscopy (The results was not presented in this paper). Moreover, it has been known that a certain CD133- cells might contain the characteristics of CSC. As we reviewed, the precision of our methods was reliable, but the accuracy is not definitive. However, to date, the method to confirm CSC has not been developed yet. The other limitation is that the methods used in this study required a lot of time and labor. Thus, it is too hard to be adopted in the actual clinical situation. For the future prospective study, investigations including automatic detection system are needed, once the technology becomes available in this field.
In conclusion, the numbers of putative CSC were not statistically different between the detection sites of the portal vein vs. peripheral vein, in the colon cancer patients. Therefore, we may not have benefitted by obtaining cells from the hepatic portal system. In addition, the CD133+EpCAM+ cells in the colon cancer patients might contain normal stem cells from cancer inflammation similar to diverticulitis. More studies should be required on developing specific methods for the detection CSC.
Figures and Tables
Fig. 1
EpCAM+CD133+ cell count according to the period of colorectal cancer patients (n = 10). EpCAM, epithelial cell adhesion molecule; PBMC, peripheral blood-derived mononuclear cell; POD, postoperative day.

Fig. 2
EpCAM+CD133+ cell count according to the period of diverticulitis patients (n = 5). EpCAM, epithelial cell adhesion molecule; PBMC, peripheral blood-derived mononuclear cell; POD, postoperative day.

Fig. 3
EpCAM+CD133+ cell count flows of colorectal cancer patients (n = 10) (The dotted line represents the mean value). EpCAM, epithelial cell adhesion molecule; PBMC, peripheral blood-derived mononuclear cell; POD, postoperative day.

Fig. 4
EpCAM+CD133+ cell count flows of diverticulitis patients (n = 5) (The dotted line represents the mean value). EpCAM, epithelial cell adhesion molecule; PBMC, peripheral blood-derived mononuclear cell; POD, postoperative day.

ACKNOWLEDGEMENTS
This study was supported by Research Institute for Convergence of Biomedical Science and Technology (30-2012-004), Pusan National University Yangsan Hospital.
Notes
References
1. Allen JE, El-Deiry WS. Circulating tumor cells and colorectal cancer. Curr Colorectal Cancer Rep. 2010; 6:212–220.
2. van Dalum G, Holland L, Terstappen LW. Metastasis and circulating tumor cells. J Int Fed Clin Chem Lab Med. 2012; 23:1–11.
3. Pilati P, Mocellin S, Bertazza L, Galdi F, Briarava M, Mammano E, et al. Prognostic value of putative circulating cancer stem cells in patients undergoing hepatic resection for colorectal liver metastasis. Ann Surg Oncol. 2012; 19:402–408.
4. Kim MY, Oskarsson T, Acharyya S, Nguyen DX, Zhang XH, Norton L, et al. Tumor self-seeding by circulating cancer cells. Cell. 2009; 139:1315–1326.
5. Tsai KS, Yang SH, Lei YP, Tsai CC, Chen HW, Hsu CY, et al. Mesenchymal stem cells promote formation of colorectal tumors in mice. Gastroenterology. 2011; 141:1046–1056.
6. Lugli A, Iezzi G, Hostettler I, Muraro MG, Mele V, Tornillo L, et al. Prognostic impact of the expression of putative cancer stem cell markers CD133, CD166, CD44s, EpCAM, and ALDH1 in colorectal cancer. Br J Cancer. 2010; 103:382–390.
7. Vaiopoulos AG, Kostakis ID, Koutsilieris M, Papavassiliou AG. Colorectal cancer stem cells. Stem Cells. 2012; 30:363–371.
8. Scatena R, Bottoni P, Giardina B. Circulating tumour cells and cancer stem cells: a role for proteomics in defining the interrelationships between function, phenotype and differentiation with potential clinical applications. Biochim Biophys Acta. 2013; 1835:129–143.
9. Chen S, Song X, Chen Z, Li X, Li M, Liu H, et al. CD133 expression and the prognosis of colorectal cancer: a systematic review and meta-analysis. PLoS One. 2013; 8:e56380.
10. Ren F, Sheng WQ, Du X. CD133: a cancer stem cells marker, is used in colorectal cancers. World J Gastroenterol. 2013; 19:2603–2611.
11. Silinsky J, Grimes C, Driscoll T, Green H, Cordova J, Davis NK, et al. CD 133+ and CXCR4+ colon cancer cells as a marker for lymph node metastasis. J Surg Res. 2013; 185:113–118.
12. Imrich S, Hachmeister M, Gires O. EpCAM and its potential role in tumor-initiating cells. Cell Adh Migr. 2012; 6:30–38.
13. Munz M, Baeuerle PA, Gires O. The emerging role of EpCAM in cancer and stem cell signaling. Cancer Res. 2009; 69:5627–5629.
14. Waldron NN, Barsky SH, Dougherty PR, Vallera DA. A bispecific EpCAM/CD-133-targeted toxin is effective against carcinoma. Target Oncol. 2014; 9:239–249.
15. Park SY, Choi GS, Park JS, Kim HJ, Ryuk JP, Choi WH. Influence of surgical manipulation and surgical modality on the molecular detection of circulating tumor cells from colorectal cancer. J Korean Surg Soc. 2012; 82:356–364.
16. Koch M, Weitz J, Kienle P, Benner A, Willeke F, Lehnert T, et al. Comparative analysis of tumor cell dissemination in mesenteric, central, and peripheral venous blood in patients with colorectal cancer. Arch Surg. 2001; 136:85–89.
17. Pantel K, Deneve E, Nocca D, Coffy A, Vendrell JP, Maudelonde T, et al. Circulating epithelial cells in patients with benign colon diseases. Clin Chem. 2012; 58:936–940.
18. Hardingham JE, Hewett PJ, Sage RE, Finch JL, Nuttall JD, Kotasek D, et al. Molecular detection of blood-borne epithelial cells in colorectal cancer patients and in patients with benign bowel disease. Int J Cancer. 2000; 89:8–13.
19. Sato T, Vries RG, Snippert HJ, van de Wetering M, Barker N, Stange DE, et al. Single Lgr5 stem cells build crypt-villus structures in vitro without a mesenchymal niche. Nature. 2009; 459:262–265.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download