Abstract
Jejunal and ileal diverticula are rare in adults. Duodenal diverticula are five times more prevalent than jejunoileal diverticula. Most patients are asymptomatic. However, chronic symptoms including intermittent abdominal pain, flatulence, diarrhea and constipation are seen in 10%-30% of patients. Gastric cancer is the second most common cancer in South Korea and here we report a case of early gastric cancer with multiple duodenal and jejunal diverticula. A 67-year-old woman was admitted to Konkuk University Medical Center with chronic diarrhea and weight loss of 19 kg over 2 months. Following gastroduodenoscopy, we identified adenocarcinoma of the lower body of the stomach. On abdominopelvic computed tomography, diverticula of duodenum and jejunum were found. Patient underwent distal gastrectomy and gastroduodenostomy with lymphadenectomy. She was discharged on the tenth postoperative day without complications.
Diverticula of the jejunum and ileum are rare in adults [1]. In the small intestine, duodenal diverticula are nearly five times more common than jejunoileal diverticula [2]. The majority of patients with small bowel diverticula remain symptom free, yet, acute complications may happen which include obstruction, gastrointestinal bleeding, diverticulitis and perforation. Chronic symptoms are also reported in these patients, which include intermittent abdominal pain, flatulence, diarrhea and constipation [3].
In South Korea, the second most common organ cancer develops in the stomach [4]. Resectable treatment options are subtotal or total gastrectomy, which are based on the site of the tumor. Reconstruction options after subtotal gastrectomy are gastroduodenostomy or gastrojejunostomy.
In the literature, there are case reports of gastric cancer accompanied Meckel's diverticulum or duodenal diverticulum. But, combination of gastric cancer and multiple diverticula of duodenum and jejunum is not reported. Here, we report a case of early gastric cancer which had duodenal and jejunal diverticula.
A 67-year-old woman was admitted to Konkuk University Medical Center with the chief complaint of chronic diarrhea and a significant weight loss of 19 kg over 2 months. The patient also complained of general weakness and dizziness along without abdominal pain. Past medical history was otherwise unremarkable but her surgical history showed that the patient had undergone appendectomy 19 years prior to this presentation and balloon dilatation of a duodenal stricture 4 years before her current presentation which was not found to be of a known origin.
Her laboratory tests at the time of admission showed elevated WBC count of 11,190/mm3 (normal range, 4,000-10,000/mm3) and low hemoglobin level of 9.6 g/dL (normal range, 12.0-16.0 g/dL). We also found low albumin level of 1.6 g/dL (normal range, 3.3-5.3 g/dL) and 2.9-mmol/L low potassium level (normal range, 3.5-5.5 mmol/L). The patient had prolonged prothrombin time of 23.7 seconds (normal range, 11.7-14.7 seconds) and prolonged activated partial thromboplastin time of 75.2 seconds (normal range, 29.0-45.0 seconds). Urinalysis found 3 WBC in high-power field (negative is normal) and bacteria. Based on these findings, we had initial impressions of protein losing gastroenteropathy and urinary tract infection.
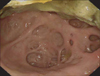
In gastroduodenoscopy, we identified a 5-mm ulcerative lesion on the greater curvature of the lower body of the stomach and duodenal diverticula on second and third parts of the duodenum (Fig. 1). The lesion of the stomach was endoscopically clipped. Pathology study of the endoscopic biopsy confirmed a moderately differentiated adenocarcinoma. Abdominopelvic computed tomography (APCT) revealed multiple diverticula in duodenum and jejunum. Small bowel loops were slightly dilated with fluid and there was no evidence of inflammation around diverticula (Fig. 2). APCT did not find lymphadenopathy or distant metastasis, therefore, the clinical stage of this gastric cancer was cT1N0M0.
During the surgery, no gastric tumor could be palpated but endoscopic clip was palpated. There was no peritoneal seeding or metastatic lesion. The observable site of pylorus was displaced proximally due to the previous ulcer scar (Fig. 3A). We found diverticula with 2- to 3-cm size on second and third parts of the duodenum (Fig. 3B). In a distance of about 150 cm from the ligament of Treitz to the jejunum, we identified 20-30 diverticula on the mesenteric border of the small bowel which had a median size of 3-4 cm (Fig. 3C, D). Distal gastrectomy and gastroduodenostomy with lymphadenectomy concluded the operation.
Pathology report confirmed moderately differentiated adenocarcinoma with mucosal invasion. There was no metastasis in the 21 retrieved lymph nodes. Final TNM staging was T1N0M0, stage Ia.
The patient recovered without complications and was discharged on the 10th postoperative day.
Diverticula of the jejunum and ileum are not commonly seen in adults; occurring in approximately 1%-2% of the population [1]. Duodenal diverticula are five times more prevalent than jejunoileal diverticula [2]. Duodenal diverticula are divided into primary congenital diverticula and secondary acquired pseudodiverticula. Congenital diverticula of the duodenum are very rare in which all layers of the intestinal wall are herniated [5]. The etiology of small bowel pseudodiverticula is unclear but it is believed that motor dysfunction or intestinal dyskinesia leads to the formation of a diverticulum [6]. Following the increase in intraluminal pressures, the mucosa and submucosa protrude through the weakest site of the muscularis layer [6]. In general, the weakest site of the bowel wall is on the mesenteric border [6].
Patients with small bowel diverticula are typically asymptomatic. However, acute complications such as obstruction, gastrointestinal bleeding, diverticulitis, and perforation can occur which may need emergent surgical intervention. The treatment of choice in these settings is segmental resection of small intestine harboring the diverticulum [7,8]. Chronic symptoms such as intermittent abdominal pain, flatulence, diarrhea, and constipation are reported in 10%-30% of patients with jejunoileal diverticula [3]. Conservative management is recommended when acute complication are not seen [8].
The reason for malabsorption is not clear but stasis in diverticular lumen is hypothesized to be the cause. Stasis results in an overgrowth of coliform organisms similar to the blind loop syndrome. It leads to vitamin B12 deficiency and consequently megaloblastic anemia. Steatorrhea could also develop. These complex pathophysiologic changes lead to malabsorption [1,6]. Medical treatment is the first step of management in patients with malabsorption including our presented case. These treatment measures include administration of oral antibiotics (e.g., metronidazole), high-protein low-residue diet and vitamin supplementation [1,2,9]. Surgical treatment is reserved for patients who are intractable to medical treatment or who have serious malabsorption or steatorrhea.
It is widely accepted that the surgical treatment of early gastric cancer on the lower body of the stomach is distal gastrectomy with lymphadenectomy. After radical resection, surgeon decides the method of anastomosis which could be either gastroduodenostomy or gastrojejunostomy. This decision is difficult to make in patients with small bowel diverticula. Duodenal or jejunal diverticula around the site of the anastomosis may lead to complications such as anastomosis leakage, bleeding, ulcer and perforation which develop after direct contact with incompletely digested food. In our presented case, gastroduodenostomy was performed. There were two reasons behind this decision. First, gastrojejunostomy could become more complicated because stasis in the afferent loop can increase the intraluminal pressure in the diverticula and cause more diverticular complications. Second, this anastomosis method is closer to physiologic states.
Figures and Tables
Fig. 2
Abdominopelvic computed tomography findings. Arrows point to the diverticula in duodenum and jejunum. (A, B) Axial view, (C, D) coronal view.

Fig. 3
Intraoperative findings showing diverticula in duodenum and jejunum. (A) Previous ulcer scar (arrow). (B) Diverticula in the second portion of the duodenum (arrows). (C) Jejunal diverticula on the mesenteric border of the small bowel. (D) Jejunal diverticula become smaller as we move distally until the diverticula disappear (arrow: terminal end of diverticula).

References
1. Longo WE, Vernava AM 3rd. Clinical implications of jejunoileal diverticular disease. Dis Colon Rectum. 1992; 35:381–388.
2. Akhrass R, Yaffe MB, Fischer C, Ponsky J, Shuck JM. Small-bowel diverticulosis: perceptions and reality. J Am Coll Surg. 1997; 184:383–388.
3. Choi JJ, Ogunjemilusi O, Divino CM. Diagnosis and management of diverticula in the jejunum and ileum. Am Surg. 2013; 79:108–110.
4. Jung KW, Won YJ, Kong HJ, Oh CM, Seo HG, Lee JS. Cancer statistics in Korea: incidence, mortality, survival and prevalence in 2010. Cancer Res Treat. 2013; 45:1–14.
5. Thorson CM, Paz Ruiz PS, Roeder RA, Sleeman D, Casillas VJ. The perforated duodenal diverticulum. Arch Surg. 2012; 147:81–88.
6. Woods K, Williams E, Melvin W, Sharp K. Acquired jejunoileal diverticulosis and its complications: a review of the literature. Am Surg. 2008; 74:849–854.
7. Koger KE, Shatney CH, Dirbas FM, McClenathan JH. Perforated jejunal diverticula. Am Surg. 1996; 62:26–29.
8. Lee BG, Park SB, Byun CG, Koh YT, Suh DY, Park DS, et al. Localized peritonitis due to perforation of multiple jejunal diverticula. J Korean Surg Soc. 2004; 67:75–78.
9. Kassahun WT, Fangmann J, Harms J, Bartels M, Hauss J. Complicated small-bowel diverticulosis: a case report and review of the literature. World J Gastroenterol. 2007; 13:2240–2242.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download