This article has been
cited by other articles in ScienceCentral.
Abstract
Purpose
The diagnosis-related group (DRG) system has been adapted to reduce overall medical costs by grouping and classifying relatively homogenous patients based on similar resource consumption patterns in the treatment. However, despite its wide range of disease manifestation from early inflammation to severe peritonitis, acute appendicitis is included in the DRG system. Responding to a need to assess the DRG system for patients diagnosed with appendicitis, this study evaluates the efficacy of the current DRG system applied to a broad spectrum of the patients with appendicitis undergoing laparoscopic appendectomy.
Methods
A retrospective review was conducted of the patients who underwent laparoscopic appendectomy. Based on the DRG codes' classification, the patients were analyzed for the amount of DRG reimbursement and the total in-patient cost in relation to the time sequence of the disease onset. Statistical analysis was performed to find factors correlated with the DRG reimbursement and total in-patient cost.
Results
Findings indicate that, as the symptom duration becomes prolonged, the CRP level and the use of peritoneal drainage increased. Patients with a symptom duration greater than 24 hours required approximately 5 days of hospital stay, 0.5 day longer in the length of hospital stay than that of patients with less than 12 hours of the onset time. As expected, the amount of DRG reimbursement and the total in-patient cost accumulated as the symptom duration increased.
Conclusion
The current DRG reimbursement system for the patients undergoing laparoscopic appendectomy recompenses a broad spectrum of patients diagnosed with appendicitis effectively.
Keywords: Diagnosis-related groups, Laparoscopy, Appendectomy, Severity of illness index
INTRODUCTION
Superfluous medical cost has been the greatest issue in public health in modern era. Reimbursement systems based on diagnosis-related group (DRG) for selected diseases have been adopted in many different countries in an effort to reduce excessive medical cost and to prevent unnecessary overtreatment. In Korea, the DRG reimbursement system was first introduced in 1997 [
1]. In 2002 various levels of hospitals adopted the system by choice for seven different diseases: cataracts, adenoid disease, anal disease, inguinal hernia, cesarean delivery, female sex organ diseases, and appendicitis [
1]. Only recently have all levels of hospitals and medical facilities mandatorily adopted the DRG system for all seven diseases. Although the DRG system has long been the topic of debate between healthcare providers and public health insurance services, it has since become a spotlighted issue in public health.
In dealing with ever-increasing medical costs along with rapid developments in medical science, the DRG system attempts to reduce overall medical cost by grouping and classifying patients based on similar resource consumption patterns in treatment. However, to healthcare providers, individual patients may present a broad spectrum of diseases, and medical cost can vary in each individual. Acute appendicitis is one salient example that exhibits a very wide range of disease presentation, from very early inflammation to the severe peritonitis. Since acute appendicitis is included in the DRG system, it is unavoidable for healthcare providers to treat patients within the parameters that the system allows. This study investigated whether the current DRG system efficiently covers the broad spectrum of patients. Furthermore, presuming that the longer the patients' symptoms present, the more severe the disease is, we tried to determine the factors that influence the amount of the DRG reimbursement and total in-patient cost.
METHODS
Following approval by the Institutional Review Board, a retrospective review was performed for the patients who underwent laparoscopic appendectomy from July 2012 to February 2013. All patients with DRG code number G08300, G08301, G08302, G08400, G08401, and G08402 generated by the National Health Insurance Service were included.
Each code number was labeled after the surgical procedure using laparoscopy. G08300 represents the patient diagnosed with perforated appendicitis who underwent laparoscopic appendectomy without any complications or comorbidity. G08301 reflects the patient with perforated appendicitis who underwent laparoscopic appendectomy with moderate complications or comorbidity. G08302 classifies the patient with perforated appendicitis who underwent laparoscopic appendectomy with severe complications or comorbidity. G08400, G08401, and G08402 describe patients with nonperforated appendicitis without any complications or comorbidity, with moderate complications or comorbidity, and with severe complications or comorbidity. Each number is automatically determined for patients by the hospital's own software program compatible with the DRG categorizing program provided by the Health Insurance Review and Assessment Service. Patients who had open conversions during the surgical procedure were excluded.
Patient records were reviewed for demographic data, the onset time of symptoms reported, laboratory and imaging results, intraoperative findings, along with the use of postoperative peritoneal drainage, and pathology. Outpatient records were reviewed for postoperative complications.
The time at Emergency Department registration, the time of skin incision, and the operation duration were gathered from patient charts. The time interval between registration and initiation of the operation was termed the door-to-incision time. Night operations, defined as operations performed between 6 PM and 6 AM, were also included in the data analysis. Length of hospital stay, DRG reimbursement, and total in-patient cost were obtained from the Department of Insurance Management in the hospital for cost analysis.
Patients were divided into three groups. The first group included patients with less than or equal to 12 hours of interval time between the onset of symptom and the Emergency Department registration. The second group consisted of patients with symptom duration of 12 to 24 hours. The third group exhibited symptom duration of over 24 hours.
SAS enterprise guide ver. 4 (SAS Institute Inc., Cary, NC, USA) was used for statistical analysis. For analyses of continuous dependent variables, we used independent t-test or Analysis of variance (ANOVA) method. Duncan's studentized range post hoc test was performed to investigate statistically significant results. For analyses of categorical variables, a chi-square test was used. A P-value of <0.05 was considered statistically significant. To investigate correlations for each variable, a Pearson correlation coefficient was used. Regression analysis was performed to investigate statistically significant relationships with different variables.
RESULTS
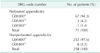
During this 8-month period, 329 patients (174 females and 155 females; male to female ratio = 0.89) were included in this study. Based on the DRG codes, 71 patients were given a code indicating perforated appendicitis, and 258 patients were classified using a code for nonperforated appendicitis (
Table 1). Approximately 94% of patients in the perforated group and 97% in the nonperforated group did not exhibit any comorbidity or complications superimposed upon the appendicitis. The comorbidity or complications observed in this study included aplastic anemia, which required transfusion, end stage renal disease requiring hemodialysis, postoperative trocar site bleeding requiring reoperation, and postoperative adhesive ileus.
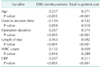
Depending on the symptom duration, the characteristics of three patient groups are characterized in
Table 2. A total of 123 patients visited the Emergency Department within 12 hours after the onset of symptoms: group A. For 95 patients, the symptom onset time fell into the time line over 12 hours but less than 24 hours: group B. One hundred and eleven patients came to the emergency room 24 hours after developing initial symptoms: group C.
All three groups showed no difference in age and sex. To estimate the severity of the disease, the WBC count and CRP were monitored. Although the WBC count was not significantly different, the CRP level was significantly higher in patients with the longer symptom duration. Because the use of postoperative peritoneal drainage has been a long-standing custom used in patients with perforated appendicitis, the tendency to use postoperative peritoneal drainage was investigated. Of patients with a symptomatic period greater than 24 hours, 28.8% had peritoneal drainage postoperatively, whereas only 12.2% of patients with symptom duration less than 12 hours received postoperative peritoneal drainage. As expected, the longer the symptom duration, the greater was the use of postoperative peritoneal drainage was present: a statistically significant correlation.
Based on the DRG codes for laparoscopic appendectomy, the number of patients categorized in each time zone of the symptom duration was totaled. Of the 71 patients coded for perforated appendicitis, 59% showed symptom duration greater than 24 hours. Meanwhile, approximately 72% of patients assigned to the nonperforated appendicitis claimed symptom duration less than or equal to 24 hours.
The mean waiting hours between arrival at the Emergency Department and the operation, door-to-incision time, was 8.2 hours, 7.6 hours, and 7.1 hours, respectively, for each group. The mean operation duration was 49.5 minutes, 49.1 minutes, and 54.7 minutes, accordingly. The door-to-incision time and operation duration did not differ statistically among the three groups. All three groups showed a similar distribution in the timing of the operation, whether performed during the day or night. The patients in groups B and C had 4.9 days and 5.0 days of hospital stay, respectively, which is significantly longer than 4.5 days in group A.
The amount of DRG reimbursement was 2,472,740 Korean Won (KRW) for group C. For groups A and B, the reimbursement values were 2,374,830 and 2,394,990 KRW respectively, which were significantly lower than for the group C. The total in-patient cost for each group is shown in
Table 2. Despite the higher amount of DRG reimbursement for the group C, the total in-patient cost was not significantly different among the three groups.
The postoperative complications were present in less than 10% of all three groups, and a statistically significant difference was not observed. Complications included wound infection, intraperitoneal abscesses, postoperative trocar site bleeding and postoperative adhesive ileus.
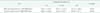
Because additional payment is given for operations performed during the nighttime, weekends, and holidays, so called
nonelective hours, the operations conducted in the nonelective hours are compared to the ones performed during daytime or elective hours, shown in
Table 3. Expectedly, the DRG reimbursement cost is higher for the operations carried out in the nonelective hours. Considering nighttime or overtime allowance, higher total in-patient cost for operations performed during nonelective hours is an understandable consequence. The symptom duration did not favor a particular time zone for the operation. None of the other variables showed a statistically significant difference.
To analyze which variables were correlated with the DRG reimbursement and total in-patient cost, Pearson correlation coefficients were calculated.
Table 4 lists the variables correlated to the DRG reimbursement and total in-patient cost. Factors including age, operation duration, and the CRP level may influence both the reimbursement and the total in-patient cost, although the correlation coefficients are relatively low. Length of hospital stay was the only factor that showed a reasonable correlation with the amount of DRG reimbursement. Moreover, the length of hospital stay showed even greater correlation with the total in-patient cost.
To find the variables affecting the DRG reimbursement directly, multiple regression analysis was performed. In
Table 5,
6 the variables with statistical significance are listed. The overall regression model presents an F-value of 43.8 with a P < 0.0001, which is highly statistically significant. The R-squared was equal to 0.356, meaning that this current regression model may explain 35.6% on how the variables affecting the amount of DRG reimbursement. The regression equation is noted subsequently:
DRG reimbursement amount = 2,106 - 9.20 × (door to incision time) + 61.13 × (length of hospital stay) + 129.33 × (nonelective operation) + 132.33 × (use of peritoneal drainage)
The increased door-to-incision time functions negatively with the amount of DRG reimbursement. The DRG reimbursement amount is increased when the operation is carried out during nonelective hours, when the length of hospital stay is prolonged, and when peritoneal drainage is used.
Multiple regression analysis was also performed to analyze variables influencing the total in-patient cost.
Table 7,
8 list the statistically significant variables influencing the total in-patient cost. The overall regression model demonstrates an F-value of 72.46 with a P < 0.0001, indicating statistical significance. This model can explain 53.4% of the total in-patient cost, reflected in the R-squared value. The regression equation can be written as follows:
Total in-patient cost = 1222 + 2.12 × (Age) + 49.44 × (symptom duration < 12 hr) + 2.03 × (operation duration) + 129.49 × (length of hospital stay) + 80.79 × (nonelective operation)
The total in-patient cost becomes higher when a patient is older, when the operation duration takes longer, and when the length of hospital stay is prolonged. Interestingly, in this regression model, symptom duration of less than 12 hours was found to be a factor that increases the total in-patient cost. In this equation, all five factors function additively to increase the total in-patient cost.
In fact, calculating the daily cost in each group from the total amount divided by the total length of hospital stay (
Table 1), the daily cost was the greatest in the patient group with the symptom duration less than 12 hours for both DRG reimbursement and total in-patient cost, shown in
Table 7. This result is affected solely by the length of hospital stay. The mean length of hospital stay was about 4.5 days for the patients with the symptom duration less than 12 hours, whereas it was about 5 days for the patients with symptom duration greater than 12 hours. The difference of merely half a day made almost negative value difference of 45,000 KRW/day in the total in-patient cost and 40,000 KRW/day for the amount of DRG reimbursement. This result demonstrates that the medical cost is mostly determined within the first 4 days of hospital stay.
DISCUSSION
Laparoscopic appendectomy is now recognized as the superior surgical technique in the management of both nonperforated and perforated appendicitis in terms of patient outcome [
2,
3,
4]. Also, several studies regarding medical cost and cost-effectiveness substantiate the laparoscopic procedure's low overall cost and reduced length of hospital stay compared to the open procedure [
5,
6,
7]. In the effort to minimize ever increasing medical cost, many different countries are adopting the DRG system in managing patients with appendicitis. Since laparoscopic appendectomies have recently been covered by DRG system in Korea, it is necessary to evaluate the efficacy and cost effectiveness of the system and identify any avoidable or adjustable factors that may increase the overall medical cost.
This study found that as the symptom duration of the disease becomes prolonged, both the medical cost and the length of hospital stay increase. Doubling the CRP level consecutively in a 12-hour time interval supports rapid progression of the disease. This study did not examine the pathological turnover rate of perforated appendicitis in temporal sequence. Because the specimen tissue may become damaged while delivered through the trocar port incision in laparoscopic appendectomy, the pathologic analysis may be influenced by damaged tissue, bearing inaccuracy. However, as evidenced by previous studies indicating that the CRP level directly correlates with the severity of the inflammation in acute appendicitis [
8,
9], increased symptom duration was found to correlate with the aggravation of the disease. This finding also supports the notion that increased symptom duration is correlated with increased medical cost and length of hospital stay. In fact, the current DRG system for laparoscopic appendectomy is composed of six different categories codes for either perforated or nonperforated appendicitis, subcategorized by the presence of comorbidities or complications based on the degree of severity. This study's data indicate that only very few patients exhibited comorbidities or complications. This may be due to that the study is only limited to the patients who underwent laparoscopic appendectomy. The disease progression over the course of time clearly leads to increased medical cost and length of hospital stay.
Besides monitoring the CRP level, this study also investigated the use of peritoneal drainage since it has been the longstanding custom for treating appendicitis with gangrenous change, peritonitis, or perforation. Conceivably in the patients with symptom duration greater than 24 hours, the use of peritoneal drainage was raised over 14% compared to the patients with the symptom duration less than 12 hours and between 12 to 24 hours. Albeit limited to children, a prior study revealed that the use of peritoneal drainage is associated with increased length of hospital stay, prolonged use of antibiotics, and slow oral feeding [
10]. Such findings are consistent with this study's data demonstrating that the use of peritoneal drainage augments the amount of DRG reimbursement. Therefore, it is certain that the aggravating disease raises resource consumption and consequently inflates medical costs. Despite the increased consumption of medical resources, the effect of peritoneal drainage has not been validated in adults with perforated appendicitis. Considering the trivial outcome in children [
10,
11], abandoning the use of peritoneal drainage may contribute to the reduction of the gratuitous resource consumption.
Analyzing the factors influencing the amount of DRG reimbursement, notably door-to-incision time has a negative effect on DRG reimbursement. It is understandable that shortening the door-to-incision time prevents lengthening of hospital stay. Nevertheless, it was shown that extended door-to-incision time was significantly associated with increased surgical site infection [
12]. Thus, the current DRG reimbursement system effectively promotes efficient medical practice in that aspect. Furthermore, when operations are performed during nonelective hours, it appeared to increase the amount of DRG reimbursement as well as the total in-patient cost in this study. Comparing the operation performed during elective hours to nonelective hours, no significant difference was found in patient demographics, disease severity, or treatment outcome. The data also suggest that the amount of DRG reimbursement sufficiently recompenses the total in-patient cost; thus, the current DRG reimbursement system yields increased cost for patient treatment and appropriately allocates the extra demands.
Age appears to raise the total in-patient cost but not the amount of DRG reimbursement. Although lacking statistical significance, the data suggest that the symptom duration gets longer as age rises. This may imply that older patients tend to seek medical attention when the symptoms get severe. Consistent with this study's findings, a previous study on the clinical features of appendicitis in the elderly demonstrates that the elderly exhibited a higher rate of perforated appendicitis than did pediatric and adult patients [
13]. When compared the rate of perforated to nonperforated appendicitis, the elderly also presented higher proportion of perforated cases [
13]. Postoperative morbidity was significantly high in the elderly, and this was associated with preoperatively diagnosed comorbid medical conditions [
13,
14]. Such findings indicate that elderly patients diagnosed with appendicitis may require an ample amount of medical attention along with an extended length of hospital stay, demanding significantly higher medical costs. However, the current DRG system seems to disregard the age factor in adjusting the reimbursement. Age should be taken into account so healthcare providers can provide optimal medical services to the elderly. A further study on the disparity of medical costs related to age in patients with appendicitis may offer the appropriate means for reimbursement.
Oddly, symptom duration of less than 12 hours plays a part in augmenting the total in-patient cost. This result may impose concerns regarding the process of immediate medical service from the diagnosis to surgical management for the patients presenting early appendicitis. Even though the data are inadequate to prove the statistical significance of this correlations, patients tended to have a longer door-to-incision time as the symptom duration was extended, presenting a nearly 1.2-hour difference in door-to-incision time between patients symptom duration less than 12 hours and those with symptom duration greater than 24 hours. This can be explained in several ways. First, it is not uncommon to encounter patients with ambiguous clinical presentation of very early inflammation of the appendix. However, the diagnosis can be challenging, especially when imaging studies with abdominal computed tomography or ultrasound provide inconclusive results. For those patients, repeated blood tests and in-patient monitoring are often provided in our facility. Need for surgical treatment is determined once the patients develop aggravated symptoms. This entire process requires additional resource consumption just for the diagnosis; consequently, the total inpatient cost may arise. Such circumstances should be considered in revising the DRG classification. Another concern is related to the discretion of the healthcare providers in delaying the surgery. With or without the intention of doing so, healthcare providers, not only surgeons but also anesthesiologists or even hospital administrators, may not prioritize the surgery for patients presenting with uncomplicated appendicitis, especially during elective hours when other surgeries await. Delaying the surgery itself can extend the length of hospital stay, which is shown to increase both the amount of DRG reimbursement and the total in-patient cost. Therefore, delaying the surgery should be monitored and examined carefully to improve the quality of medical service.
In conclusion, the current DRG reimbursement system for the patients undergoing a laparoscopic appendectomy appears to cover a broad spectrum of the patients diagnosed with appendicitis relatively well. However, patient selection for who undergoes laparoscopic appendectomy versus open appendectomy by a surgeon would largely affect the study's results. In addition to this selection bias, this single-centered study with a small sample size is limited to represent the overall outcome of the DRG reimbursement system nationwide. Therefore, it is difficult to generalize that the current DRG reimbursement system adequately implements all patients who undergo laparoscopic appendectomy. Similar studies in other medical facilities or hospitals should be carried out to demonstrate the efficacy of the current DRG reimbursement system.
It is indisputable that the prolonged symptom duration will result in disease progression and consequently increase medical costs. In an effort to reduce the overall medical cost, public medical education on appendicitis will achieve general consensus on when to seek appropriate medical care readily. This will help reduce the rate of perforated appendicitis, which may contribute to cutting down on the overall medical cost. Considering the DRG classification, particular apprehension should be taken for cases exhibiting difficulty in diagnosis as well as the elderly with pre-existing comorbid medical condition and possible complications associated with surgery. Finally, monitoring door-to-incision time will provide important information on the performance of the healthcare providers, in regard to not only the outcome but also the process of medical service.





 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download