Abstract
Purpose
The purpose was to evaluate outcomes according to different operative strategies of type A esophageal atresia (EA).
Methods
All patients who underwent surgery for type A EA between 1980 and 2011 were included. Patients were divided into 2 groups: E-E group included patients who received esophageal end-to-end anastomosis, whereas E-G group included patients who received esophago-gastric tube anastomosis.
Results
Twenty-two patients were included. The median gestational age was 37.5 weeks. The median birth weight was 2.5 kg. Twenty-one patients underwent gastrostomy as initial procedures, and one patient underwent primary esophageal end-to-end anastomosis. The median gap between both esophageal ends was six vertebral distance (VD). Seven patients underwent primary anastomosis of the esophagus, and 14 patients underwent gastric replacement. Three patients (13.6%) had anastomotic leakage and 10 patients (45.5%) had anastomotic stenosis. Most of the patients (90.9%) had gastroesophageal reflux, but only two patients required antireflux surgery. The median VD was significantly shorter in E-E group than in E-G group (3 VD vs. 6 VD). Stenosis was significantly more often in E-E group, but there was no significant difference in leakage and reflux symptoms.
Conclusion
The treatment for type A EA can include E-E anastomosis or E-G anastomosis, depending on the length of the end-to-end interval after performing gastrostomy. Appropriate tension and blood flow in the anastomosis site are essential for preventing postoperative stenosis and leakage, and esophageal replacement with gastric tube is believed to be feasible and safe in cases where excessive tension is present.
In most cases of type A esophageal atresia (EA), immediate primary anastomosis is difficult to perform because the intervals between both ends of the esophagus are longer than that in other types of EA. Usually, gastrostomy can be priorly performed, followed by either esophageal replacement or delayed primary anastomosis; however, each procedure has its own advantages and disadvantages [1]. The advantage of performing early gastrostomy followed by esophageal replacement with gastric tube is that the anastomosis can be performed by reducing the tension in cases where the length of the esophagus is insufficient; however, this has been reported to result in gastroesophageal reflux (GER) and anastomotic stenosis because of the change in the location of the gastroesophageal junction to the chest, which is caused by raising the mobilized stomach through the hiatus [2].
In cases where delayed primary anastomosis after early gastrostomy is performed, the prognosis associated with GER and swallowing function is reportedly better because the native esophagus is preserved [1]. However, providing continuous treatment in the neonatal intensive care unit (ICU) until the esophagus reaches an appropriate length has disadvantages that such as the cost and the risk of pathogenic infections, including repeated pneumonia due to aspiration [3].
Therefore, in this study, we aimed to compare the outcomes of different types of surgical treatment for type A EA by evaluating the patients from a single institution.
We performed a retrospective study using the medical records of 22 patients (13.4%) who were found to have type A EA, among 164 patients diagnosed with EA at our institution from January 1980 to December 2011.
The demographic factors such as sex, birth weight, gestational age and associated anomalies, as well as the diagnostic method, operative method, complications, treatment for the complications, and outcomes were investigated.
If asymptomatic stenosis at the anastomosis site was detected on esophagography, it was categorized as mild; in addition, cases that improved after endoscopic balloon dilatation (EBD) were categorized as moderate, whereas and those requiring surgical treatment were categorized as severe. With regard to GER and anastomosis leakage, cases that exhibited an improment after conservative treatment were categorized as mild to moderate, whereas those requiring surgical treatment were categorized as severe.
For the analysis of outcomes according to operative methods, 21 patients excluding 1 patient who received primary esophageal end-to-end anastomosis without gastrostomy were divided into the end-to-end (E-E) and esophago-gastric tube (E-G) groups. The E-G group was further divided into the isoperistaltic and antiperistaltic groups depending on the peristaltic direction of the gastric tube. We used PASW ver. 18.0 (SPSS Inc., Chicago, IL, USA) for statistical analysis, along with the Mann-Whitney U test and the Fisher exact test; the significance level was set at P < 0.05.
The 22 type A EA patients who received surgery at our institution comprised 12 male and 10 female patients (ratio, 1.2:1). Except for 1 patient for whom the gestational and birth weights were unknown, the median value for gestational age in the other 21 patients was 37.5 weeks (range, 32-42 weeks) and the median birth weight was 2.5 kg (range, 1.5-3.3 kg). Seven patients (31.8%) were premature babies aged <37 weeks, 11 patients (50%) were low birth weight babies weighing <2.5 kg, and 1 patient was a very low birth weight baby weighing <1.5 kg (Table 1). Among the 22 patients, 14 (63.6%) showed a total of 38 associated anomalies. Cardiovascular malformations accounted for the highest frequency of anomalies (9 patients, 40.9%) (Table 2).
The median gap between the proximal and distal esophagus in all patients was 6 (range, 2-7) vertebral distance (VD).
Among the 22 patients, 10 patients received prenatal diagnosis based on the presence of polyhydramnios and the absence of gastric air shadow on fetal ultrasonography. In cases where type A EA was suspected, the diagnosis was confirmed based on the absence of air shadow on plain abdominal images and the twisting of the gastric tube with a blocked entrance after birth. Twelve patients were diagnosed postnatally; 10 patients showed no gas shadow on the x-ray with a blocked gastric tube entrance after birth, whereas the other 2 patients were diagnosed based on the finding of a barium esophagogram at different institutions. The distance between the both ends of the esophagus was measured by using the VD.
In 1 patient, primary esophageal end-to-end anastomosis was performed because the esophageal end-to-end length was found to be 1.5 VD even when thoracotomy was done without gastrostomy. In the other 21 patients, gastrostomy was priorly performed, whereas 2 patients also underwent cervical esophagostomy, at different institutions, because of severe drooling despite continuous postoperative oral suction. Nasogastric tube insertion was performed through the proximal esophagus at the time of the definitive surgery, and the esophageal end-to-end distance was measured using the radiograph taken with a Hegar dilator in situ in the distal esophagus through the gastrostomy. When the length was less than 4 VD, end-to-end anastomosis was performed; however, if the length was same or more than 4 VD, esophago-gastric tube anastomosis was performed. End-to-end anastomosis of the esophagus was performed in 7 patients after gastrostomy, and esophago-gastric tube anastomosis after gastrostomy was performed in 14 patients.
Of 21 patients, 10 patients were transferred to our institution from other institutions after gastrostomy, whereas the other 11 patients received the procedure at our institution. We performed tube gastrostomy according the Stamm method using a 14-Fr Malecot tube or a silicon-type gastrostomy tube. Gastrostomy was performed in the antrum of the greater curvature of the stomach, considering the possibility that gastric tube replacement would subsequently be performed.
For esophageal end-to-end anastomosis, all procedures were performed in the right fourth intercostal incision, excluding 1 case performed in the thoracoabdominal incision. Intrathoracic anastomosis was performed in all cases. Among these cases, anastomosis was performed in 4 patients by the dissection of the gastroesophageal junction and the stomach fundus using an additional abdominal incision, as the distal esophagus had great tension during anastomosis. In 2 cases, pyloroplasty was performed because of suspected damage to the vagus nerve during surgery. In 2 patients, we attempted to extend the length of the distal esophagus by using bougination through a gastrostomy between the primary gastrostomy and secondary esophageal end-to-end anastomosis procedure.
A gastric tube was created with greater curvature of the stomach by using GIA, and the diameter of the gastric tube was determined on the basis of chest tube (12-20 Fr) depending on the patients' weight (if body weight at operation <2.5 kg, 12 Fr was used; whereas if that ≥2.5 kg, 14 Fr or 20 Fr was used.) An isoperistaltic conduit, which involves the alignment of the gastric tube in the same direction as the gastric peristalsis, was applied in 9 patients, whereas an antiperistaltic conduit, wherein the alignment is in the opposite direction of the gastric peristalsis, was used in 5 patients. In addition, the gastric tube was placed through the mediastinal route in 11 patients; however, in 3 patients, the retrosternal route was used because of a history of operation at the mediastinal area or combined heart disease.
Anastomosis was performed by using a thoracic approach in cases where the esophageal proximal blind pouch was located in close to the carina, or by using the cervical approach in cases where the proximal blind pouch was located in the cervical area or in the thoracic inlet.
Anastomosis of the gastric tube was performed in the thoracic esophagus in 4 patients and in the cervical esophagus in 10 patients. For thoracic anastomosis, the right second intercostal space (ICS) approach was used for 1 patient, whereas the fourth ICS approach was used for 3 patients. Cervical anastomosis was performed by using the left side in 7 patients, the right side in 1 patient, and the previous esophagostomy site in 2 patients. In 3 cases, vagus nerve injury was suspected and pyloroplasty was simultaneously performed.
For the stabilization of the anastomosis site after esophageal end-to-end anastomosis or esophago-gastric tube anastomosis, ventilator care with sedation was maintained for 2 days. After surgery, a nasogastric tube was kept for 7 days, and we checked esophagography on the 7th postoperative day. Food intake was permitted in cases where no leakage was detected. In case food intake was difficult owing to swallowing discoordination or reflux caused by long-term fasting, a nasogastric tube was used to support nutrition and it was kept when the patients were discharged from the hospital. After discharge, they kept feeding via nasogastric tube and they could eat orally without nasogastric tube within postoperative 3-6 months.
The 1 patient who received primary esophageal end-to-end anastomosis without gastrostomy was born in 1980, and is the first such case. This patient was a male who was born at the gestational age of 38 weeks; his birth weight was 2,500 g, and he did not have any associated anomalies. He was transferred to our institution 7 days after birth because of continuous vomiting and pneumonia, where he received esophageal end-to-end anastomosis on the 9th day of birth. His VD was 1.5 and his weight at the time of surgery was 2,610 g.
At the time of gastrostomy, the median age was 1 day (range, 0-9 days). Moreover, the median weight at the time of surgery was 2.4 kg (range, 2.1-3.3 kg), and the median postoperative ICU treatment period was 15 days (range, 4-23 days).
Except for 1 patient who received primary esophageal end-to-end anastomosis, the median age at the definitive surgery was 8 months (range, 4-12 months). The median weight at the time of surgery was 8.2 kg (range, 6.1-12.3 kg), the mean postoperative ICU treatment period was 4 days (range, 1-14 days), and the median interval between primary surgery and definitive surgery was 259 days (range, 145-370 days).
The median follow-up period was 94.5 months (range, 1-316 months) and there were no deaths among the 22 patients during the follow-up period.
Among 21 patients who received gastrostomy, 3 patients (14.3%) had gastrostomy-associated complications. Two patients had gastrostomy malposition, and 1 patient had gastrostomy leakage. All patients underwent gastrostomy revision and showed improvements.
However, complications were noted found in all cases after the definitive surgery. Anastomosis leakage occurred in 3 patients (13.6%). This was found to be mild in 2 patients who recovered after conservative management such as tube feeding and were discharged after oral food intake on the 19th and 29th days after the surgery. However, 1 patient showed signs of mediastinal expansion on the 2nd postoperative day with suspected anastomosis leakage; in this case, we repaired the leakage site after explorative thoracotomy.
Anastomosis stenosis was detected in 9 patients (42.9%). Except for 1 patient who did not have symptoms, EBD was performed in 8 patients with stenosis. EBD was performed repeatedly from 2 to 9 times (average number of times, 4) from the 27th day of the anastomosis. Three of 8 patients who received EBD showed improvement (33.3%); however, 5 patients did not show improvement and required resection of the stenosis area and underwent reanastomosis. Among the 5 patients who received resection of the stenosis area, 2 patients smoothly progressed to meal intake whereas the remaining 3 patients again developed stenosis after surgery and received EBD from 2 to 5 times; at present, they are on a normal diet without any problems.
GER was observed in 20 patients (90.9%). The symptoms were severe in 1 patient, and Nissen fundoplication and pyloroplasty were performed. Nineteen patients showed mild to moderate symptoms and received conservative treatment such as medication therapy. During the follow-up period, 11 patients did not experience any reflux symptoms and 11 patients showed mild symptoms such as intermittent coughing after overeating or at night.
In addition, complications such as pleural effusion, wound infection, pneumonia, esophageal hiatal hernia, delayed gastric emptying, cardiac arrest, ileus, and dumping syndrome were observed. Ileus, pleural effusion, delayed gastric emptying, and dumping syndrome improved with conservative management, whereas esophageal hiatal hernia is being observed through the outpatient clinic as it is asymptomatic.
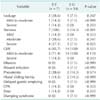
The median gap was 3 VD for the E-E group and 6 VD for the E-G group, with the E-E group showing a significantly short gap. There was no significant difference between the 2 groups with regard to patient demographics, weight, and age at the time of surgery (Table 3).
No significant difference was noted between the 2 groups with regard to anastomosis leakage. Stenosis was found to develop more frequently in the E-E group than in the E-G group (P = 0.001). In particular, severe stenosis occurred in 57.1% of patients in the E-E group, which was significantly higher than that in the E-G group.
In addition, GER was found to develop more frequently in the E-G group than in the E-E group, but the difference was not statistically significant. In the E-G group, GER occurred in all patients (Table 4).
No significant difference was noted between the 2 groups with regard to the other complications. Among the patients in the E-G group, when comparing the patients according to the use of an isoperistaltic tube or an antiperistaltic tube, no difference was noted in the frequencies of leakage, postoperative stenosis, or GER (Table 5).
Type A EA is characterized by a wide interval between the proximal and distal esophageal blind ends, which makes primary anastomosis difficult [4]. According to Humphreys and Ferrer Jr [5], the first case with a successful surgery of type A EA was in 1946. The baby was born in 1935 and was survived with maintaining food intake via gastrostomy [5].
In type A EA, primary anastomosis is possible if the gap between both esophageal ends is short; however, in cases with a wide gap, esophageal reconstruction is performed by using various organs.
Since Howard and Myers [6] performed successfully delayed esophageal end-to-end anastomosis by expanding the upper esophagus with a mercury bougie for 5 weeks, delayed esophageal end-to-end anastomosis after upper esophagus expansion had been performed until the late 1970s. Thereafter, esophageal end-to-end anastomosis as a delayed procedure has been performed widely for its physiological approach, postoperative functionality, and high patient satisfaction.
Despite a slight abnormality in the peristalsis of the esophagus, conservation of the native esophagus has been preferred as it is the best conduit in itself [7]. In addition, as the physiological function and structure of the esophagus are conserved as much as possible for patients who received primary end-to-end anastomosis, it has been reported that superior prognosis is noted in terms of function related to swallowing and GER [1]. Maksoud-Filho et al. [1] also reported that the long-term prognosis was good in terms of swallowing and GER for patients in whom the esophagus was conserved.
After 12 weeks from the birth, it is reported that esophageal end-to-end anastomosis could be successfully performed by complete dissection around the esophagus, maintenance of ventilator care, and circular muscle resection in order to avoid excessive tension after surgery [7]. In the initial period after birth, the growth of the esophagus is fast and secondary GER or the stenosis caused by this reflux can be medically treated. It has been argued that the esophagus with anastomosis does not show the abnormal mucosal lesion that in observed in other reconstructive operations, and follow-up shows good functional outcomes [8].
However, conserving the native esophagus in EA patients with long gaps is not always feasible. In that case, end-to-end esophageal anastomosis can cause high perioperative complications. Therefore, it is necessary to reduce the tension and facilitate the surgical process by creating a "conduit" [9]. In other words, after creating and developing an esophagostomy and gastrostomy, esophageal replacement using other structures, such as the colon, stomach, small intestine, and the damaged part of the esophagus, is performed [8].
Esophageal replacement with the colon has been widely performed until the late 1980s, as the procedure was easy to perform. Postoperative leakage of esophago-colon anastomosis occurred in 30%-50% patients, and accompanied various complications such as anastomosis stenosis, sagging and stasis of the intrathoracic dislocated colon, and necrosis of the bowel segment [8]. Recently, stomach replacement has been widely used, and Spitz et al. [10] has argued that this procedure is desirable as it has higher patient satisfaction and lower rate of postoperative complications than the colon replacement method. However, careful monitoring is necessary for the early diagnosis of postoperative esophagitis, Barrett's changes, and atrophic gastritis. In some cases, it has been argued that using the stomach route in EA is preferable, as the blood flow is sufficient and the length can be measured; moreover, there is an original resistance to acid and the ability to maintain the shape of the tube without separate expansion [11]. Reconstructive surgery using the small intestine includes the Roux-en-Y method or the transposition method with a small intestine graft by using microvascular anastomosis; however, this is rarely performed in children due to the unstable vascular connection created after anastomosis [12]. Various esophageal replacement surgeries can reduce esophageal stenosis and GER by reducing the postoperative tension in the anastomosis site; however, they are time consuming, complex, and may result in the expansion and change in the shape of the organ, as well as ulcers or bleeding due to reflux [13].
The need for esophageal replacement by using a conduit and end-to-end anastomosis is determined depending on the gap between the esophageal ends; however, identifying the esophageal gap is difficult. At the time of EA diagnosis, the location of the proximal esophagus can be predicted roughly by means of x-ray images, on the basis of the location of the Levin tube; however, the location of the distal esophagus cannot be identified accurately despite the use of ultrasonography. Even if the VD was identified in the combination of ultrasonography and the gastrography with contrast via gastrostomy, most cases show discrepancies with actual surgical findings [7]. In this study, we attempted to identify the location of the distal esophagus by using a metal probe via gastrostomy before surgery, and this provided a more accurate assessment of the location than the gastrostomy tube contrast method before surgery, and also matched the findings confirmed during surgery. Therefore, we suggest using a metal probe in order to accurately identify the location of the distal esophagus.
Among the 22 patients examined in this study, 1 patient who received the first surgery in 1980 underwent esophageal end-to-end anastomosis without bridge operation, whereas the other 21 patients all received primary gastrostomy. The VD of the E-E group and the E-G group were 3 and 6, respectively, with the E-E group showing a significantly short gap. The results of this study indicate that, in the case of type A EA, definitive surgery is considered if the weight is approximately 9 kg at 8-9 months after the primary gastrostomy, and the decision of whether to perform end-to-end anastomosis or esophago-gastric tube anastomosis should be based on the VD at the time of the definitive surgery.
Postoperative complications mostly involve anastomosis [14,15]. According to a previous study, anastomosis leakage, anastomosis stenosis, GER, repeated pneumonia, and sepsis with GER accounted for most of the cases of complications [16].
Anastomosis leakage has been reported to occur in 37.5%-45.0% of patients [17]. The factors involved in anastomosis leakage include the use of silk sutures, anastomosis tension, ischemia due to an excessive dissection in the distal esophagus, and technical failure [18]. Anastomosis leakage is an important complication directly associated with death. In the cases of mild leakage, conservative treatment can include parenteral nutrition with antibiotics under fasting conditions; however, in cases where leakage is severe, appropriate drainage is most important [19]. Rescorla et al. [20] reported that approximately 50% of patients from the esophageal end-to-end anastomosis group showed anastomosis leakage but spontaneous recovery was noted after conservative treatment. The leakage rate in this study was 13.6%, which is lower than that reported in previous studies. In addition, there was no statistical significance as it occurred in 28.6% of the group receiving end-to-end anastomosis or in 7.1% of the esophago-gastric tube anastomosis group, with a slightly higher tendency in the end-to-end anastomosis group. This result supports previous findings that esophageal replacement with gastric tube helps in reducing tension in anastomosis and lowers anastomosis leakage by sufficiently adjusting the length and allowing for good blood flow compared with replacement with other organs.
Chun and Kim [21] reported that anastomotic stenosis occurred in 52.2% of type A EA surgeries, which mostly improved after EBD or bougination, including some cases requiring reoperation. The use of silk sutures, one-sided anastomosis, anastomosis tension, the experience of the surgeon, anastomosis leakage, and GER can also be factors causing stenosis [22]. In this study, anastomotic stenosis occurred in 47.6% of patients, similar to the frequency reported by previous studies [23]. In the comparison of the E-E group and the E-G group, stenosis occurred more frequently in the E-E group with statistical significance, and severe stenosis also occurred significantly more often in the E-E. This suggests that, in order to avoid stenosis, the method should be selected to ensure maintenance of blood flow and reduction of tension.
Since the first report of its use in a pediatric patient in 1984, the use of a balloon catheter for the treatment of esophageal stenosis has been performed [24]. According to previous reports [25,26], the success rate of EBD was 93%-97%; however, the success rate in this study was 33.3%, and surgical treatment was performed when the patient showed no response to EBD [27].
GER is reported to be the most common complication [3]. Burjonrappa et al. [28] reported that collapse of abdominal antireflux mechanism and distal esophageal motor function occurred if the distal esophagus is pulled excessively during anastomosis. Abnormality in the vagus nerve, reduction in the intra-abdominal esophagus due to excessive mobilization, anastomosis with tension, and abnormal peristalsis of the esophagus have been reported to be factors associated with GER [27].
Postoperative GER occurs in 18%-70% of cases [29]. Patients with GER require EBD because of the risk of a secondary occurrence of anastomotic stenosis [27]. In case no response is seen after antireflux medical treatment, fundoplication or temporary stent insertion is required [29], and EBD is very rarely required for symptom relief after the surgery [27].
Although GER occurred in almost all patients in this study (90.9%), the percentage of which was higher than that reported previously, the proportion of cases requiring surgery was rather lower at 10% and most cases showed improved symptoms with medical treatment. This may be a result of the initiation of active treatment following the identification of mild GER during follow-up. As GER can make oral intake difficult and cause repeated aspiration pneumonia, it needs to be controlled for improving the quality of life through close follow-up with endoscopy [30]. In addition, although no statistically significant difference was observed between the E-E and the E-G group, GER occurred in all the patients in the E-G group. Moreover, no difference in GER was noted despite the change in conduit from isoperistaltic to antiperistaltic. This is believed to be due to the disappearance of the existing esophageal area after the surgery, and appropriate treatment is necessary for GER when a replacement procedure is performed.
In conclusion, type A EA accounted for approximately 13.4% of all EA cases. Depending on the length of the end-to-end interval, the treatment for type A EA was carried out by performing esophageal end-to-end anastomosis or esophago-gastric tube anastomosis after gastrostomy performed immediately after birth.
On comparing the patients who received esophageal end-to-end anastomosis and esophago-gastric tube anastomosis, stenosis occurred significantly more often in the end-to-end anastomosis group; however, no difference was noted between the 2 groups with regard to leakage and GER. Therefore, appropriate tension in the anastomosis site and appropriate blood flow in the esophagus are key factors for preventing postoperative stenosis and leakage, and esophageal replacement is believed to be a feasible and safe procedure in cases where excessive tension is present.
Figures and Tables
References
1. Maksoud-Filho JG, Goncalves ME, Tannuri U, Maksoud JG. An exclusively intraabdominal distal esophageal segment prevents primary delayed anastomosis in children with pure esophageal atresia. J Pediatr Surg. 2002; 37:1521–1525.
2. Guo W, Fonkalsrud EW, Swaniker F, Kodner A. Relationship of esophageal anastomotic tension to the development of gastroesophageal reflux. J Pediatr Surg. 1997; 32:1337–1340.
3. Puri P, Blake N, O'Donnell B, Guiney EJ. Delayed primary anastomosis following spontaneous growth of esophageal segments in esophageal atresia. J Pediatr Surg. 1981; 16:180–183.
4. Sanal M, Haeussler B, Tabarelli W, Maurer K, Sergi C, Hager J. Pure esophageal atresia with normal outer appearance: case report. J Pediatr Surg. 2007; 42:E1–E3.
5. Humphreys GH, Ferrer JM Jr. Management of esophageal atresia. Am J Surg. 1964; 107:406–411.
6. Howard R, Myers NA. Esophageal atresia: a technique for elongating the upper pouch. Surgery. 1965; 58:725–727.
7. Seguier-Lipszyc E, Bonnard A, Aizenfisz S, Enezian G, Maintenant J, Aigrain Y, et al. The management of long gap esophageal atresia. J Pediatr Surg. 2005; 40:1542–1546.
8. Kim SM, Choi SH, Kim SH, Kwon IK, Han SJ, Oh JT. Esophageal atresia without tracheoesophageal fistula: report of 6 cases. J Korean Assoc Pediatr Surg. 2005; 11:157–164.
9. Ahmad SA, Sylvester KG, Hebra A, Davidoff AM, McClane S, Stafford PW, et al. Esophageal replacement using the colon: is it a good choice? J Pediatr Surg. 1996; 31:1026–1030.
10. Spitz L, Kiely E, Sparnon T. Gastric transposition for esophageal replacement in children. Ann Surg. 1987; 206:69–73.
11. Anderson KD, Randolph JG. Gastric tube interpostion: a satisfactory alternative to the colon for esophageal replacement in children. Ann Thorac Surg. 1978; 25:521–525.
12. Saeki M, Tsuchida Y, Ogata T, Nakano M, Akiyama H. Long-term results of jejunal replacement of the esophagus. J Pediatr Surg. 1988; 23:483–489.
13. Lam KH, Lim ST, Wong J, Lam SK, Ong GB. Gastric histology and function in patients with intrathoracic stomach replacement after esophagectomy. Surgery. 1979; 85:283–290.
14. Chittmittrapap S, Spitz L, Kiely EM, Brereton RJ. Anastomotic leakage following surgery for esophageal atresia. J Pediatr Surg. 1992; 27:29–32.
15. Holder TM, Cloud DT, Lewis JE Jr, Pilling GP 4th. Esophageal atresia and tracheoesophageal fistula: a survey of its members by the surgical section of the American Academy of Pediatrics. Pediatrics. 1964; 34:542–549.
16. Bagolan P, Iacobelli Bd Bd, De Angelis P, di Abriola GF, Laviani R, Trucchi A, et al. Long gap esophageal atresia and esophageal replacement: moving toward a separation? J Pediatr Surg. 2004; 39:1084–1090.
17. Ein SH, Shandling B, Heiss K. Pure esophageal atresia: outlook in the 1990s. J Pediatr Surg. 1993; 28:1147–1150.
18. Chun YS, Jung SE, Lee SC, Park KW, Kim WK. Seventeen year's experience with ninety-six esophageal atresia. J Korean Assoc Pediatr Surg. 1995; 1:140–148.
19. Cho SH, Oh BS, Lee DJ. End to end anastomosis of type A(long gap) esophageal atresia in 1200 gram premature baby: a case report. Korean J Thorac Cardiovasc Surg. 1997; 30:236–240.
20. Rescorla FJ, West KW, Scherer LR 3rd, Grosfeld JL. The complex nature of type A (long-gap) esophageal atresia. Surgery. 1994; 116:658–664.
21. Chun YS, Kim WK. Surgeon's technique and anastomotic stricture after repair of esophageal atresia. Inje Med J. 2002; 23:263–268.
22. Holder TM, Ashcraft KW, Sharp RJ, Amoury RA. Care of infants with esophageal atresia, tracheoesophageal fistula, and associated anomalies. J Thorac Cardiovasc Surg. 1987; 94:828–835.
23. Puri P, Ninan GK, Blake NS, Fitzgerald RJ, Guiney EJ, O'Donnell B. Delayed primary anastomosis for esophageal atresia: 18 months to 11 years follow-up. J Pediatr Surg. 1992; 27:1127–1130.
24. Ball WS, Strife JL, Rosenkrantz J, Towbin RB, Noseworthy J. Esophageal strictures in children. Treatment by balloon dilatation. Radiology. 1984; 150:263–264.
25. Said M, Mekki M, Golli M, Memmi F, Hafsa C, Braham R, et al. Balloon dilatation of anastomotic strictures secondary to surgical repair of oesophageal atresia. Br J Radiol. 2003; 76:26–31.
26. Lang T, Hummer HP, Behrens R. Balloon dilation is preferable to bougienage in children with esophageal atresia. Endoscopy. 2001; 33:329–335.
27. Parolini F, Leva E, Morandi A, Macchini F, Gentilino V, Di Cesare A, et al. Anastomotic strictures and endoscopic dilatations following esophageal atresia repair. Pediatr Surg Int. 2013; 29:601–605.
28. Burjonrappa S, Thiboutot E, Castilloux J, St-Vil D. Type A esophageal atresia: a critical review of management strategies at a single center. J Pediatr Surg. 2010; 45:865–871.
29. Antoniou D, Soutis M, Christopoulos-Geroulanos G. Anastomotic strictures following esophageal atresia repair: a 20-year experience with endoscopic balloon dilatation. J Pediatr Gastroenterol Nutr. 2010; 51:464–467.
30. Sri Paran T, Decaluwe D, Corbally M, Puri P. Long-term results of delayed primary anastomosis for pure oesophageal atresia: a 27-year follow up. Pediatr Surg Int. 2007; 23:647–651.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download