Abstract
Purpose
The consumers' preferences are not considered in developing or implementing new medical technologies. Furthermore, little efforts are made to investigate their demands. Therefore, their preferred surgical method and the factors affecting that preference were investigated in pancreatic surgery.
Methods
Six-hundred subjects including 100 medical personnel (MP) and 500 lay persons (LP) were surveyed. Questionnaire included basic information on different methods of distal pancreatectomy; open surgery (OS), laparoscopic surgery (LS), and robotic surgery (RS). Assuming they required the operation, participants were told to indicate their preferred method along with a reason and an acceptable cost for both benign and malignant conditions.
Results
For benign disease, the most preferred method was LS. Limiting the choice to LS and RS, LS was preferred for cost and well-established safety and efficacy. OS was favored in malignant disease for the concern for radicality. Limiting the choice to LS and RS, LS was favored for its better-established safety and efficacy. The majority thought that LS and RS were both overpriced. Comparing MP and LP responses, both groups preferred LS in benign and OS in malignant conditions. However, LP more than MP tended to prefer RS under both benign and malignant conditions. LP thought that LS was expensive whereas MP thought the cost reasonable. Both groups felt that RS was too expensive.
Technology is rapidly evolving, and many aspects of our lives are affected by such technological changes. Field of medicine is not an exception. Advances in medical technology and equipment have led modern surgery into an era of minimally invasive surgery. Since the first introduction of laparoscopic surgery (LS) in 1987 [1], its application has expanded from gallbladder to various organs. With increasing reports on technical feasibility and comparable oncologic outcomes [2], the indications of LS are expanding. Whereas LS was initially limited mainly to benign diseases, the indication is expanding to malignant diseases in certain organs such as stomach, colon, gallbladder, and liver [3-6].
Despite the expanding turf of LS, there are still application limitations due to the restricted degrees of freedom of equipment manipulation and to the two-dimensional endoscope images [7]. To overcome some of the shortcomings of LS and to augment its usefulness, robot-assisted surgery (RS) was introduced in the late 1990s, and is being further developed [8]. Even before RS, which is thought to be still in its infancy, becomes recognized as an established surgical method, natural orifice transluminal endoscopic surgery (NOTES) is making its way into clinical practice [9]. Such changes indicate the rapid pace of evolution in medical technology.
Korean surgeons have been actively engaging in RS. Asia's very first RS was performed in Korea in 2005, and based on statistics reported in 2010, the largest number of da Vinci Surgical Units in Asia are located in Korea. Of the countries currently holding such units, Korea ranks fifth in the world. Furthermore, with regard to per capita distribution of da Vinci surgical units, Korea ranks 3rd among the world's nations with approximately 0.60 units per million citizens [10].
In the field of pancreatic surgery, the introduction of these newer technologies has been relatively slow compared to other organs due to the anatomic complexities and relative higher complication risks. In spite of that slowness, the application of these technologies is quickly spreading and many surgeons are making an effort to expand its applications and indications. With increasing reports of comparable safety and feasibility of LS and RS to that of open surgery (OS) in distal pancreatectomy, laparoscopic and robot-assisted distal pancreatectomies are being increasingly performed.
The development of the technologies and techniques are being led by health care providers and medical industries. Moreover, indication and selection of the method of pancreatic surgery are mostly dependent on health care providers' decisions. However, a health care provider's decision may be influenced by diverse factors including personal tendency, national sociopolitical barriers to application of a new medical technology, and national medical cost policies. Thus, it seems unlikely that the perceptions and demands of medical consumers are being reflected in the technological evolution of surgery and in selection of surgical methods.
This study aims to investigate the preferences of potential medical consumers on pancreatic surgical methods. In addition, factors influencing such preferences are evaluated. Thereby, enable the primary developers and health care providers to step closer to the perceptions and demands of patients.
A questionnaire to investigate surgical method preference was developed by the Hepatobiliary and Pancreas Surgery Division of Department of Surgery at Seoul National University Hospital. Institutional Review Board approval was obtained and the questionnaire-based survey was conducted between July and November 2011. The questionnaires were distributed by personal contact, mail, or via the internet.
The questionnaire consisted of three sections. Section 1 anonymously collected basic demographic information such as sex, age group, education level, socio-economic status, and profession (Supplementary questionnaire section 1). Section 2 presented basic information about distal pancreatectomy along with brief summaries of OS, LS, and RS (Supplementary questionnaire section 2). Pros and cons of the three operations, in terms of complication rate, safety and technical establishment, radicality, cosmesis, pain, recovery, and costs, were also provided. Section 3 described a scenario in which the participant hypothetically requires a distal pancreatectomy for a benign pancreatic disease (Supplementary questionnaire section 3).
In that section, the first question asked the participants to rank OS, LS, and RS in their order of preference. The participants were then asked to choose the main reason for their surgical preference in the previous question. The second question asked the participants to choose between LS and RS only, and to provide their reason for that choice. The third question asked for the participant's opinion of a reasonable cost for LS and RS. Similar questions, but with regard to a scenario in which the participant hypothetically has a malignant pancreatic disease, were asked in the second part of section 3 of the questionnaire.
Among 600 participants, 500 were lay persons (LP) and 100 were medical personnel (MP). The latter included 50 medical doctors and 50 nurses. The medical doctors were mainly general surgeons (32%) and the others were from various departments such as plastic surgery, internal medicine, and orthopedic surgery. For 500 LP, the responses were obtained through personal contact in 110 participants and through internet survey in 390 participants. For MP, responses of 84 participants were through personal contact and 16 were through mail. The survey was requested to a total number of 20,210 subjects. Of these subjects, 993 decided to participate (4.9%) and 600 participants successfully completed the survey (3.0%).
Descriptive statistics for quantitative variables and frequencies with percentage were calculated. For comparative analysis between LP and MP, chi-square tests, Student t-tests, and analysis of variance were performed. The P-value of less than 0.05 was considered significant. All mean values are described as mean ± standard error of mean.
Reliability and validation analyses of survey were performed by randomly sampling 60 participants and asking them to complete the survey questionnaire a second time, approximately 3 weeks after completion of the first questionnaire. To test reliability, kappa (κ) indices were calculated for questions with two categories and weighted κ indices were calculated for questions with more than three categories [11]. When the κ index was above 0.600, reliability was interpreted to be "substantial" to "almost perfect", and κ index between 0.001 and 0.400 was interpreted to have "fair" or "slight" reliability [12].
No previous survey was available that could be used as a gold standard by which the validity of the present survey could be evaluated. Therefore, a reliability index, obtained by using a test-retest method, was used to estimate the validity coefficient. As the equality of variance of the measured error could not be assumed, the validity range was calculated as below [13].
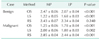
Of the 600 participants responding to the surgery, 57.8% were female and 42.2% were male. The participants' ages showed a normal distribution with the 4th decade being the median age group. Most of the participants had received at least a higher education (n = 537, 89.5%). The economic status responses revealed that the majority of participants (77.1%) were from the middle class earning between 20,000 and 80,000 USD annually (Table 1).
In the case of participants with hypothetical benign condition, 52.2% (313/600) chose LS as the most preferred method. OS and RS were preferred by 28% and 20%, respectively (Fig. 1). The mean rank for LS was the lowest (1.56 ± 0.03) whereas the mean ranks for OS and RS were 2.13 ± 0.03 and 2.36 ± 0.03, respectively. In contrast, the most favored method was OS (56.2%, 337/600) followed by LS (28.2%) and RS (15.7%) in the case of participants with a hypothetical malignant condition (Fig. 1). The mean ranks were 1.69 ± 0.04, 1.84 ± 0.03, 2.51 ± 0.03 for OS, LS, RS, respectively. There were significant differences between benign and malignant conditions, in terms of the proportions of preferences (P < 0.001) and the mean ranks of OS, LS, and RS (P < 0.001, P < 0.001, and P = 0.001, respectively).
The main factors that influenced the participants' decisions in the case of a benign disease were radicality (33.7%) and safety (33.0%) (Fig. 2). Compared to the benign scenario, the malignant disease results showed that radicality had a greater influence as 56.2% of participants felt it to be the most important factor. The influence of safety came behind radicality with 26.7% (Fig. 2).
When participants were only given a choice between LS and RS, 75.2% of respondents with a hypothetical benign disease chose LS over RS. Cost was the predominant reason for that choice (40.2%) followed by established safety and efficacy (31.3%). In the hypothetical malignant disease scenario, LS was favored by 69.7% of the participants. As in the case of benign disease, the two main reasons for the choice were established safety and efficacy (47.2%) followed by cost (28.8%).
Of the 600 participants, 56.2% thought that LS was currently too expensive. Of the respondents, 95.7% found the cost of RS too expensive and more than half of them indicated that the cost should be less than half of the present cost. As in the benign case, 98.3% of the participants with a hypothetical malignant disease believed that RS was too expensive and 54.7% replied that its cost should be less than half of the current cost.
Among the participants with a hypothetical benign disease, LS was the most preferred method by both MP and LP. However there were several significant differences between the two groups. There was a marked difference in the distribution of preference between the two types of participants (P < 0.001) (Fig. 3A). The preference of MP was predominantly LS (82.0%) with only a small portion of MP participants choosing OS and RS (8% and 10%, respectively). In contrast, although LS was the most preferred method (46.2%), the decisions were relatively dispersed with 31.6% for OS and 22.2% for RS in LP participants. The mean LS rank was significantly lower in the MP group than in the LP group (1.22 ± 0.06 vs. 1.68 ± 0.04, respectively, P < 0.001), while that of OS was significantly higher in the MP group compared to that of LP (2.47 ± 0.06 vs. 2.07 ± 0.04, respectively, P < 0.001). However, the mean RS ranks did not differ between MP and LP participants (2.43 ± 0.07 vs. 2.34 ± 0.04, respectively, P = 0.240) (Table 2).
Among MP, the main reasons for the surgical preference were safety followed by radicality (34.0% and 26.0%). Among LP, radicality was the most important factor followed by safety (35.2% and 32.8%). More participants in MP found cosmesis an important issue than LP (23.0% vs. 8.6%, P < 0.001), whereas cost was more influential to LP than MP (11.4% vs. 4.0%, P = 0.028) (Fig. 4A).
In a choice between LS and RS, the majorities of MP and LP preferred LS (91.0% and 72.0%, respectively). Significantly more LP participants than MP participants chose RS (28.0% vs. 9.0%, P < 0.001). In both groups, the main reason for the choice was related to cost (44.0% and 39.4% for MP and LP, P = 0.434) and established safety and efficacy (24.0% and 32.8% in MP and LP, P = 0.098). LP participants had a marginally higher expectations for new technology than MP participants (14.2% vs. 7.0%, P = 0.051). In contrast, a larger portion of MP than LP indicated a reluctance for undergoing RS, owing to the uncertainty associated with the new technology (23.0% vs. 13.4%, P = 0.021).
The majority of MP (52.0%) indicated that the current cost of LS was reasonable while 63.1% of the LP participants thought that LS should be less expensive. Although there was a significant difference between the two groups (P < 0.001), the majority of both MP and LP participants responded that the cost of RS should be lower (87.0% and 97.4%, respectively).
MP overwhelmingly preferred OS (83.0%) over LS (16.0%) and RS (1.0%) (Fig. 3B). Even though the LP's first choice was also OS (50.8%), the preferred choices were rather dispersed to LS (30.6%) and RS (18.6%). The preference difference between MP and LP was statistically significant (P < 0.001) (Fig. 3B). The mean rank assigned by MP participants, in comparison to LP participants, was significantly lower for OS (1.25 ± 0.06 vs. 1.78 ± 0.04, respectively, P < 0.001), and significantly higher for LS (2.00 ± 0.06 vs. 1.80 ± 0.03, respectively, P = 0.002) and for RS (2.85 ± 0.04 vs. 2.44 ± 0.04, respectively, P < 0.001) (Table 2).
The most important considerations were radicality and safety in both groups (MP, 81.0% and 17.0%; LP, 51.4% and 28.6%) as illustrated in Fig. 4B.
In restricted choice between LS and RS, 82.0% of MP participants and 67.2% of LP participants chose LS. However, LP showed a greater preference than MP participants for RS (30.4% vs. 14.0%, respectively, P = 0.003). Important factors affecting those preferences were established safety and efficacy (MP, 51.0%; LP, 46.6%) and cost (MP, 22.0%; LP, 30.3%); and those results did not differ significantly between MP and LP (P = 0.085). As in the cases of a hypothetical benign disease, LP had a greater expectations than MP for new technology (10.8% vs. 7.0%, respectively, P = 0.282), and MP tended to have a greater concern about the uncertainty of new technology than LP with marginal significance (19.0% vs. 12.0%, P = 0.074).
Even in the case of a hypothetical malignancy, the predominant opinion of both MP and LP on RS cost was that it was too expensive (82.0% and 97.6%, respectively). However, significantly more MP compared to LP thought that the cost of RS was either reasonable or should cost more (18.0% vs. 2.4%, respectively, P < 0.001).
Based on the obtained κ indices, the reliabilities of responses to most of the questions were found to be substantial to almost perfect. The reliability coefficient (κ index or weighted κ index) ranged from 0.603 to 0.912 for most questions. There were almost perfect agreement questions about the rank of RS in both benign (0.871) and malignant cases (0.912), as well as for the questions about choosing between LS and RS in the benign case (0.889).
On the other hand, four questions demonstrated relatively low reliability (κ < 0.500). Those four questions were about the reason for selecting the preferred method in the benign scenario (κ = 0.467), the reason for the choice between LS and RS in both the benign (κ = 0.388) and malignancy (κ = 0.481) scenarios, and the question about the acceptability of the cost of RS in the malignancy scenario (κ = 0.465).
Estimates of the validity coefficient ranged from 0.388-0.623 to 0.912-0.955 depending on the question. The coefficients indicate that the survey, in general, may be considered reliable and valid, but the survey could still be improved with further adjustments. The reliability and validity index are summarized in Table 3.
The application of LS and RS to the pancreas was relatively slow, but the surgical evolution did not circumvent the organ. Laparoscopic distal pancreatectomy and laparoscopic pancreaticoduodenectomy were first reported in the early 1990s [14], and robot-assisted pancreatic surgery was introduced about 10 years later [15,16]. With accumulated evidence, the safety and effectiveness of laparoscopic distal pancreatectomy is now widely accepted in benign and borderline lesions. With regard to pancreaticoduodenectomy, the safety and feasibility have been reported but the results are probably applicable to only a few expert surgeons [17]. Even before the acceptance of LS as an established method in pancreatic surgery, robot-assisted pancreatic surgery was introduced and is now being performed more frequently. Robot-assisted pancreatic surgery has theoretical advantages but objective and concrete evidences on the safety and effectiveness are lacking, and more evaluations are needed. A study comparing robot-assisted pancreatic surgery and conventional LS did not show compelling evidence of cost-effective advantages of RS [18]. Even so, studies into applicability and safety of NOTES in pancreatic surgery are currently in progress [19].
However, it must be noted that such technological developments require large expenditures of resources, including human resources, financial resources, and time. Moreover, after such a development, additional resources are needed to validate the new method. Successful establishment of novel technology is not guaranteed. Therefore, in order to reduce wasted resources and to distribute resources more effectively, the blind pursuit of high technology should be discouraged. Instead, greater attention should be paid to the demands of customers. The Korean National Evidence-based Healthcare Collaborating Agency [10] concluded that the use of RS is expanding in Korea despite a lack of evidence establishing its safety and effectiveness. Among the many reasons for the increase in RS is the indiscreet use of RS in cases with unverified indications. Such use may be due to a lopsided selection of surgical method based on the convenience and/or skewed attitude of surgeon, or it may be due to biased information delivered to a patient by medical professions. The over-expanding tendency to use RS is not only an issue limited to Korea, but rather it appears to be a world-wide problem. We believe that our study will help address this issue by providing suggestions for the effective distribution of resources in pancreatic surgery by examining the preference of medical consumers.
This survey investigated perceptions about and preferences for pancreatic surgical methods by asking participants to hypothesize about a disease that would require a distal pancreatectomy. The reason for assuming distal pancreatectomy instead of pancreaticoduodenectomy was that a distal pancreatectomy may be easier for LP and a nonsurgeon MP to understand. Also, using a hypothetical situation may induce participants' to under-appreciate the highly technical demand of the pancreatic surgery and underestimate the graveness of the potential complications related to pancreaticoduodenectomy, both of which could produce misleading results. In addition, the safety and efficacy of laparoscopic and robot-assisted pancreaticoduodenectomies need further investigation. The survey asked nearly identical questions regarding surgical methods for both benign and malignant scenarios. This was because the nature of disease should influence the decision-making process.
The results demonstrated that LS was the most preferred method in the case of a benign disease, while OS was the most preferred method in malignant disease cases. Although there were differences in proportion of responses, radicality was the most important issue and safety the second most important in both conditions. The benefits of minimally invasive surgery such as cosmesis, less pain, and faster recovery were relatively minor issues to the participants. We speculate that these minor issues will affect the surgical preference only when there is equivalence of radicality and safety between the methods.
Another important finding was that given a choice between LS and RS, LS surgery was the method of choice in both benign and malignant conditions. Although, their priority changed according to the nature of the disease, cost and established safety and efficacy were the two most important considerations indicating that these are the most important issues that need to be settled for RS. Further inquiry into the matter of cost revealed that over half of the participants responded that the cost should be less expensive than its current cost. As for RS, the majority believed that it was too expensive. Even assuming established safety and efficacy of RS, over 98% of participants indicated that the cost should be lower. In this study, the cost was calculated only for procedure fee, equipment, and a 1-week admission fee. RS was 4.91 times more expensive than OS, and 2.69 times that of LS. This obviously may vary according to the national policies on medical costs or the health insurance system of each country. Even so, in a review of the published cost-studies of RS, Barbash and Glied [20] reported that additional costs were generated by various degree when RS was performed compared with standard surgery.
An additional analysis on responses with regards to economic and education status was done (results not shown). In benign conditions, LS was preferred the most regardless of economic and education status (except for those who only received elementary education). The higher economic and educational status population tended to prefer LS over OS and RS far more than the lower populations. The difference was insignificant according to the economic status (P = 0.281) but was significant for educational status (P = 0.019). OS was the most preferred method in malignant conditions. The preference for OS was relatively higher for higher economic and educational status population (P = 0.055 for economic status and P = 0.017 for educational status). With the choice of LS and RS only, LS was more preferred in both benign and malignant conditions. There was no difference according to the economic status (P = 0.259 in benign and P = 0.749 in malignant). But it was interesting that lower educated tended to prefer RS more than LS (P = 0.004 in benign and P < 0.001 in malignant). The trends of response were similar according to the economic and education status. This is probably due to the confounding effect of education and economic status. But statistical significances were found in analysis by the educational status, and therefore this may suggest that the degree of education affect the preference of the participants with higher impact.
A comparative analysis of MP and LP showed some interesting differences. The first notable difference was the relatively dispersed distribution of preferences among LP compared to the more converged method preference of MP. Among MP, LS was the dominant choice in the case of a benign disease while OS was dominant in the case of a malignant disease. As in MP, LS and OS were the preferred choice in both of benign and malignant disease cases in the opinion of LP participants. However, the results for the most preferred method was barely over 50%. The possible reason for such a result may be due to a difference between the two groups in terms of medical knowledge and the information they behold. Even though written information was provided, the level of understanding may be different for LP and MP. Moreover, MP may be biased due to preformed concept from the structured medical education that they received.
Another significant difference was that more LP participants preferred RS in both benign and malignant disease cases. Moreover, LP had a greater expectation of the new technology in both benign and malignant scenarios. Interestingly, MP had a greater level of concerns than LP about RS due to uncertainty about the new technology.
Finally, even though MP results indicated they were slightly more generous about the current cost of the operations, the majority of MP agreed that the cost should not be any more expensive than the current cost of LS. Almost 90% of MP found the cost of RS too expensive and thought it should be less expensive.
In summary, potential medical consumers, regardless of their profession, prefer LS for a benign disease and OS for a malignant disease. This preference is based on the difference in radicality and safety of the two surgical methods. In a choice between LS and RS, LS was preferred in both benign and malignant disease cases by both MP and LP. In making their choice, the participant's major concerns were cost and the establishment of safety and efficacy.
There are some limitations to this study. First, although reliability and validity of the questionnaire was generally acceptable, four questions need to be modified to improve the reliability. However, modifying questions that ask for reasons is not simple as a complex interaction among multiple factors is probably involved in such question. In contrast, the question about surgical cost may be easily improved by reducing the number of categories from which to choose. A second limitation is whether participants well-understood the issue. The pancreas is a complex organ and even MP may find some aspects of it difficult to understand. Although we tried to make the questionnaire as easy and simple as possible, many participants may have found some questions difficult. Lastly, although MP were included in order to compare their perspectives with those of LP, the inclusion of MP may have biased the overall results. In order to minimize that potential bias, we limited the number of MP to 1/6 of the total participants. In addition, the results were separately analyzed for MP and LP. Despite these limitations, this study provides important information on surgical preferences from a hypothetical consumer's point of view.
Medical science could not have reached its current status if it were not for pioneers in technology among many other things. In addition, further developments may result in revolutionary progress of medical science over the long term. Therefore, development of novel technologies and continuing efforts to expand indications of new techniques should be encouraged. However, enormous amount of resources are involved in such development; therefore, carefully planned distribution is needed to avoid excessive diversion of resources that could be used to provide optimal and satisfactory management for present-day patients. Thus, expansion and development efforts should be modulated so that existing resources are well-balanced between technological evolution and the further improvement and stabilization of currently utilized techniques.
Caution should be paid to the indiscreet pursuit of new technology as it can lead to inappropriate use of important resources and can endanger patients. In order for the new technologies and techniques to be successfully adopted, they should be cost-effective, and consumer safety should never be compromised. In the current study, it was ironic that MP who are both potential developers and potential customers should express more uncertainty about a newer technology; moreover, they indicated that it was too expensive. It is desirable for developers to consider who will benefit the most from a new technology before engaging in pursuit of that new technology; patients, developers, health care providers, or medical industries?
In conclusion, this study demonstrated that LS and OS are relatively readily acceptable to consumers, and RS still needs further improvements according to the customers' perceptions. These demands of present patients should be heard more attentively by developers and health care providers. Resources should be invested in further improving current LS and OS and efforts should be committed to lower the costs of equipment of laparoscopic and RS at the same time.
Figures and Tables
Fig. 1
Laparoscopic surgery is the most preferred method in benign disease cases, whereas open surgery the first choice in malignant disease cases.

Fig. 2
Main considerations in choosing the preferred method of surgery according to disease type are summarized.

Fig. 3
(A) Laparoscopic surgery is the most preferred by both medical personnel and lay persons in benign disease cases. (B) In malignant cases, open surgery is the method of choice in both groups.

Fig. 4
The difference in the most influential factor in deciding the surgical method between medical personnel and lay persons in benign (A) and malignant (B) conditions is illustrated.

ACKNOWLEDGEMENTS
This study is supported by grant from the National R&D Program for Cancer Control from the Ministry of Health & Welfare, Republic of Korea (No. 1120310). The statistical consultation was given by Dr. Joongyub Lee at the Medical Research Collaborating Center at Seoul National University Hospital.
Notes
References
1. Litynski GS. Profiles in laparoscopy: Mouret, Dubois, and Perissat: the laparoscopic breakthrough in Europe (1987-1988). JSLS. 1999; 3:163–167.
2. Kang CM, Kim DH, Lee WJ. Ten years of experience with resection of left-sided pancreatic ductal adenocarcinoma: evolution and initial experience to a laparoscopic approach. Surg Endosc. 2010; 24:1533–1541.
3. Huscher CG, Mingoli A, Sgarzini G, Sansonetti A, Di Paola M, Recher A, et al. Laparoscopic versus open subtotal gastrectomy for distal gastric cancer: five-year results of a randomized prospective trial. Ann Surg. 2005; 241:232–237.
4. Colon Cancer Laparoscopic or Open Resection Study Group. Buunen M, Veldkamp R, Hop WC, Kuhry E, Jeekel J, et al. Survival after laparoscopic surgery versus open surgery for colon cancer: long-term outcome of a randomised clinical trial. Lancet Oncol. 2009; 10:44–52.
5. Lee SE, Jang JY, Lim CS, Kang MJ, Kim SW. Systematic review on the surgical treatment for T1 gallbladder cancer. World J Gastroenterol. 2011; 17:174–180.
6. Chen HY, Juan CC, Ker CG. Laparoscopic liver surgery for patients with hepatocellular carcinoma. Ann Surg Oncol. 2008; 15:800–806.
7. Horiguchi A, Uyama I, Miyakawa S. Robot-assisted laparoscopic pancreaticoduodenectomy. J Hepatobiliary Pancreat Sci. 2011; 18:287–291.
8. Lanfranco AR, Castellanos AE, Desai JP, Meyers WC. Robotic surgery: a current perspective. Ann Surg. 2004; 239:14–21.
9. Marescaux J, Dallemagne B, Perretta S, Wattiez A, Mutter D, Coumaros D. Surgery without scars: report of transluminal cholecystectomy in a human being. Arch Surg. 2007; 142:823–826.
10. Shin CM, Lee YJ, Suh HS, Jang BH, Park J, Son HJ, et al. A health technology assessment for clinical effectiveness of robotic surgery in Korea. Seoul: National Evidence-based Healthcare Collaborating Agency;2011.
11. Cohen J. A coefficient of agreement for nominal scales. Educ Psychol Meas. 1960; 20:37–46.
12. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977; 33:159–174.
13. Armstrong BK, White E, Saracci R. Principles of exposure measurement in epidemiology. New York: Oxford University Press;1992.
14. Gagner M, Pomp A. Laparoscopic pancreatic resection: Is it worthwhile? J Gastrointest Surg. 1997; 1:20–25.
15. Melvin WS, Needleman BJ, Krause KR, Ellison EC. Robotic resection of pancreatic neuroendocrine tumor. J Laparoendosc Adv Surg Tech A. 2003; 13:33–36.
16. Giulianotti PC, Sbrana F, Bianco FM, Elli EF, Shah G, Addeo P, et al. Robot-assisted laparoscopic pancreatic surgery: single-surgeon experience. Surg Endosc. 2010; 24:1646–1657.
17. Palanivelu C, Rajan PS, Rangarajan M, Vaithiswaran V, Senthilnathan P, Parthasarathi R, et al. Evolution in techniques of laparoscopic pancreaticoduodenectomy: a decade long experience from a tertiary center. J Hepatobiliary Pancreat Surg. 2009; 16:731–740.
18. Kang CM, Kim DH, Lee WJ, Chi HS. Conventional laparoscopic and robot-assisted spleen-preserving pancreatectomy: does da Vinci have clinical advantages? Surg Endosc. 2011; 25:2004–2009.
19. Willingham FF, Gee DW, Sylla P, Kambadakone A, Singh AH, Sahani D, et al. Natural orifice versus conventional laparoscopic distal pancreatectomy in a porcine model: a randomized, controlled trial. Gastrointest Endosc. 2009; 70:740–747.
20. Barbash GI, Glied SA. New technology and health care costs: the case of robot-assisted surgery. N Engl J Med. 2010; 363:701–704.
Supplementary Material
Supplementary questionnaire section 1, 2, 3 can be found via http://thesurgery.or.kr/src/sm/astr-86-7-s001.pdf.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download