Abstract
Anatomic variations of the portal vein (PV) and bile duct (BD) are more common on the right lobe as compared with left lobe grafts in living donor liver transplantation (LDLT). We recently experienced a case of LDLT for hepatocellular carcinoma combined with liver cirrhosis secondary to hepatitis B virus and hepatitis C virus infection. The only available donor had right lobe graft with type IV PV associated with type IV BD. The patient underwent relaparotomy for PV stenting due to PV stenosis. Percutaneous transhepatic biliary drainage was done for a stricture at the site of biliary reconstruction. Thereafter, the patient was discharged in good health. Our experience suggests that, the use of right lobe graft with type IV PV accompanied by type IV BD should be the last choice for LDLT, because of its technical difficulty and risks of associated complications.
Living-donor liver transplantation (LDLT) using a right lobe graft has become popular because it provides a larger size of liver graft that is appropriate for adult recipients despite ethical issues of the safety of a healthy living donor. Most liver transplantation centers have used right lobe more than left lobe grafts for adult recipients. So, transplant surgeons are more often confronted with anatomic variations of the portal vein (PV) and bile duct (BD), which are more common on the right liver as compared with the left [1]. Here, we used a right lobe graft with type IV PV combined with a similar BD variant that was considered in the past as a relative contraindication for donation.
We recently experienced a case of a 35-year-old male who underwent primary LDLT with right lobe graft for single hepatocellular carcinoma, 2.5 cm in diameter, on top of liver cirrhosis due to hepatitis B virus and hepatitis C virus. On routine preoperative imaging study of the only available live donor, including three-dimensional reconstruction computed tomography with volumetric analysis and magnetic resonance cholangiography, he had right lobe with type IV PV (anterior sectoral branching from the umbilical portion of the left PV) associated with type IV BD (right posterior sectoral duct drains into left duct at its umbilical portion) and dual arterial inflows; the first one supplied right posterior segment and the second one supplied right anterior segment, both originated from the common hepatic artery (Fig. 1).
The graft weighed 737 g, which yielded a graft-to-recipient weight ratio of 1.02%. The cold ischemic time was 125 minutes, and the warm ischemic time was 46 minutes. The operative time was 24 hours, with transfusions of 19 units of packed red blood corpuscles, 24 units of fresh frozen plasma and 34 units of platelet concentrate. During removal of the recipient's native liver, transection of the PV was performed 1-cm proximal to the bifurcation. A Y-graft was then created by harvesting the left and right PV's 1-cm distal to the bifurcation. The Y-graft was then anastomosed to the anterior and posterior sectoral PV's on the back table. Final anastomosis was made between the stem of the Y-graft and the native PV in a way to prevent postoperative twisting or stretching (Fig. 2). Arterial reconstruction of dual hepatic arteries of the graft was performed under microscopic magnification using 9-0 polypropylene (Proline; Ethicon Endo-Surgery Inc., Somerville, NJ, USA) interrupted sutures. Biliary reconstruction with Roux-en-Y hepatico-jejunostomy without biliary stents was done for the two ducts. Also, segment V and VIII hepatic veins reconstruction was done using cryopreserved iliac vein, and anastomosing right inferior hepatic vein separately into inferior vena cava. Intraoperative Doppler ultrasound scan demonstrated good portal, arterial flow and hepatic outflow in the graft and also postoperative three-dimensional reconstruction computed tomography scan done on the fourth postoperative day revealed integrity of PV, hepatic artery and hepatic vein reconstructions.
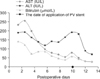
On the eighth postoperative day, there was a rise in serum aspartate aminotransferase, alanine aminotransferase and bilirubin (Fig. 3) with an increase in the amount of ascites. Three-dimensional reconstruction computed tomography scan done on the tenth postoperative day revealed anastomotic strictures in both anterior and posterior PV's. The patient underwent relaparotomy for intraoperative insertion of self-expandable metallic stents (Ev3 Inc., Plymouth, MN, USA) across each PV anastomosis through inferior mesenteric vein. Thereafter, there was a decline in aspartate aminotransferase, alanine aminotransferase, and bilirubin levels to normal levels. On the twenty-second postoperative day, there was a continuously spiking fever due to multiple small liver abscesses, confirmed by computed tomography scan that also revealed mild intrahepatic biliary radicals dilatation suggesting a stricture at the sites of biliary reconstruction. Percutaneous transhepatic biliary drainage was done on the thirtieth postoperative day. Intravenous antibiotics were given for 6 weeks. Thereafter, the patient was discharged from the hospital in good health on the eighty-fifth postoperative day after complete eradication of infection.
In LDLT, the right lobe has many anatomic variations, which can lead to surgical complications. Inaccurate knowledge of the vascular and biliary anatomy can lead to necrosis and loss of graft owing to ischemic, biliary, or parenchymal complications [2]. As our knowledge of the vascular anatomy increases and surgical techniques evolve, more marginal livers are secured from donors with previous contraindications for partial hepatic donation [3].
Lee et al. [4] reported in their study three cases in which right posterior PV comes directly from the main PV and the right anterior PV emerges from the left PV at or near the umbilical point, in all three cases double end-to-end anastomosis after plasty using recipient's PV was performed. But detailed information of those cases was not described.
Lee et al. [5] do not permit right hepatectomy from donors with type IV anomalous PV branching. They advised that donors with such venous anomaly allow for right posterior sector donation only. Also, Mount Sinai Hospital reported that no patients with such anomaly were operated on in their study of 96 right lobe LDLT [6].
Anterior PV branch arising from the left PV at or near the umbilical portion is a high risk and challenging variant. Nakamura et al. [7] described in their study two cases of type IV PV. An interposed venous graft was anastomosed with the recipient's portal trunk in an end-to-side fashion in these two cases. Also, in this report, they described a case similar to ours in which anterior PV branch arose deep in the parenchyma and was accompanied by intraparenchymal anterior BD tributary concluding that it should be considered as a contraindication for grafting because of the difficulty of reconstruction. The anterior biliary tributary in this case was left unreconstructed with external biliary drainage to avoid compression on the complex PV reconstruction.
LDLT using the right lobe can be performed safely, but there is a potential risk because of various anatomic variants. In this case report, we used right lobe graft in which anterior PV branch arising from left PV near the umbilical portion with right posterior BD drained into the left duct at its umbilical portion. Complex vascular and biliary anatomy were the major risk factors for PV and biliary complications in our case. So, we believe that the use of right lobe graft with type IV PV accompanied by type IV BD in LDLT should be the last choice for donation, because of the increased risk of PV and biliary complications.
Figures and Tables
 | Fig. 1(A) Reconstruction computed tomography scan showing portal vein anatomy of the donor. (B) Reconstruction computed tomography scan showing arterial anatomy of the donor. (C) Intraoperative cholangiogram showing biliary anatomy of the donor. RAPV, right anterior portal vein; RPPV, right posterior portal vein. LHA, left hepatic artery; RAHA, right anterior hepatic artery; RPHA, right posterior hepatic artery; RPSD, right posterior sectoral duct; RASD, right anterior sectoral duct. |
ACKNOWLEDGEMENTS
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (2011-0014581) and Korea University Research Fund (K1220311).
Notes
References
1. Marcos A, Ham JM, Fisher RA, Olzinski AT, Posner MP. Surgical management of anatomical variations of the right lobe in living donor liver transplantation. Ann Surg. 2000; 231:824–831.
2. Gadzijev EM. Surgical anatomy of hepatoduodenal ligament and hepatic hilus. J Hepatobiliary Pancreat Surg. 2002; 9:531–533.
3. Ohkubo M, Nagino M, Kamiya J, Yuasa N, Oda K, Arai T, et al. Surgical anatomy of the bile ducts at the hepatic hilum as applied to living donor liver transplantation. Ann Surg. 2004; 239:82–86.
4. Lee KK, Lee SK, Moon IS, Kim DG, Lee MD. Surgical techniques according to anatomic variations in living donor liver transplantation using the right lobe. Transplant Proc. 2008; 40:2517–2520.
5. Lee SG, Hwang S, Kim KH, Ahn CS, Park KM, Lee YJ, et al. Approach to anatomic variations of the graft portal vein in right lobe living-donor liver transplantation. Transplantation. 2003; 75:3 Suppl. S28–S32.
6. Varotti G, Gondolesi GE, Goldman J, Wayne M, Florman SS, Schwartz ME, et al. Anatomic variations in right liver living donors. J Am Coll Surg. 2004; 198:577–582.
7. Nakamura T, Tanaka K, Kiuchi T, Kasahara M, Oike F, Ueda M, et al. Anatomical variations and surgical strategies in right lobe living donor liver transplantation: lessons from 120 cases. Transplantation. 2002; 73:1896–1903.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download