Abstract
Gastric anisakiasis is a parasitic disease caused by the gastric mucosal penetration of the Anisakis larvae ingested with raw fish. Acute gastric anisakiasis is diagnosed by the endoscopic visualization of Anisakis larvae along with mucosal edema, erythema, hemorrhage, and/or an ulcer, whereas chronic anisakiasis is often observed as a localized tumor commonly occurring in the submucosal layer, and is characterized by eosinophilic granuloma with edema and embedded Anisakis larvae on pathological examination of surgical specimens. We report here a case of chronic gastric anisakiasis provoking a bleeding gastric ulcer, which is a rare clinical manifestation of this condition.
Gastric anisakiasis, which was first reported in 1960 by Van Thiel et al. [1], occurs when the nematode Anisakis marina is ingested and penetrates the gastric mucosa.
The clinical symptoms of gastric anisakiasis are classified as acute or chronic [2]. Most patients with acute symptoms have epigastric pain within 1 to 3 days, and show mucosal edema, erosion, erythema, hemorrhage, and/or ulcers on endoscopic examination. It is easily treated by endoscopic removal of the larvae [3]. However, the chronic type is usually asymptomatic or has mild nonspecific pain, and is often observed as a localized tumor commonly occurring in the submucosal layer, and is characterized by eosinophilic granuloma with edema. Thus, the chronic type of gastric anisakiasis is rarely diagnosed and with diagnosis made incidentally at endoscopy or after discovery of embedded Anisakis larvae during pathological examination of specimens obtained during surgery [3].
Moreover, in such cases, rare unusual morphologies are noted that resemble malignant tumor-like features and bleeding ulcerated submucosal tumors (SMT), but these disappear shortly after the removal of the Anisakis larvae. Thus, a relationship between anisakiasis and a vanishing tumor has been suggested [4,5].
We report here a case of chronic gastric anisakiasis provoking a bleeding gastric ulcer with the intention of its consideration in the differential diagnosis of gastric SMT.
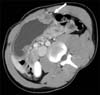
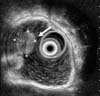
A 28-year-old man complained of sharp upper abdominal pain overnight and of passing tarry stool the following morning. The patient did not recall eating raw fish in the past several weeks. He did not complain of nausea, vomiting, diarrhea, or fever. The results of all the hematologic and chemical blood tests were normal on admission, with the exception of an elevated WBC count, CRP level, and erythrocyte sedimentation rate. Upper endoscopy showed a central ulcer on a submucosal tumor-like lesion with surrounding mucosal edema on the greater curvature of the gastric midbody (Fig. 1). Examination of biopsy specimens revealed ulceration and inflammatory cell infiltration. Abdominal CT showed a localized and inhomogeneous enhanced submucosal mass of approximately 3 cm in size on the greater curvature of the gastric midbody (Fig. 2). Moreover, endoscopic ultrasonography (EUS) showed a 3-cm- × 2.5-cm-sized heterogeneous submucosal occupied mass on the greater curvature of the gastric midbody (Fig. 3).
Although the biopsy results proved that this was not a malignant condition, surgery was considered because the tumor may have been a gastrointestinal stromal tumor and due to the size of the submucosal mass (3 cm). A laparoscopic gastric wedge resection was performed and histopathological examination showed severe inflammatory cell infiltration, edema, and abscess formation with a submucosal eosinophilic granuloma around the larvae, which are findings consistent with gastric anisakiasis (Fig. 4). The patient's postoperative course was uneventful.
The pathogenesis of gastric anisakiasis is considered to include an allergic reaction to the Anisakis antigen. Infestation of the gastric mucosa with the larva of Anisakis causes direct tissue damage following an invasion of the gut wall. Eosinophil infiltration and proliferation of connective tissue occur around the larval body, followed by the formation of an eosinophilic granuloma, which has the appearance of an SMT. Subsequently, the granuloma usually decreases in size and gradually disappears [2,3]. Rarely, patients with strong allergic reactions develop stomach perforation and bleeding [5,6].
In the present case, the patient showed a central ulcer on gastric SMT and severe inflammatory cell infiltration with submucosal eosinophilic granuloma surrounding the larvae, and it is thought that chronic gastric anisakiasis provoked a bleeding gastric ulcer by triggering a strong allergic reaction.
Although serologic tests such as anti-Anisakis-specific IgE antibody and anti-Anisakis larvae IgG antibody were not performed in the present case, we believe that it is reasonable for this case to be considered as chronic anisakiasis rather than acute anisakiasis in view of both the clinical and histopathological findings.
The present case did not have recent history of eating raw fish. Moreover, CT and EUS showed a localized gastric submucosal mass, and histopathological finding showed abscess formation with a submucosal eosinophilic granuloma surrounding the larvae, which are usually found in chronic gastric anisakiasis.
An elevated titer of anti-Anisakis IgE antibody in blood is sensitive (100%) but not very specific (50%) because of cross-reactions with proteins in other parasites (Ascaris, Toxocara, and Echinococcus), microorganisms, insects, and plants. The measurement of anti-Anisakis IgE antibody titer may require a long duration, and the titer may not even be elevated in the early phase after the onset of symptoms. Healthy individuals who eat raw fish regularly may exhibit a pseudo-positive reaction. Therefore, the diagnosis of anisakiasis is difficult to make only on the basis of the anti-Anisakis IgE antibody titer, particularly in acute cases.
Although serologic tests are not useful in acute cases, they are important for chronic cases that have unreliable diagnoses by histopathological examination. The diagnosis can be confirmed by the detection of anti-Anisakis larvae IgG antibody in blood samples; this test yields positive results from day 1 after ingestion of the larva and yields negative results between six and 12 months after ingestion [7].
Kojima [8] classified the histological findings of chronic anisakiasis into four types according to the duration of infection and the degree of larval denaturalization. The first is the phlegmon type wherein larvae are located in the submucosal layer with eosinophil, neutrophil and histiocyte infiltrations. The second is the chronic abscess type, wherein the larvae are denaturalized and an abscess is formed by eosinophils and fibrin. The third type is the abscess-granulomatous type, which develops in six months after Anisakis larvae infection, and shows progressive granuloma and fibrosis. The fourth type is the granulomatous type, in which the abscesses develop into granulomas. The present case is considered to represent the phlegmon or chronic abscess type.
Most reports on anisakiasis have indicated that the most frequent parasitic location was the greater curvature of the gastric lower, mid and upper body. The reason for the recovery of worms primarily from the greater curvature is not clear, but Shibata et al. [9] noted that the great curvature provides a good environment for the Anisakis larvae to penetrate the gastric wall, due to the large number of folds and the more active secretion of mucus in this region. In the present case, the SMT was also distributed over the greater curvature of the gastric midbody.
Cases of gastric anisakiasis with a morphology that resembles a Borrmann type II advanced gastric cancer and a bleeding ulcerated SMT have been rarely reported, and these findings disappeared within a short period after removal of the Anisakis larvae. Thus, a relationship between anisakiasis and vanishing tumor has been suggested [4,5].
There have been several reports on vanishing tumors of the stomach since Yamazaki et al. [10] first reported the case of a tumor in the gastric curvature that disappeared rapidly; these investigators provisionally termed the lesion a "vanishing tumor of the stomach" [4,5,10].
Although not all cases of vanishing tumor of the stomach observed were anisakiasis, almost all of them presented as a localized tumor that was characterized by an eosinophilic granuloma with edema, and commonly occurred in the submucosal layer.
However, there was a report of an extremely rare case of anisakiasis that resulted in a bleeding ulcerated gastric SMT, as in the present case, and we were able to confirm chronic gastric anisakiasis after obtaining a surgical pathology specimen.
Therefore, to avoid unnecessary surgery, we should consider chronic gastric anisakiasis even in cases exhibiting the morphology of an ulcerative gastric SMT, without the definitive histopathological findings of anisakiasis.
We report here a case of chronic gastric anisakiasis provoking a bleeding gastric ulcer and suggest that chronic gastric anisakiasis should be considered in the differential diagnosis of gastric SMT.
Figures and Tables
Fig. 1
Endoscopic view shows central ulcer on submucosal tumor-like lesion with surrounding mucosal edema on greater curvature of gastric midbody.

Fig. 2
Abdominal CT shows localized and inhomogeneous enhanced submucosal mass of approximately 3 cm in size on greater curvature of gastric midbody (arrow).
References
1. van Thiel P, Kuipers FC, Roskam RT. A nematode parasitic to herring, causing acute abdominal syndromes in man. Trop Geogr Med. 1960; 12:97–113.
2. Alonso-Gomez A, Moreno-Ancillo A, Lopez-Serrano MC, Suarez-de-Parga JM, Daschner A, Caballero MT, et al. Anisakis simplex only provokes allergic symptoms when the worm parasitises the gastrointestinal tract. Parasitol Res. 2004; 93:378–384.
3. Madi LR, Ali M, Legace-Wiens P, Duerksen DR. Gastrointestinal manifestations and management of anisakiasis. Can J Gastroenterol. 2013; 27:126–127.
4. Hiramatsu K, Kamiyamamoto S, Ogino H, Satomura Y, Konishi K, Miwa A, et al. A case of acute gastric anisakiasis presenting with malignant tumor-like features: a large gastric vanishing tumor accompanied by local lymph node swelling. Dig Dis Sci. 2004; 49:965–969.
5. Takeuchi K, Hanai H, Iida T, Suzuki S, Isobe S. A bleeding gastric ulcer on a vanishing tumor caused by anisakiasis. Gastrointest Endosc. 2000; 52:549–551.
6. Ito Y, Ikematsu Y, Yuzawa H, Nishiwaki Y, Kida H, Waki S, et al. Chronic gastric anisakiasis presenting as pneumoperitoneum. Asian J Surg. 2007; 30:67–71.
7. Lorenzo S, Iglesias R, Leiro J, Ubeira FM, Ansotegui I, García M, et al. Usefulness of currently available methods for the diagnosis of Anisakis simplex allergy. Allergy. 2000; 55:627–633.
8. Kojima K. Parasitic granuloma with special reference to histopathological findings of the Anisakis-like larva infection. Jpn J Parasitol. 1966; 15:30–31.
9. Shibata O, Uchida Y, Furusawa T. Acute gastric anisakiasis with special analysis of the location of the worms penetrating the gastric mucosa. In : Ishikura H, Namiki M, editors. Gastric anisakiasis in Japan. Tokyo: Springer-Verlag;1989. p. 53–57.
10. Yamazaki M, Hara K, Hasegawa T, Kanazawa M. Vanishing tumor of the stomach? Rinsho Hoshasen. 1976; 21:47–54.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download