Abstract
Purpose
The aim of this study is to evaluate long-term outcomes regarding readmission for laparoscopy-assisted distal subtotal gastrectomy (LADG) compared to conventional open distal subtotal gastrectomy (CODG) for early gastric cancer (EGC).
Methods
Between January 2003 and December 2006, 223 and 106 patients underwent LADG and CODG, respectively, for EGC by one surgeon. The clinicopathologic characteristics, postoperative outcomes, postoperative complications, overall 5-year survival, recurrence, and readmission were retrospectively compared between the two groups.
Results
Multiple readmission rate in LADG was significantly less than that in CODG (0.4% vs. 3.8%, P = 0.039), although the readmission rate, reoperation rate after discharge, and mean readmission days were not significantly different between the two groups. Readmission rates of the LADG and CODG groups were 12.6% and 14.2%, respectively. First flatus time and postoperative hospital stay was significantly shorter in the LADG group. However, there was no significant difference in the complication rates between the two groups. Overall 5-year survival rates of the LADG and CODG group were 100% and 99.1% (P = 0.038), respectively.
Gastric cancer is one of the most common digestive tract malignancies worldwide [1], and every year, 930,000 new cases are diagnosed and 700,000 deaths occur [2]. In Korea, 28,078 new gastric cancer cases were diagnosed in 2008, accounting for 15.7% of all cancer occurrences [3]. Early detection of gastric cancer has increased recently because of improved diagnostic procedures and nationwide screening in Korea [4]. Early gastric cancer (EGC) is defined as adenocarcinoma in which the depth of invasion is confined to the mucosa or submucosa, irrespective of lymph node metastasis, and has a good prognosis with surgical curative resection [5]. Many surgeons are very interested in the patient's quality of life, because most patients can be cured after surgery [6,7,8]. Many clinical studies have been carried out on long-term survival results and short-term postoperative outcome in order to clarify the advantages of laparoscopy-assisted distal subtotal gastrectomy (LADG) for EGC patients [9,10,11,12,13,14,15]. Recently, the first multicenter, prospective, randomized trial for laparoscopy-assisted distal gastrectomy to assess the short- and long-term outcomes for EGC in Korea (Korea Laparoscopic Gastrointestinal Surgery Study Group [KLASS-01] trial) has been carried out [16].
However, no report on the long-term outcome regarding readmission associated with late complications for LADG has been published to date. Those readmissions can remarkably affect a patient's quality of life [17,18]. We reviewed patients with EGC who underwent LADG or conventional open distal subtotal gastrectomy (CODG) from January 2003 to December 2006 for assessment of the features of readmission associated with late complications during median follow-up period. Furthermore, we analyzed the short-term postoperative outcomes and long-term oncologic outcomes during median follow-up period.
Between January 2003 to December 2006, 329 consecutive patients who underwent distal subtotal gastrectomy with lymph node dissection for EGC were enrolled in this study. Of the patients, 223 patients underwent LADG, while CODG was performed on 106 patients. In early periods, our indication of LAG for gastric cancer was cT1N0M0. In 2006, we extended the indication to T2N1M0. Both LADG and CODG were performed by one surgeon with the same surgical techniques. The details of our surgical technique for LADG have been described in a previous report [9]. Each procedure was determined based on the patients' opinion following sufficient explanation of both procedures. All patients gave informed written consent for their operations. This retrospective study was approved by the Institutional Review Board of Dong-A University Medical center (IRB No. 11-183). All patients underwent preoperative evaluation, including gastrofiberoscopy and computed tomography of the abdomen and pelvis. For assessment of the depth of invasion, endoscopic ultrasonography was performed in some cases. In the case of mucosal lesions suitable for endoscopic treatment, endoscopic submucosal dissection was performed. The indication for endoscopic mucosal resection at our hospital was a T1 (mucosa) lesion of <2 cm in size with no ulcer.
We prospectively collected our gastric cancer database and retrospectively reviewed the medical records. Clinicopathologic features such as age, gender, body mass index (BMI), comorbidity disease, tumor size, histologic type, tumor location, reconstruction, resection margin, T stage, lymph node dissection, and metastatic lymph node status were compared between the LADG and CODG groups. In addition, postoperative outcomes, hospital course, postoperative morbidity, postoperative mortality, and long-term clinical outcomes, including cancer recurrence, survival and readmission were compared between the two groups. Hospital admission records were reviewed to identify readmissions associated with only gastric cancer or surgery. In addition, the reasons for readmission, timing of readmission, type of treatments, rate of reoperation after discharge, number of readmissions, and hospital stay for readmission were evaluated. We divided the readmission timing into 3 periods (<1 month, 1 month to 1 year, and >1 year).
All follow-up patients were monitored postoperatively by a routine check for blood tests, tumor markers (alpha-fetoprotein, CEA, and CA 19-9), chest radiography, endoscopy, and computed tomography every six months for two years, then every year for the next three years.
Chi-square and independent t-tests were used to compare the clinicopathological factors of patients who underwent LADG and CODG using GraphPad InStat ver. 3.06 (GraphPad Software Inc., La Jolla, CA, USA). Statistical significance was assumed for P-values <0.05. Survival curves were calculated by the Kaplan-Meier method. The log-rank test was used to analyze survival differences and PASW ver. 18.0 (SPSS Inc., Chicago, IL, USA) was used for the analysis.
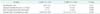
Readmission rates of the LADG and CODG groups over 5 years were 12.6% and 14.2%, respectively. The causes and timing of readmission in patients in both groups are presented in Table 1. In the LADG group, the most common cause was anastomosis edema (8 patients), and 3 patients needed reoperation due to 1 afferent loop syndrome, 1 ventral hernia, and 1 remnant stomach cancer. In the CODG group, postoperative ileus (5 patients) was the most common cause for readmission. Four patients underwent reoperation due to 1 ileus, 1 pancreatitis, 1 internal hernia, and 1 anastomotic leakage. Twelve of 28 patients (42.9%) in LADG group and 7 of 15 patients (46.7%) in CODG group were readmitted within 1 month after discharge.
Twenty eight patients in LADG group were treated by 20 conservative therapies, 15 radiologic or endoscopic interventions, and three reoperations. In CODG group, the type of treatments for 15 patients included 8 conservative therapies, 3 radiologic or endoscopic interventions, and four reoperations (Table 2).
The rate of readmission, rate of reoperation after discharge, and hospital stay for readmission were not significantly different in the two groups. However, multiple readmission rate (>2 times) in LADG was significantly less than that in CODG (0.4% vs. 3.8%, P = 0.039) (Table 3).
The clinicopathological characteristics of the patients are presented in Table 4. There were no significant differences between the two groups with respect to age, gender, comorbidity disease, histologic type, tumor location, distal margin, T stage, and N stage. BMI and tumor size was higher and larger in CODG than LADG (P = 0.010 and P < 0.001). Billroth I reconstruction was performed more in LADG group (P < 0.001). Proximal margin was statistically significant between both groups (P = 0.003). The extent of lymph node dissection and number of retrieved lymph nodes were statistically different between the two groups (P < 0.001 and P = 0.031).
Operation time was significantly longer in the LADG group than in the CODG group (219.7 ± 47.6 vs. 168.6 ± 39.8 minutes, respectively; P < 0.001). Postoperative hospitalization and first flatus times were statistically shorter in the LADG group (P < 0.001 and P < 0.001, respectively) than in the CODG group. There were 19 (17.9%) and 32 (14.3%) operation-related morbidities in the CODG and LADG groups, respectively. Duodenal stump leakage occurred in 1 case of the CODG group, which was corrected by surgical intervention. Other minor complications were treated by conservative care. There was no statistical difference between the two groups in terms of rate of complications (P = 0.376) and no mortality in either group (Table 5).
The median follow-up period for the LADG group was 93.5 months (range, 4.3-122.5 months) and for the CODG group was 97.7 months (range, 2.7-125.1 months) (P = 0.484) (Table 5). Tumor recurrence was detected in 1 case (0.5%) in the LADG group and 2 cases (1.9%) in the CODG group during the follow-up periods. In the CODG group, the first patient was a 46-year-old male who was diagnosed with submucosal cancer with lymph node metastasis (T1bN2M0, 7th edition). The tumor recurrence was detected in the brain 2.7 months after operation. He refused other management for recurrence. The second case was a 68-year-old male who was diagnosed with T1bN1M0. The recurrence was detected at the lung with multiple lymphadenopathies after 65.2 months. He underwent additional chemotherapy. In the LADG group, 1 case was a 58-year-old male who underwent Billroth-II anastomosis for T1bN1M0. The recurrence was detected at the anastomosis site after 12.0 months, although his proximal and distal resection margins in the first subtotal gastrectomy were 10.0 and 3.5 cm, respectively. He underwent completion gastrectomy, which diagnosed submucosal invasion without lymph node metastasis.
Overall 5-year survival rates of the LADG and CODG groups were 100% and 99.1% (P = 0.038), respectively, while 5-year disease free survival rates were 99.5% and 99.1% (P = 0.195), respectively (Fig. 1).
Readmissions should be considered to be indicators of medical care that reflect secondary or late complications and the breach of initial care [19]. The rate of readmission of patients has been introduced in some countries as a marker of problems in patient management and outcomes [20,21]. However, there have been few reports on readmission after gastrectomy for gastric cancer [22]. We investigated the causes of readmission, rate of readmission, reoperation rate after discharge, length of hospital stay after readmission, and number of times for readmission per one patient associated with gastric cancer or surgery between both groups over five years. Readmission due to postoperative complications definitely has an effect on patients' quality of life after gastrectomy. In the LADG group, the most common cause of readmission was anastomosis edema compared to the CODG group. We think that the anastomosis edema was associated with the size of the circular stapler (Proximate CDH 25 or 29; Ethicon Endo-Surgery Inc., Blue Ash, OH, USA). We applied a 25-mm-sized circular stapler at the Billroth-I anastomosis early on, because a 29-mm-sized circular stapler was not suitable for a small wound. On the other hand, we used a CDH 29 circular stapler during the Billroth-I anastomosis of CODG. However, only 1 of 8 anastomosis edema patients was managed by endoscopic balloon dilatation. The most common cause for readmission was postoperative ileus in the CODG group, as expected. The CODG group might be affected by a larger skin wound and more bowel manipulation during surgery than the LADG group.
In our results, 12 of 28 patients (42.9%) in LADG group and 7 of 15 patients (46.7%) in CODG group were readmitted within 1 month after discharge. These results suggested that surgeons should closely observe patients for gastrectomy of gastric cancer after discharge within at least 1 month.
Readmission rate, reoperation rate after discharge, and mean hospital stay after readmission were not significantly different between the two groups. However, multiple readmission rate (>2 times) in LADG was significantly less than that in CODG (0.4% vs. 3.8%, P = 0.039). Causes of multiple readmissions were 2 ileus, 1 pancreatitis, and 1 diarrhea in the CODG group. One patient made multiple readmissions due to gastric outlet obstruction in the LADG group.
Many reports have shown several advantages and better short-term outcomes of laparoscopic surgery when compared to open surgery, such as better cosmetic effect, improved quality of life, less intense pain, shortened hospital stay, early rehabilitation, and early return to social activity [9,10,11,12]. However, there have been relatively few reports on the long-term outcomes of laparoscopy-assisted distal gastrectomy for EGC regarding the long-term safety and feasibility [13,14,15]. Fujiwara et al. [13] reported the overall 5-year survival rate of 94 patients treated with laparoscopy-assisted surgery of EGC. Although patients with advanced gastric cancer were included, the overall 5-year survival rate was 90.0%, and recurrence occurred in 4 of 94 patients. Lee et al. [14] recently showed that there was no significant difference in survival rates between the two groups; the overall 5-year survival rates of the CODG and LADG groups were 94.9% and 95.9%, respectively. There was only 1 case of recurrence in each group.
In the present study, the overall 5-year survival rates of LADG and CODG were 100% and 99.1%, respectively; there was statistically significant difference (P = 0.038). During the median follow-up periods of both groups, recurrence occurred in 2 patients of the CODG group and 1 patient of the LADG group.
This study has several weak points. BMI, tumor size, reconstruction, proximal margin, extent of lymph node dissection, and number of retrieved lymph nodes were statistically different between the two groups. However, those differences have no clinical significance, because all patients had EGC, although the patient's selection bias might affect it. Another weak point includes the retrospective study and the potentiality that some patients were readmitted to another hospital. A multicenter nationwide cohort study is required to overcome those weak points.
In conclusion, compared to the CODG group, the LADG group has several advantages in surgical short-term outcome and some benefit in terms of readmission in surgical long-term outcome for EGC patients, even though the oncologic outcome of LADG is similar to that of CODG over 5 years. Therefore, LADG can be a feasible and preferred procedure for the treatment of EGC in terms of surgical and oncologic long-term outcome.
Figures and Tables
 | Fig. 1Comparison of 5-year survival rate (A) and disease free survival rate (B) between LADG and CODG. The 5-year survival rates were statistically different between both groups (100% vs. 99.1%, P = 0.038), respectively, while there was no statistical difference in 5-year disease free survival rates between both groups (99.5% vs. 99.1%, P = 0.195), respectively. LADG, laparoscopy-assisted distal gastrectomy; CODG, conventional open distal gastrectomy. |
ACKNOWLEDGEMENTS
This study was supported by a grant from the National R&D Program for Cancer Control, Ministry of Health & Welfare, Republic of Korea (1320270).
References
1. Smith JK, McPhee JT, Hill JS, Whalen GF, Sullivan ME, Litwin DE, et al. National outcomes after gastric resection for neoplasm. Arch Surg. 2007; 142:387–393.
2. Patel PR, Yao JC, Hess K, Schnirer I, Rashid A, Ajani JA. Effect of timing of metastasis/disease recurrence and histologic differentiation on survival of patients with advanced gastric cancer. Cancer. 2007; 110:2186–2190.
3. Jung KW, Park S, Kong HJ, Won YJ, Lee JY, Park EC, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2008. Cancer Res Treat. 2011; 43:1–11.
4. Hyung WJ, Kim SS, Choi WH, Cheong JH, Choi SH, Kim CB, et al. Changes in treatment outcomes of gastric cancer surgery over 45 years at a single institution. Yonsei Med J. 2008; 49:409–415.
5. Sano T, Hollowood A. Early gastric cancer: diagnosis and less invasive treatments. Scand J Surg. 2006; 95:249–255.
6. Sun Y, Yang Y. Study for the quality of life following total gastrectomy of gastric carcinoma. Hepatogastroenterology. 2011; 58:669–673.
7. Ikeguchi M, Kuroda H, Saito H, Tatebe S, Wakatsuki T. A new pouch reconstruction method after total gastrectomy (pouch-double tract method) improved the postoperative quality of life of patients with gastric cancer. Langenbecks Arch Surg. 2011; 396:777–781.
8. Kim YW, Baik YH, Yun YH, Nam BH, Kim DH, Choi IJ, et al. Improved quality of life outcomes after laparoscopy-assisted distal gastrectomy for early gastric cancer: results of a prospective randomized clinical trial. Ann Surg. 2008; 248:721–727.
9. Kim MC, Kim KH, Kim HH, Jung GJ. Comparison of laparoscopy-assisted by conventional open distal gastrectomy and extraperigastric lymph node dissection in early gastric cancer. J Surg Oncol. 2005; 91:90–94.
10. Lee JH, Han HS, Lee JH. A prospective randomized study comparing open vs laparoscopy-assisted distal gastrectomy in early gastric cancer: early results. Surg Endosc. 2005; 19:168–173.
11. Kitano S, Shiraishi N, Fujii K, Yasuda K, Inomata M, Adachi Y. A randomized controlled trial comparing open vs laparoscopy-assisted distal gastrectomy for the treatment of early gastric cancer: an interim report. Surgery. 2002; 131:1 Suppl. S306–S311.
12. Adachi Y, Shiraishi N, Shiromizu A, Bandoh T, Aramaki M, Kitano S. Laparoscopy-assisted Billroth I gastrectomy compared with conventional open gastrectomy. Arch Surg. 2000; 135:806–810.
13. Fujiwara M, Kodera Y, Misawa K, Kinoshita M, Kinoshita T, Miura S, et al. Longterm outcomes of early-stage gastric carcinoma patients treated with laparoscopy-assisted surgery. J Am Coll Surg. 2008; 206:138–143.
14. Lee JH, Yom CK, Han HS. Comparison of long-term outcomes of laparoscopy-assisted and open distal gastrectomy for early gastric cancer. Surg Endosc. 2009; 23:1759–1763.
15. Kitano S, Shiraishi N, Uyama I, Sugihara K, Tanigawa N. Japanese Laparoscopic Surgery Study Group. A multicenter study on oncologic outcome of laparoscopic gastrectomy for early cancer in Japan. Ann Surg. 2007; 245:68–72.
16. Kim HH, Hyung WJ, Cho GS, Kim MC, Han SU, Kim W, et al. Morbidity and mortality of laparoscopic gastrectomy versus open gastrectomy for gastric cancer: an interim report--a phase III multicenter, prospective, randomized Trial (KLASS Trial). Ann Surg. 2010; 251:417–420.
17. Epstein AM, Jha AK, Orav EJ. The relationship between hospital admission rates and rehospitalizations. N Engl J Med. 2011; 365:2287–2295.
18. Krumholz HM, Parent EM, Tu N, Vaccarino V, Wang Y, Radford MJ, et al. Readmission after hospitalization for congestive heart failure among Medicare beneficiaries. Arch Intern Med. 1997; 157:99–104.
19. Ashton CM, Wray NP. A conceptual framework for the study of early readmission as an indicator of quality of care. Soc Sci Med. 1996; 43:1533–1541.
20. Ansari MZ, Collopy BT, Booth JL. Hospital characteristics associated with unplanned readmissions. Aust Health Rev. 1995; 18:63–75.
21. Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009; 360:1418–1428.
22. Kim MC, Kim KH, Jung GJ. A 5 year analysis of readmissions after radical subtotal gastrectomy for early gastric cancer. Ann Surg Oncol. 2012; 19:2459–2464.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download