Abstract
Purpose
Chest computed tomography is performed frequently for the preoperative pulmonary staging in colorectal cancers (CRCs) regardless of the result of chest x-ray (CXR) due to its high sensitivities and specificities. The advancement of CT technology detects more indeterminate lung lesions that may require further investigations, referrals and follow-up. The aim of this study was to suggest a guideline for performing chest CT for preoperative pulmonary staging in colorectal cancer.
Methods
We performed a retrospective analysis of the records of patients who had chest CT preformed without the evidence of metastasis on CXR for preoperative pulmonary staging.
Results
Of 21 patients with metastatic nodules on chest CT, 23.8% showed pulmonary metastasis on positron emission tomography, 47.6% showed extrapulmonary metastasis on preoperative evaluation and 61.9% showed elevated serum carcinoembryonic antigen level above 10 ng/mL. These results showed significant value compared to patients without metastatic nodules. But, in analyzing patients with or without indeterminate nodules in the three contents listed above, there was no significance.
Colorectal cancer (CRC) is the second leading cause of cancer related death in Western countries and the third most common cancer in Korea [1,2]. Approximately one-fourth of CRC patients have metastasis on diagnosis. Liver is the most common site of metastasis and lung is the second most common site in CRC [3,4]. Autopsy data showed that 15% of patients with CRC have pulmonary metastasis, and that 9.4% of all pulmonary metastases at autopsy are from CRC [5].
For the assessment of the chest in the initial staging of patients with CRC, chest x-ray (CXR), abdominal CT (with pulmonary hilar extension), chest CT, PET (positron emission tomography) or combined PET/CT modalities have all been described [6]. Traditionally, pulmonary staging for CRC has been carried out by means of CXR. Chest CT is not performed routinely if a patient does not show abnormality on CXR [3]. Nowadays, chest CT is performed more frequently due to its high sensitivities of 51%-73% and specificities of up to 74%, regardless of the result of CXR [7,8,9]. And, the advancement of CT technology detects not only more numerous nodules but also smaller ones [10,11]. However, this modality has the potential to detect more indeterminate lung lesions (20%-30%) that may require further investigations, referrals and follow-up. Actually, these lesions are usually difficult to determine and seldom malignant. (10%-20%) [3,12,13] And, additional assessments, such as repeat CT, PET and percutaneous or open biopsy can increase not only patients' burden but also patients' worry of the exposure to radiation during CT scan.
The aim of this study was to suggest a guideline for performing chest CT for preoperative pulmonary staging in the patients who have no abnormal finding on CXR, which could prevent performing chest CT indiscriminately and reduce patients' burden.
One hundred twenty patients who had been undergone colorectal surgery at Ewha Womans University Mokdong Hospital due to CRC without any pulmonary nodule on CXR were included in this study. They were all diagnosed with CRC pathologically and received CXR and chest CT for preoperative pulmonary staging. Patients who had exhibited metastatic lesion on CXR regardless of the result of chest CT were excluded. Patients' medical records were reviewed and analyzed retrospectively.
On chest CT, pulmonary nodules that had been confirmed as metastasis by radiologists were referred to as 'metastatic nodule' and nodules that had been suspected as benign nodule where the possibility of metastasis had not been excluded by radiologists were referred to as 'indeterminate nodule'. Radiologists determined the 'metastatic nodule' with the characteristics of smooth margin, monogonal shape and diffuse scattered distribution.
Patients were divided into two groups by the presence of 'metastatic nodule' or 'indeterminate nodule' and analyzed in the six contents. The contents are in intervals from the time of surgery to the appearance of extrapulmonary metastasis, the positivity of pulmonary metastasis on PET, the presence of preoperative extrapulmonary metastasis, serum level of CEA, the presence of metastatic lymph node (LN) on abdominal CT, and the location of primary tumor. The interval from the time of surgery to the appearance of extrapulmonary metastasis was used for the assessment of the clinical value of the positivity of chest CT and five other contents were analyzed for the evaluation of the relationship with pulmonary metastasis.
The interval from the time of surgery to the appearance of extrapulmonary metastasis was estimated by the Kaplan-Meier method and differences between the groups in the other four contents were analyzed with chi-square test. A level of P < 0.05 was regarded as statistically significant.
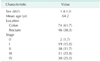
Of 120 patients enrolled in this study, 69 patients were male and 51 patients were female. Their age distribution and mean age were from 37 to 85 and 64.2 years old, respectively. The tumors originated from the colon in 74 patients (61.7%) and rectum in 46 patients (38.3%). According to the TNM classification proposed by the American Joint Committee on Cancer cancer staging manual, 7th edition [14], 2 CRCs (1.7%) were stage 0, 19 CRCs (15.8%) were stage I, 38 CRCs (31.7%) were stage II, 31 CRCs (25.8%) were stage III, and 30 CRCs (25.0%) were stage IV (Table 1).
For the assessment of clinical value of positivity on chest CT, we divided patients by the presence of metastatic nodules or indeterminate nodule on preoperative chest CT and compared the mean interval from the time of surgery to the appearance of extrapulmonary metastasis. In the patients with metastatic nodules, the mean interval was 83.7 weeks and it was 150.7 weeks in the patients without metastatic nodules (P < 0.001). After adjusting for pathologic stage, it showed significant value (P = 0.048). When indeterminate nodules were present, the mean interval was 150.9 weeks and it was 146.6 weeks when indeterminate nodules were not present (P = 0.185). Adjusting for pathologic stage, it did not show significant value (P = 0.812).
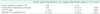
To find the factors associated with metastatic pulmonary nodules on preoperative evaluation, we divided patients into two groups by the presence of metastatic nodules and compared them in five contents of the positivity of pulmonary metastasis on PET, the presence of preoperative extrapulmonary metastasis, serum level of CEA, the presence of metastatic LNs on abdominal CT, and the location of primary tumor (Table 2). Of 21 patients with metastatic nodules on chest CT, 5 patients (23.8%) showed pulmonary metastasis on PET, but patients without metastatic nodules did not show any pulmonary metastasis on PET (P < 0.001).
Among the 21 patients with metastatic pulmonary nodules, 47.6% showed extrapulmonary metastasis on preoperative evaluation but, only 10.1% of 99 patients without metastatic pulmonary nodules, had extrapulmonary metastatic lesion (P < 0.001). In the patients with metastatic nodules on chest CT, 13 patients (61.9%) showed elevated serum CEA level above 10 ng/mL (normal range, 0-5 ng/mL). Meanwhile, there were 20 patients (21.1%) among those without metastatic nodules on chest CT, which showed significant difference (P < 0.001). Considering the presence of metastatic LN on abdominal CT, pulmonary metastatic nodule on chest CT did not show significant relationship with the presence of metastatic LN on abdomen CT (P = 0.223). Also, rectal cancer did not show significant association with metastatic nodules on chest CT (P = 0.639).
To reveal the association of indeterminate pulmonary nodules with the factors analyzed to find the relationship with metastatic pulmonary nodules, we divided patients by the presence of indeterminate pulmonary nodules on chest CT and compared them in the same manner as metastatic pulmonary nodules (Table 3). In the patients with or without indeterminate nodule, there was no patient showing pulmonary metastasis on PET. Of 20 patients with indeterminate nodule on chest CT, no patient had extrapulmonary metastasis, and 10 patients among 79 patients without indeterminate nodule (12.7%) showed extrapulmonary metastasis. This result had no statistical significance (P = 0.206). In the patients with indeterminate nodule on chest CT, 3 patients (15.8%) exhibited elevation of serum CEA level above 10 ng/mL, but compared with the patients without indeterminate nodule, there was no significant value (P = 0.529). Considering metastatic LN on abdominal CT, 14 patients (70.0%) and 55 patients (69.6%) showed the existence and absence of indeterminate nodule on chest CT, respectively, and there was no significant relationship between them (P = 0.974). Patients with rectal cancer presented indeterminate nodule in only 4 patients (20.0%) and 33 patients (41.8%) did not exhibit indeterminate nodule. This result was not significant statistically, either (P = 0.072).
Of 21 patients with metastatic pulmonary nodule, 16 patients showed aggravated metastatic lesion on follow-up chest CT after CRC surgery and 5 patients did not show any interval change of pulmonary nodule. Among the 5 patients without interval change of pulmonary nodule, two patients had surgical resection of metastatic pulmonary lesion performed, which had been proved as metastatic colon cancer, pathologically. In the patients with indeterminate pulmonary nodule, only one patient showed aggravation of metastatic lesion on follow-up study (Fig. 1).
Most guidelines concerning the staging of CRC agree that the chest should be imaged preoperatively, but there is disagreement regarding the exact type of imaging modality [6]. The 2005 Australian Government National Health and Medical Research Council Clinical Prevention, Early Detection and Management of Colorectal Cancer, the 2007 guidelines of the management of CRC issued by the Association of Coloproctology of Great Britain and Ireland, and the 2010 National Comprehensive Cancer Network Guidelines of colon and rectal cancer recommend CT scan as a routine preoperative staging modality instead of CXR [5,6,7,8,9,10,11,12,13,14,15,16,17]. While, the Scottish Guidelines Network and the American Society of Colon and Rectal Surgeons do not specify which form of imaging is most appropriate [18,19]. Regardless of this disagreement, with high sensitivities and specificities, the use of chest CT as a routine preoperative pulmonary staging is increasing [7,8,9]. But, recently, some reports suggest the disadvantage of routine preoperative pulmonary staging with CT, such as costs, radiation exposure, prolonged uncertainty because of the frequent finding of indeterminate lesions and increased patients' anxiety [6,20]. In a study by Povoski et al. [21], the authors reported a positive yield for malignancy of only 4% on CT and a positive predictive value for CT of 36% for detection of malignant lesions of the lung. In another study by Grossmann et al. [20], a prospective study of 200 patients with CRC, detected indeterminate pulmonary nodule in 50 patients. Out of 50 patients, 48 additional investigations were required. But, malignant pulmonary changes were detected only in 10 of the patients and no patient the operative plan changed or received neoadjuvant treatment. The authors concluded that routine chest CT staging should not be advocated. In our study, there were 21 patients with metastatic nodule and 20 patients with indeterminate nodule among 120 patients with CRC. To assess the clinical value of metastatic and indeterminate nodule, we analyzed the interval from the time of surgery to the appearance of extrapulmonary metastasis. Patients with metastatic nodule showed significant shorter interval than the patients without metastatic nodule. But, comparing with the patients without indeterminate nodule, patients with indeterminate nodule did not show significant results. This suggests that the indeterminate nodule can mimic pulmonary staging but does not have significant effect on the patients' clinical course.
With limited clinical value of indeterminate pulmonary nodules and increasing detection of them by the advancement of CT technology, some reports advocated that chest CT should not be performed as a routine preoperative pulmonary staging and defining high-risk patient groups and predictive factors for pulmonary metastasis is required to prevent indiscriminate chest CT and reduce patients' burden [6,20]. Traditionally, chest CTs have been performed when abnormality on CXR is present. And, several authors suggesting high-risk groups of developing pulmonary metastasis have included patients with rectal cancer and those with liver metastasis [20,22]. The perceived higher risk of developing pulmonary metastasis from patients with rectal cancer has been attributed to the direct spread into the systemic circulation via the inferior and middle rectal veins. Meanwhile, the patients with colon cancer without liver metastasis are felt to be at low risk of developing pulmonary metastasis. The venous drainage of the colon is via the portal system and the first site of spread has always been regarded as the liver. Tan et al. [23] demonstrated patients with rectal cancer were strongly associated with the presence of isolated pulmonary metastasis compared to colon cancer patients (odds ratio, 2.11; 95% confidence interval, 1.21-3.70). And, when liver metastasis is present, the subsequent spread can then occur to the lungs via systemic circulation. In our study, rectal cancer was not associated with metastatic pulmonary nodule on chest CT but the presence of extrapulmonary metastasis, such as liver, was associated with pulmonary metastasis. Additionally, the positivity of pulmonary metastasis on PET and elevated serum level of CEA above 10 ng/mL were also associated with pulmonary metastatic nodule. With these results, we can determine the high-risk group of pulmonary metastasis in patients with CRC as positivity of PET, extrapulmonary metastasis, and elevated serum CEA level above 10 ng/mL.
To conclude, in our opinion, when there is no evidence of pulmonary metastasis on CXR, it would be better to perform chest CT only in the high-risk groups determined as positivity of PET, extrapulmonary metastasis, and elevated serum CEA level above 10 ng/mL, not as routine imaging. And, it can be helpful to reduce patients' burden such as costs, radiation exposure, and prolonged uncertainty.
Figures and Tables
Fig. 1
Results of follow-up study for pulmonary nodules after surgery. a)Two patients with metastatic nodule on chest CT were performed surgical resection of metastatic pulmonary lesion; Lesions were proved as metastatic colon cancer, pathologically. CRC, colorectal cancer; CXR, chest x-ray.

References
1. Jemal A, Siegel R, Xu J, Ward E. Cancer statistics, 2010. CA Cancer J Clin. 2010; 60:277–300.
2. Jung KW, Park S, Kong HJ, Won YJ, Lee JY, Park EC, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2008. Cancer Res Treat. 2011; 43:1–11.
3. McIntosh J, Sylvester PA, Virjee J, Callaway M, Thomas MG. Pulmonary staging in colorectal cancer: is computerised tomography the answer? Ann R Coll Surg Engl. 2005; 87:331–333.
4. McCormack PM, Attiyeh FF. Resected pulmonary metastases from colorectal cancer. Dis Colon Rectum. 1979; 22:553–556.
5. Davis SD. CT evaluation for pulmonary metastases in patients with extrathoracic malignancy. Radiology. 1991; 180:1–12.
6. Parnaby CN, Bailey W, Balasingam A, Beckert L, Eglinton T, Fife J, et al. Pulmonary staging in colorectal cancer: a review. Colorectal Dis. 2012; 14:660–670.
7. Murata K, Khan A, Herman PG. Pulmonary parenchymal disease: evaluation with high-resolution CT. Radiology. 1989; 170(3 Pt 1):629–635.
8. Murata K, Takahashi M, Mori M, Kawaguchi N, Furukawa A, Ohnaka Y, et al. Pulmonary metastatic nodules: CT-pathologic correlation. Radiology. 1992; 182:331–335.
9. Luketich JD, Friedman DM, Weigel TL, Meehan MA, Keenan RJ, Townsend DW, et al. Evaluation of distant metastases in esophageal cancer: 100 consecutive positron emission tomography scans. Ann Thorac Surg. 1999; 68:1133–1136.
10. Yankelevitz DF, Henschke CI. Small solitary pulmonary nodules. Radiol Clin North Am. 2000; 38:471–478.
11. Remy-Jardin M, Remy J, Giraud F, Marquette CH. Pulmonary nodules: detection with thick-section spiral CT versus conventional CT. Radiology. 1993; 187:513–520.
12. Kronawitter U, Kemeny NE, Heelan R, Fata F, Fong Y. Evaluation of chest computed tomography in the staging of patients with potentially resectable liver metastases from colorectal carcinoma. Cancer. 1999; 86:229–235.
13. Brent A, Talbot R, Coyne J, Nash G. Should indeterminate lung lesions reported on staging CT scans influence the management of patients with colorectal cancer? Colorectal Dis. 2007; 9:816–818.
14. Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A, editors. AJCC cancer staging manual. 7th ed. New York: Springer;2010.
15. Clinical practice guidelines for the prevention, early detection and management of colorectal cancer [Internet]. Canberra (AU): Australian Government National Health and Medical Research Council;c2013. cited 2012 Feb 16. Available from: http://www.nhmrc.gov.au/guidelines/publications/cp106.
16. Guidelines for the management of colorectal cancer [Internet]. London (UK): The Association of Coloproctology of Great Britain and Ireland;c2014. cited 2012 Feb 16. Available from: http://www.acpgbi.org.uk/resources/guidelines/guidelines-for-the-management-of-colorectal-cancer/.
17. NCCN clinical practice guidelines in oncology (NCCN Guidelines): Colon/rectal cancer. ver. 1. 2010 [Internet]. Fort Wathington: National Comprehensive Cancer Network;c2012. cited 2012 Feb 16. Available from: http://www.nccn.org/professionals/physician_gls/f_guidelines.asp.
18. Scottish Intercollegiate Guidelines Network. Colorectal cancer: a national clinical guideline recommended for use in Scotland. Edinburg: Scottish Intercollegiate Guidelines Network;1997.
19. Otchy D, Hyman NH, Simmang C, Anthony T, Buie WD, Cataldo P, et al. Practice parameters for colon cancer. Dis Colon Rectum. 2004; 47:1269–1284.
20. Grossmann I, Avenarius JK, Mastboom WJ, Klaase JM. Preoperative staging with chest CT in patients with colorectal carcinoma: not as a routine procedure. Ann Surg Oncol. 2010; 17:2045–2050.
21. Povoski SP, Fong Y, Sgouros SC, Kemeny NE, Downey RJ, Blumgart LH. Role of chest CT in patients with negative chest x-rays referred for hepatic colorectal metastases. Ann Surg Oncol. 1998; 5:9–15.
22. Kirke R, Rajesh A, Verma R, Bankart MJ. Rectal cancer: incidence of pulmonary metastases on thoracic CT and correlation with T staging. J Comput Assist Tomogr. 2007; 31:569–571.
23. Tan KK, Lopes Gde L Jr, Sim R. How uncommon are isolated lung metastases in colorectal cancer? A review from database of 754 patients over 4 years. J Gastrointest Surg. 2009; 13:642–648.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download