Abstract
Purpose
The aim of this study is to investigate the clinical features and outcomes of 9 consecutive patients who suffered with leptomeningeal carcinomatosis (LMC) originating from gastric cancer.
Methods
Between January 1995 and December 2010, we retrospectively reviewed the medical records of 9 patients with gastric LMC who had been treated at St. Vincent's Hospital, The Catholic University of Korea.
Results
With the exception of 1 patient, the primary gastric cancer was Borrmann type III or IV, and 5 cases had poorly differentiated or signet ring cell histology. TNM stage of the primary gastric cancer was III in 6 patients. The median interval from diagnosis of the primary malignancy to the diagnosis of LMC was 9 months. Headache (6 cases), altered mental status (4 cases), and dysarthria (3 cases) were presenting symptoms of LMC. Computed tomography findings were abnormal in 4 of 7 cases, while magnetic resonance imaging revealed abnormality in 4 of 5 cases. Radiation therapy was administered to 5 patients and intrathecal chemotherapy was administered to only 1 patient. Median overall survival duration from the diagnosis of LMC was 3 months.
Leptomeningeal carcinomatosis (LMC), also known as carcinomatous leptomeningitis, is diffuse infiltration of malignant cells throughout the pia mater and the arachnoid membrane. Although LMC occurs in only 3-8% of all cancer patients, it is associated with devastating neurologic complications and high mortality [1]. LMC is most commonly seen in patients with leukemia, breast cancer, lymphoma, and lung cancer [2]. However, the prevalence of LMC in gastric cancer patients is as low as 0.16-0.69% [3].
Gastric cancer is the third most common cancer worldwide and is the second most common cause of death from cancer, though almost two-thirds of the cases occur in Asia [4]. The high prevalence of gastric cancer in Korea allows us the chance to study gastric cancer patients with LMC. Although there have been several published reports of LMC complicating gastric cancer, the clinical features, treatment outcomes, and prognostic factors of LMC as a metastasis from gastric carcinoma have yet to be clearly determined.
We have encountered 9 cases of LMC complicating the clinical course in patients with gastric cancer. In the present retrospective study, we reviewed our experience with LMC originating from gastric cancer to determine the clinical features and survival outcomes.
Between January 1995 and December 2010, 2,052 cases with gastric cancer were observed in St. Vincent's Hospital, The Catholic University of Korea. Among them, 9 patients who were diagnosed with LMC of gastric cancer were analyzed. Although it is not representative of the cohort of patients, the prevalence of LMC was 0.43%. Eligibility for this study included: (1) histologically confirmed gastric cancer; (2) LMC confirmed by cerebrospinal fluid (CSF) cytology and/or by magnetic resonance imaging (MRI); (3) no history of other/concurrent malignancies. We conducted a retrospective survey of the medical records of the subjects to collect data on the clinical features, laboratory and radiologic findings, treatment modalities employed and outcomes, and survival of the patients.
The clinical course from the diagnosis of gastric cancer was counted from the date of the initial endoscopy confirming gastric cancer. Overall survival was calculated from the date of diagnosis of the LMC by CSF cytology or imaging study to the date of death. The median overall survival was calculated by the Kaplan-Meier method, using StatView ver. 5.0.0 (SAS Institute Inc., Cary, NC, USA).
The clinicopathological characteristics of the patients are summarized in Table 1. Of the 9 patients, 7 (77.8%) were male, and the median age was 53 years old (range, 37 to 72 years). The majority of patients had advanced disease at initial diagnosis of gastric cancer. The 7th edition of the American Joint Committee on Cancer TNM stages of the primary gastric cancer were III in 6, IV in 1, and II in 1 patient. Among 8 patients who underwent gastric resection, lymphovascular tumor emboli were found in 7 patients and perineural invasion was detected in 2 patients. The locations of primary tumors were as follows: 2 in the cardia and the proximal body; 6 in the mid and distal body; and 1 in the whole stomach. Most of the patients had Borrmann type III or IV advanced cancer. Pathologically, 4 cases proved to be poorly differentiated adenocarcinoma. Signet-ring cell carcinoma was also observed in 1 patient.
The median interval from diagnosis of the primary gastric cancer to the diagnosis of LMC was 10 months, ranging from 0 to 76 months. One patient presented with initial LMC. The majority of patients (7 of 9 cases) initially presented with metastatic gastric cancer without LMC, and then progressed to LMC. One-third of the patients presented with curable disease at the initial diagnosis of gastric cancer (Table 2).
The presenting neurologic symptoms and signs are summarized in Table 3. The most frequent brain symptom is a headache, and an altered mental status was the most frequent brain sign. Motor deficit was the most frequently seen spinal symptom. Dysarthria or dysphonia was the most common cranial nerve symptom and both decreased visual acuity, and dizziness was the second most common.
The CSF analysis results are listed in Table 4. One patient had normal CSF profiles, including normal opening pressure before cytology results were obtained. An elevated opening pressure on lumbar puncture was noted in 7 patients. The mean CSF pressure in the patients was 305 mm CSF. 55.6% and 88.9% of patients had elevated protein and white blood cells in CSF, respectively.
All the patients with LMC had received adjuvant or palliative chemotherapy (Table 5). The median number of chemotherapy regimens and cycles that patients had received before the diagnosis of LMC was 1 (range, 1 to 4) and 6 (range, 1 to 14). At the time of the diagnosis of LMC, other metastatic disease was also observed in 7 patients, including lymph node metastasis (n = 4), bone metastasis (n = 2), peritoneal dissemination (n = 1), lung metastasis (n = 1), liver metastasis (n = 1), brain metastasis (n = 1), and skin metastasis (n = 1); the remaining 2 patients showed no evidence of metastasis other than LMC. Brain computed tomography was assessed in 7 patients and leptomeningeal enhancement was observed in 4 patients (57%). A gadolinium-enhanced MRI conducted in 5 patients where leptomeningeal enhancement was noted in 4 cases (80%). Among the 9 patients, best supportive care alone was selected for treatment in 3 patients. The therapeutic modalities applied for the remaining 6 patients were as follows: radiation treatment alone in 3 patients, systemic chemotherapy plus radiation in 2 patients, and intrathecal (IT) chemotherapy in 1 patient. For the IT administration of methotrexate, a subcutaneous reservoir was implanted. Median overall survival from diagnosis of LMC, which is shown in Fig. 1, was 3 months (range, 1 to 10 months).
LMC complicating solid tumors is not uncommon in breast cancer, lung cancer, leukemia, lymphoma, and melanoma [2]. However, LMC is a very rare complication of gastric cancer, occurring in 0.16-0.69% of gastric cancer patients [3]. In this study, the prevalence of LMC was 0.43% in all gastric cancer patients, but this figure could be underestimated because we reviewed only the cytologically confirmed cases and some of the patients with LMC may not have been evaluated appropriately.
Several routes for tumor cells to the leptomeninges have been suggested including arterial circulation, retrograde flow in Batson's venous plexus, spread via perineural spaces, perivascular spaces, or lymphatics, and direct infiltration from bone metastases [5]. In our study, seven of the nine patients had multiple metastases including retroperitoneal and supraclavicular lymph nodes, bone, peritoneum, lung, liver, and skin at the time of the diagnosis of LMC. In previous studies, the time lapse between the first recognition of cancer and establishing the diagnosis of LMC presenting with heavy neurological symptoms and signs is approximately 12 months [6]. However, in our study, the interval was much shorter, at only nine months. After the diagnosis of LMC, median survival is around 3 months (range, 1 to 10 months). Bulut et al. [7] reported that a patient's neurological symptoms regressed after intrathecal methotrexate though her symptoms were intense and she needed urgent palliation. Lee et al. [8] reported that median overall survival for patients with LMC is only 4-6 weeks if untreated and 2-4 months with therapy. Although LMC is a fatal disease, appropriate treatment may ameliorate or stabilize the symptoms of LMC. Thus, recognition of LMC is important and a high index of suspicion is needed.
The presenting symptoms and signs of LMC are commonly nonspecific and lead to multifocal neurological deficits. In a series of 54 patients with LMC from gastric cancer, headache was most prevalent (85.1%), followed by nausea/vomiting, dizziness, alterations in mental status, seizure, and motor weakness [9]. In our case, the most common symptom was headache, followed by altered mental status and dysarthria/dysphonia.
The main diagnostic procedures are cytological examination of the CSF and neuroimaging. Although CSF cytology is required for definite diagnosis of LMC, this procedure is invasive and its sensitivity is suboptimal. Wasserstrom et al. [10] reported that the sensitivity of single lumbar puncture is only 54% and 91% sensitivity could be achieved with repeated tests. In this study, one patient had an MRI scan of the brain as diagnostic imaging procedure, and this proved positive for diffuse brain LMC. We did not repeat CSF cytology examination because the patient's general condition worsened. MRI is generally regarded as superior to computed tomography (CT) for diagnosis of LMC, contrast-enhanced CT scans are often used initially as they are more cost effective and readily available. MRI best delineates the extent of LMC, including spinal cord involvement, allowing serial studies for disease follow-up [11]. Galdolinium-enhanced T1 sequences detect abnormal meningeal enhancement characteristics of LMC, and fluid-attenuated inversion recovery weighing may demonstrate increased signal of the sulci reflecting the abnormal subarachnoid space [11]. Although MRI is the main choice of imaging study for the diagnosis of LMC, meningeal gadolinium enhancement is not a specific finding and its sensitivity has been reported as between 65% and 75% [6]. Meningeal contrast enhancement may be seen with infectious and inflammatory process, but focal areas of linear enhancement, especially in a nodular pattern, in the appropriate clinical setting is highly suggestive of LMC [11]. In the current study, MRI was positive in four of five cases, and only in one patient was the MRI scan of the brain normal. Therefore, both CSF cytology and MRI should be used to diagnose LMC in patients with suspicious clinical signs.
Treatment options are very limited in LMC. Options are IT chemotherapy, radiotherapy, and best supportive care [12]. IT chemotherapy is the mainstay of treatment. Three drugs that are used include methotrexate, cytarabine, and thiotepa in combination with hydrocortisone [13-15]. Previous reports showed that patients receiving IT chemotherapy live longer than those receiving best supportive care [16,17]. However, from several randomized controlled studies, the median overall survival for LMC with either methotrexate or cytarabine was just 3-4 months [18-22]. Radiotherapy has been tried in the palliative setting for selected patients with severe neurologic dysfunction or mass lesions with a high tumor burden [8,23,24]. In our study, craniospinal irradiation was the most common treatment modality, however, additional or sequential role of radiation was not observed. Best supportive care is an option in such patients with poor performance status. Systemic chemotherapy was also administered to a limited number of patients who had better performance status. In our study, two patients who were treated with systemic chemotherapy showed the best median overall survival duration (9.5 months).
In conclusion, LMC is a rare manifestation of gastric cancer and is an extremely fatal disease. As appropriate treatment may ameliorate or stabilize the symptoms of LMC, the recognition of LMC is important and a high index of suspicion is needed.
Figures and Tables
Fig. 1
Overall survival from the diagnosis of leptomenningeal carcinomatosis. Median overall survival was 3.0 months.
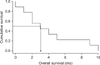
Table 5
Clinical profile of 9 patients with leptomeningeal carcinomatosis

EGCa, early gastric cancer; MDAC, moderately differentiated adenocarcinoma; PDAC, poorly differentiated adenocarcinoma; NA, not available; TG, total gastrectomy; STG, subtotal gastrectomy; 5-FU, 5-fluorouracil; CDDP, cisplatin; DOC, docetaxel; LMC, leptomeningeal carcinomatosis; LN, lymph node; LOC, loss of consciousness; UE, upper extremity; CSF, cerebrospinal fluid; CT, computed tomography; WNL, within normal limit; MRI, magnetic resonance imaging; BSC, best supportive care; IT MTX, intrathecal methotrexate.
References
1. DeAngelis LM. Current diagnosis and treatment of leptomeningeal metastasis. J Neurooncol. 1998; 38:245–252.
2. Grossman SA, Krabak MJ. Leptomeningeal carcinomatosis. Cancer Treat Rev. 1999; 25:103–119.
3. Kim M. Intracranial involvement by metastatic advanced gastric carcinoma. J Neurooncol. 1999; 43:59–62.
4. Parkin DM, Bray FI, Devesa SS. Cancer burden in the year 2000. The global picture. Eur J Cancer. 2001; 37:Suppl 8. S4–S66.
5. Kokkoris CP. Leptomeningeal carcinomatosis. How does cancer reach the piaarachnoid? Cancer. 1983; 51:154–160.
6. Tomita H, Yasui H, Boku N, Nakasu Y, Mitsuya K, Onozawa Y, et al. Leptomeningeal carcinomatosis associated with gastric cancer. Int J Clin Oncol. 2012; 17:361–366.
7. Bulut G, Erden A, Karaca B, Goker E. Leptomeningeal carcinomatosis of gastric adenocarcinoma. Turk J Gastroenterol. 2011; 22:195–198.
8. Lee JL, Kang YK, Kim TW, Chang HM, Lee GW, Ryu MH, et al. Leptomeningeal carcinomatosis in gastric cancer. J Neurooncol. 2004; 66:167–174.
9. Oh SY, Lee SJ, Lee J, Lee S, Kim SH, Kwon HC, et al. Gastric leptomeningeal carcinomatosis: multi-center retrospective analysis of 54 cases. World J Gastroenterol. 2009; 15:5086–5090.
10. Wasserstrom WR, Glass JP, Posner JB. Diagnosis and treatment of leptomeningeal metastases from solid tumors: experience with 90 patients. Cancer. 1982; 49:759–772.
11. Lisenko Y, Kumar AJ, Yao J, Ajani J, Ho L. Leptomeningeal carcinomatosis originating from gastric cancer: report of eight cases and review of the literature. Am J Clin Oncol. 2003; 26:165–170.
12. Chowdhary S, Chamberlain M. Leptomeningeal metastases: current concepts and management guidelines. J Natl Compr Canc Netw. 2005; 3:693–703.
13. Raj KP, Sanati H, Mehta RS, Zell JA. Need for a new treatment strategy: leptomeningeal carcinomatosis from gastric cancer. Anticancer Drugs. 2009; 20:301–304.
14. Chamberlain MC. Leptomeningeal metastasis. Curr Opin Oncol. 2010; 22:627–635.
15. Groves MD. New strategies in the management of leptomeningeal metastases. Arch Neurol. 2010; 67:305–312.
16. Beauchesne P. Intrathecal chemotherapy for treatment of leptomeningeal dissemination of metastatic tumours. Lancet Oncol. 2010; 11:871–879.
17. Orlando L, Curigliano G, Colleoni M, Fazio N, Nole F, Martinelli G, et al. Intrathecal chemotherapy in carcinomatous meningitis from breast cancer. Anticancer Res. 2002; 22:3057–3059.
18. Omuro AM, Lallana EC, Bilsky MH, DeAngelis LM. Ventriculoperitoneal shunt in patients with leptomeningeal metastasis. Neurology. 2005; 64:1625–1627.
19. Cole BF, Glantz MJ, Jaeckle KA, Chamberlain MC, Mackowiak JI. Quality-of-life-adjusted survival comparison of sustained-release cytosine arabinoside versus intrathecal methotrexate for treatment of solid tumor neoplastic meningitis. Cancer. 2003; 97:3053–3060.
20. Giannone L, Greco FA, Hainsworth JD. Combination intraventricular chemotherapy for meningeal neoplasia. J Clin Oncol. 1986; 4:68–73.
21. Glantz MJ, Jaeckle KA, Chamberlain MC, Phuphanich S, Recht L, Swinnen LJ, et al. A randomized controlled trial comparing intrathecal sustained-release cytarabine (DepoCyt) to intrathecal methotrexate in patients with neoplastic meningitis from solid tumors. Clin Cancer Res. 1999; 5:3394–3402.
22. Grossman SA, Finkelstein DM, Ruckdeschel JC, Trump DL, Moynihan T, Ettinger DS. Eastern Cooperative Oncology Group. Randomized prospective comparison of intraventricular methotrexate and thiotepa in patients with previously untreated neoplastic meningitis. J Clin Oncol. 1993; 11:561–569.
23. Drappatz J, Batchelor TT. Leptomeningeal neoplasms. Curr Treat Options Neurol. 2007; 9:283–293.
24. Gleissner B, Chamberlain MC. Neoplastic meningitis. Lancet Neurol. 2006; 5:443–452.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download