Abstract
Purpose
Because predicting recurrence intervals and patterns would allow for appropriate therapeutic strategies, we evaluated the clinical and pathological characteristics of early and late recurrences of colorectal cancer.
Methods
Patients who developed recurrence after undergoing curative resection for colorectal cancer stage I-III between January 2000 and May 2006 were identified. Early recurrence was defined as recurrence within 2 years after primary surgery of colorectal cancer. Analyses were performed to compare the clinicopathological characteristics and overall survival rate between the early and late recurrence groups.
Results
One hundred fifty-eight patients experienced early recurrence and 64 had late recurrence. Multivariate analysis revealed that the postoperative elevation of carbohydrate antigen 19-9 (CA 19-9), venous invasion, and N stage correlated with the recurrence interval. The liver was the most common site of early recurrence (40.5%), whereas late recurrence was more common locally (28.1%), or in the lung (32.8%). The 5-year overall survival rates for early and late recurrence were significantly different (34.7% vs. 78.8%; P < 0.001). Survival rates after the surgical resection of recurrent lesions were not different between the two groups.
Colorectal cancer (CRC) is the third most common cancer, and in 2008, it was the fourth most frequent cause of cancer-related death worldwide [1]. In Korea, the incidence of CRC increased markedly between 1999 and 2008; by an average of 6.9% per year in men and 5.2% per year in women [2].
Surgical resection is the best treatment option for patients with CRC, but tumor recurrence after resection-both local and distant-is associated with a high risk of cancer-related death. At the time of initial diagnosis, approximately two-thirds of patients with CRC undergo resection with curative intent, but 30%-50% of these patients relapse and die of their disease [3]. The majority of these recurrences occur during the first 2 years after surgery and most follow-up programs end 5 years after the primary treatment [4-6].
The principal aim of postoperative surveillance in patients with CRC is to improve survival. The recurrence of CRC is for the most part a time-limited phenomenon, with 60%-80% of recurrences becoming apparent within the first 2 years after resection and 90% within the first 4 years [7]. Survival in cases of early recurrence has remained persistently poor [8]. Both recurrent and metastatic disease, if detected early, might be amenable to a potentially curative surgical resection and this will improve the patient's chances of survival [9,10]. This provides rationale for the follow-up strategy in patients at high risk of early recurrence, allowing the rational use of adjuvant therapy and the implementation of intensive follow-up regimes for those at increased risk. However, there are still no uniformly accepted follow-up programs after curative resection for CRC and very few studies have sought to identify factors that predict the time of recurrence or the pattern of recurrence. Therefore, in this study, we aimed to identify factors that predict the recurrence interval and characterize the recurrence pattern after curative resection for CRC. An ability to predict the recurrence interval and pattern would allow appropriate therapeutic strategies to be devised, providing more tailored follow-up strategies for high-risk patients.
We retrospectively reviewed 1,216 patients with stage I-III CRC who had undergone curative resection at Kyungpook National University Hospital (Daegu, Korea) between January 2000 and May 2006. Of these, 628 had primary colon cancer and 588 had primary rectal cancer. Two surgeons performed the operations in all the patients during the study period. Tumors were staged in accordance with the seventh edition of the American Joint Committee on Cancer classification [11].
The clinical and pathological parameters included in this analysis were age, sex, preoperative levels of the tumor markers carcinoembryonic antigen (CEA) and carbohydrate antigen (CA) 19-9, primary tumor site (colon or rectum), pathology results, date of diagnosis of the recurrence, and site of recurrence. Lesions were considered colon tumors if they were located more than 15 cm from the anal verge, and rectal tumors if they were 15 cm or less from the anal verge. The adjuvant chemotherapy administered to patients with stage II or III CRC consisted of a 5-fluorouracil-based chemotherapy regimen or oral anticancer drugs (capecitabine, or fluoropyrimidine).
The standard postoperative surveillance program at our institute consists of routine follow-up at 3-month intervals for the first 2 years and at 6-month intervals thereafter, during which, a full history is obtained and a physical examination is performed. CEA and CA 19-9 levels are assayed on postoperative day 7 and at each visit after discharge. We also performed colonoscopy within 12 months following surgery and every 3 years thereafter. Chest radiography and abdominopelvic computed tomography are performed at 6 months postoperatively and then at yearly intervals. The criteria for establishing a recurrent disease included confirmation by histopathology, the presence of a palpable mass, or radiographic evidence of disease with subsequent clinical progression and supportive biochemical data, in particular increased serum CEA and CA 19-9 levels.
Recurrences were categorized as local if they were perianastomotic, and as distant if they involved the liver, lung, or other organs (e.g. para-aortic lymph nodes, peritoneum, bone, brain, or adrenal gland). Regional nodal recurrence and lateral pelvic lymph node recurrence of rectal cancer were included in the definition of local recurrence. Metachronous lesions detected during the follow-up period were not classified as tumor recurrences. The time to recurrence was determined by using the date of the follow-up visit at which tumor recurrence was discovered or by reviewing the hospital records of patients who were admitted. We defined early recurrence as that diagnosed in the first 2 years after surgery, and late recurrence as that occurring at any time thereafter.
Differences in the clinical and pathological features of early and late recurrences were analyzed using the chi-squared and Fisher exact probability test. Univariate and multivariate analyses were performed on variables influencing the recurrence interval, and for the latter, we also applied logistic regression tests. Variables with an associated P-value of less than 0.05 in univariate analysis were entered into a multivariate logistic regression model. The preoperative and postoperative status of tumor markers were related to each other, and we therefore chose the factor that had a higher odds ratio in the final multivariate model. Patient survival was analyzed using the Kaplan-Meier method, and differences between the survival curves were tested using a two-tailed log-rank test. Statistical analysis was performed using SPSS ver. 17.0 (SPSS Inc., Chicago, IL, USA); P < 0.05 was considered statistically significant.
During the follow-up period, recurrent tumors were diagnosed in 222 patients (18.3%), including 97 with colon cancer (15.4%) and 125 with rectal cancer (21.3%). Of all, 158 had an early recurrence (71.2%) and 64 had a late recurrence (28.8%). In the late recurrence group, 3 patients had recurrence more than 5 years after surgery. The mean time to postoperative recurrence was 19 months (range, 2-78 months), and the median follow-up period was 36 months (range, 4-100 months). Details of the patients' clinicopathological findings are shown in Table 1, with a focus on the distinctions between early and late recurrence. There were no differences in age, sex, primary tumor site, operative method, tumor size, type of histopathology, the degree of lymphatic or neural invasion, or pathological T-stage.
Fifty-six patients (35.4%) in the early recurrence group received adjuvant chemotherapy, compared with 18 (28.1%) in the late recurrence group. However, there was no statistically significant difference between administration chemotherapy and the time of recurrence (P = 0.295). Amongst the colon cancer cases, high postoperative CA 19-9 level and lymph node metastasis were significantly more prevalent in the early recurrence group than in the late recurrence group (P = 0.019 and P = 0.046, respectively). An analysis of rectal cancer cases showed that elevated preoperative and postoperative CA 19-9 level and lymph node metastasis were significantly more prevalent in the early recurrence group than in the late recurrence group (P = 0.008, P = 0.036, and P = 0.029, respectively). Neoadjuvant radiotherapy was not performed in our hospital during the study period, and no patient underwent radiotherapy before surgical resection. Multivariate analysis revealed that elevated postoperative CA 19-9 level, venous invasion and advanced N stage were significantly more prevalent in the early recurrence group than in the late recurrence group (Table 2).
Thirty-nine of the 222 patients (17.6%) had local recurrence alone, 173 patients (77.9%) had distant metastasis alone, and 10 patients (4.5%) had both local recurrence and distant metastasis. Except in those patients with both local and distant metastasis, the most common site of distant metastasis was the liver (n = 71, 34.2%), followed by the lung (n = 55, 25.0%), peritoneum (n = 23, 10.4%), and other organs (n = 24, 12.2%). Other sites of metastasis included the para-aortic lymph nodes (n = 13), bone (n = 2), brain (n = 3), adrenal gland (n = 1), and multiple-organs (n = 5).
The patterns of recurrence in the early and late recurrence groups are shown in Table 3. In the early recurrence group, tumors most frequently recurred in the liver. The sites at which tumors recurred differed between the early recurrence and late recurrence groups, with late recurrences developing more frequently in the lung or locally. In the late recurrence group, 3 patients had recurrence in the lung more than 5 years after curative surgery. Recurrent or metastatic lesions were more frequently resectable in the late recurrence group than in the early recurrence groups (54.7% vs. 38.0%, respectively; P = 0.023) (Table 3). A total of 48 patients (80%) in the early recurrence group and 28 patients (80%) in the late recurrence group underwent R0 resection.
Table 4 details the site of recurrence with respect to the location of primary tumor in the early and late recurrence groups. Except for patients with both local recurrence and distant metastasis, the liver was the most common site of metastasis in both groups of patients with colon cancer, but there was a higher incidence of lung recurrence in the late recurrence group. In patients with rectal cancer, the liver was the most common site of early recurrence (n = 34, 41.0%), whereas late recurrence occurred frequently both locally (n = 12, 36.4%) and in the lung (n = 13, 39.4%).
With a minimum follow-up time of 5 years for survivors, the median survival times (from operation to death) in the early and late recurrence groups were 32 and 77 months, respectively. The 5-year survival rate of patients who had early recurrence (34.7%) was worse than that for those with late recurrence (78.8%). The 5-year overall survival rate was significantly lower in the early recurrence group than in the late recurrence group (Fig. 1A) (P < 0.001). Considering overall survival after recurrence, in the late recurrence group, the 1-, 2- and 3-year overall survival rates were 84.4%, 70.3%, and 58.3%, respectively, which were significantly better than those in the early recurrence group (64.3%, 44.2%, and 37.6%, respectively; P = 0.003) (Fig. 1B). In patients who underwent repeated resections of metastatic lesions, there was no significant difference in overall survival regardless of the recurrence interval (Fig. 1C) (P = 0.791).
Recurrence after curative surgery in patients with CRC remains a major clinical problem. Reaching a consensus on the best treatment strategy has been made more difficult, however, because the definitions of early and late recurrence vary between studies. Thus, while some studies have defined early recurrence as being within the first 2 years after surgery, others have defined it as being within the first year or within the first 3 years after curative surgery [12-15]. A number of these studies analyzed risk factors associated with recurrence or the survival period after recurrence. Approximately 60%-80% of recurrences develop within the first 2 years after surgery and cases of recurrence 5 years after surgery are rare [7,16]. In concurrence with previous studies, most of the 158 patients (71.2%) showed recurrence within the first 2 years after surgery; 39 patients (17.6%), 2-3 years after surgery; and 25 patients (11.3%), more than 3 years after surgery. Only 3 patients (0.01%) showed recurrence more than 5 years after curative surgery. Therefore, we defined early recurrence as that occurring within the first 2 years after curative surgery and late recurrence as that occurring 2 years or more after curative surgery.
Identification of prognostic factors for recurrence might improve survival rates in patients with CRC after curative resection, as this would allow early detection and treatment. Previous studies have identified a number of factors including tumor stage, depth of invasion, the degree of vascular or perineural invasion, and serum levels of CEA and CA 19-9 as having statistically significant association with CRC recurrence [14,15,17]. Using these factors as predictors of the recurrence interval could further help in identifying high-risk patients and in making decisions regarding postoperative therapy. In our study, a short recurrence interval was associated with a high postoperative CA 19-9 level, venous invasion, and advanced N stage of primary tumor. Serum CEA and CA 19-9 levels are commonly used as tumor markers for patients with CRC. After curative resection, such preoperative tumor markers are important prognostic factors, and increase in their levels during the follow-up period is suggestive of a recurrence of cancer [18-20]. A previous study from our institution reported that high serum CEA and CA 19-9 levels measured preoperatively and at follow-up after curative resection were prognostic factors for CRC [21]. However, these tumor markers have not been evaluated in relation to the recurrence interval. Several previous studies found that postoperative CEA elevation has been reported to be greater for liver metastasis. Recently, CA 19-9 was suggested to be related to peritoneal recurrence [22]. In our study, both liver and peritoneal recurrence occurred prominently in the early recurrence group. The impact of CA 19-9 on early recurrence might be affected in patients with peritoneal recurrence. The presence of CA19-9 in tumors was reportedly related to tumor cell adhesion [23]. However, this information does not fully explain our results, and further studies are required to delineate the underlying mechanism and role of CA 19-9 in CRC.
In addition to serum markers, the depth of wall invasion by the primary tumor has also been reported to be an important prognostic factor. Several studies reported that adjacent organ involvement and depth of tumor invasion were significant prognostic factors for postoperative recurrence and survival rate in patients with CRC undergoing curative resection, although another retrospective study reported that the depth of invasion was not significant in predicting postoperative early recurrence in such patients [13,14,24]. Our results concurred with this latter study in that tumor depth was not significantly different between cases of early and late recurrence. We also found that adjacent organ involvement and the depth of tumor invasion were not predictive factors for early recurrence. Our results, however, show that venous invasion and lymph node metastasis are more important than tumor depth with respect to predicting the recurrence interval.
The relationship between the recurrence interval and the use of adjuvant therapy remains unclear [8,25,26]. An independent prognostic factor for early recurrence (i.e. within a 1 year of curative surgery) has been found to be the lack of adjuvant chemotherapy for patients with stage III tumors [26]. However, this was not the case in another study, even after adjusting for the initial tumor stage, and similarly, in our study, adjuvant chemotherapy was not predictive of the recurrence interval [8].
Several studies reported the different distribution of recurrent organs according to the time of recurrence [12-14]. A retrospective study of postoperative patients with colon and rectal cancer showed that the liver was the most common site of early recurrence and that local recurrence was more common in patients with rectal cancer than in those with colon cancer [14]. Cho et al. [12] reported that liver metastases occurred more frequent in patients with early recurrence, whereas lung metastases occurred more frequently in cases of late recurrence. Similarly, Aghili et al. [13] reported that the liver was the main site of early recurrence, although the late recurrence group more frequently had recurrence in the bone and peritoneum. In our study, the pattern of recurrence also differed between the early and late recurrence groups, with the liver being the most common site of early recurrence, whereas tumors that recurred late were more commonly either local or in the lung, and the latter finding was more prominent in patients with rectal cancer. Taken together, these findings indicate that patients should be monitored carefully for lung metastases during the late period of postoperative surveillance.
We found that both the 5-year overall survival rate and survival after recurrence were significantly lower in patients with an early recurrence of CRC than in those with late recurrence. In the early recurrence group, the survival of patients who underwent repeat resection did not differ significantly from the survival of those in the late recurrence group. This concurs with a previous study; in that, when patients can undergo curative resection for relapse, they receive a survival benefit regardless of the timing of relapse [27]. However, repeated resection for recurrence was feasible in only 38.0% of patients in the early recurrence group in our study, a rate that was lower than that in the late recurrence group. Thus, current clinical evaluations are not sufficient to diagnose recurrence at an early stage. Many studies have evaluated the efficacy of molecular markers or circulating tumor cells in detecting CRC recurrence [28,29]. However, to date, there have been no well-definite studies to find markers of early stage recurrence and further studies are warranted to optimize tailored follow-up surveillance regimens and to provide earlier detection of recurrence in at-risk patients.
As with most retrospective studies, a number of limitations need to be considered. Patients were enrolled from a single institution, and the data was retrospectively reviewed. Although these limitations are inevitable, this study analyzed data for patients who were followed up for at least five years after primary surgical resection. We, therefore, do not believe that these limitations detract from the importance of this study highlighting the presence of clinically different behavior between early and late recurrence. Unlike in colon cancer, neoadjuvant radiotherapy is an important therapy for the control of rectal cancer that can affect its recurrence pattern [30]. However, our study cannot analyze this point because no patient in this study underwent neoadjuvant radiotherapy prior to surgical resection. Since neoadjuvant radiotherapy is now widely used for advanced rectal cancer, further studies are required to elucidate this issue. Finally, because we have already performed intensive surveillance during the initial 2 years after surgical resection, we cannot define an adequate follow-up schedule. However, this study suggested that CA19-9 should be added for surveillance and that patients with risk factors for early recurrence should be followed up more intensively for the first 2 years than in the subsequent 3 years.
In conclusion, we found that the recurrence interval of CRC is a prognostic factor, and that a shorter interval between resection and recurrence of the primary tumor was associated with a poorer prognosis. Patients at high risk of early recurrence, such as those with an elevated postoperative CA 19-9, venous invasion of tumor, or an advanced N stage, should have more intensive follow-up. Intriguingly, in patients who underwent repeated resection of metastatic lesions, there was no significant difference in overall survival after recurrence, regardless of the recurrence interval. Therefore, close follow-up including CA19-9 is important for the earlier detection of recurrence and complete resection of recurrent disease provides a significant chance for cure in a subset of patients. Moreover, surveillance for local and pulmonary metastases is important for late follow-up surveillance.
Figures and Tables
Fig. 1
The overall survival curves for patients with colorectal cancer according to the recurrence interval. (A) Overall survival using a cutoff time of 2 years. (B). Overall survival after recurrence. (C) Overall survival after recurrence among patients undergoing repeated resection.
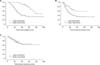
Table 1
Comparison of clinicopathological characteristics between patients with early and late tumor recurrence

Table 2
Multivariate analysis of clinicopathological factors with respect to early and late recurrence

ACKNOWLEDGEMENTS
This study was supported by a grant from the Korea Health Technology R&D Project, Ministry of Health & Welfare, Republic of Korea (A111345).
References
1. Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. GLOBOCAN 2008 v2.0, Cancer Incidence and Mortality Worldwide: IARC CancerBase No. 10 [Internet]. Lyon (FR): International Agency for Research on Cancer;c2014. cited 2013 Jan 31. Available from: http://globocan.iarc.fr.
2. Ministry of Health and Welfare. The Korea central cancer registry. Annual Report of Cancer Incidence in 2008. Seoul: Ministry for Health and Welfare;2010.
3. Abulafi AM, Williams NS. Local recurrence of colorectal cancer: the problem, mechanisms, management and adjuvant therapy. Br J Surg. 1994; 81:7–19.
4. Renehan AG, Egger M, Saunders MP, O'Dwyer ST. Impact on survival of intensive follow up after curative resection for colorectal cancer: systematic review and meta-analysis of randomised trials. BMJ. 2002; 324:813.
5. Desch CE, Benson AB 3rd, Somerfield MR, Flynn PJ, Krause C, Loprinzi CL, et al. Colorectal cancer surveillance: 2005 update of an American Society of Clinical Oncology practice guideline. J Clin Oncol. 2005; 23:8512–8519.
6. Guyot F, Faivre J, Manfredi S, Meny B, Bonithon-Kopp C, Bouvier AM. Time trends in the treatment and survival of recurrences from colorectal cancer. Ann Oncol. 2005; 16:756–761.
7. Longo WE, Johnson FE. The preoperative assessment and postoperative surveillance of patients with colon and rectal cancer. Surg Clin North Am. 2002; 82:1091–1108.
8. Kaiser AM, Kang JC, Chan LS, Beart RW. The prognostic impact of the time interval to recurrence for the mortality in recurrent colorectal cancer. Colorectal Dis. 2006; 8:696–703.
9. Figueredo A, Rumble RB, Maroun J, Earle CC, Cummings B, McLeod R, et al. Follow-up of patients with curatively resected colorectal cancer: a practice guideline. BMC Cancer. 2003; 3:26.
10. Lopez-Kostner F, Fazio VW, Vignali A, Rybicki LA, Lavery IC. Locally recurrent rectal cancer: predictors and success of salvage surgery. Dis Colon Rectum. 2001; 44:173–178.
11. Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A, editors. AJCC cancer staging manual. 7th ed. New York: Springer;2010.
12. Cho YB, Chun HK, Yun HR, Lee WS, Yun SH, Lee WY. Clinical and pathologic evaluation of patients with recurrence of colorectal cancer five or more years after curative resection. Dis Colon Rectum. 2007; 50:1204–1210.
13. Aghili M, Izadi S, Madani H, Mortazavi H. Clinical and pathological evaluation of patients with early and late recurrence of colorectal cancer. Asia Pac J Clin Oncol. 2010; 6:35–41.
14. Tsai HL, Chu KS, Huang YH, Su YC, Wu JY, Kuo CH, et al. Predictive factors of early relapse in UICC stage I-III colorectal cancer patients after curative resection. J Surg Oncol. 2009; 100:736–743.
15. Kobayashi H, Mochizuki H, Sugihara K, Morita T, Kotake K, Teramoto T, et al. Characteristics of recurrence and surveillance tools after curative resection for colorectal cancer: a multicenter study. Surgery. 2007; 141:67–75.
16. McCall JL, Black RB, Rich CA, Harvey JR, Baker RA, Watts JM, et al. The value of serum carcinoembryonic antigen in predicting recurrent disease following curative resection of colorectal cancer. Dis Colon Rectum. 1994; 37:875–881.
17. Tsai HL, Cheng KI, Lu CY, Kuo CH, Ma CJ, Wu JY, et al. Prognostic significance of depth of invasion, vascular invasion and numbers of lymph node retrievals in combination for patients with stage II colorectal cancer undergoing radical resection. J Surg Oncol. 2008; 97:383–387.
18. Yakabe T, Nakafusa Y, Sumi K, Miyoshi A, Kitajima Y, Sato S, et al. Clinical significance of CEA and CA19-9 in postoperative follow-up of colorectal cancer. Ann Surg Oncol. 2010; 17:2349–2356.
19. Holubec L Jr, Topolcan O, Pikner R, Pecen L, Holubec Sen L, Finek J, et al. Criteria for the selection of referential groups in tumor marker statistical evaluation on the basis of a retrospective study. Anticancer Res. 2003; 23(2A):865–870.
20. Morita S, Nomura T, Fukushima Y, Morimoto T, Hiraoka N, Shibata N. Does serum CA19-9 play a practical role in the management of patients with colorectal cancer? Dis Colon Rectum. 2004; 47:227–232.
21. Park IJ, Choi GS, Jun SH. Prognostic value of serum tumor antigen CA19-9 after curative resection of colorectal cancer. Anticancer Res. 2009; 29:4303–4308.
22. Yu H, Son GM, Joh YG. The clinical significance of preoperative serum levels of carbohydrate antigen 19-9 in colorectal cancer. J Korean Surg Soc. 2013; 84:231–237.
23. Dabelsteen E. Cell surface carbohydrates as prognos t ic ma rker s in human carcinomas. J Pathol. 1996; 179:358–369.
24. Fujita S, Shimoda T, Yoshimura K, Yamamoto S, Akasu T, Moriya Y. Prospective evaluation of prognostic factors in patients with colorectal cancer undergoing curative resection. J Surg Oncol. 2003; 84:127–131.
25. Bentzen SM, Balslev I, Pedersen M, Teglbjaerg PS, Hanberg-Sorensen F, Bone J, et al. Time to loco-regional recurrence after resection of Dukes' B and C colorectal cancer with or without adjuvant postoperative radiotherapy: a multivariate regression analysis. Br J Cancer. 1992; 65:102–107.
26. Jung SH, Kim HC, Kim AY, Choi PW, Park IJ, Yu CS, et al. Colorectal cancer presenting as an early recurrence within 1 year after a curative resection. J Korean Soc Coloproctol. 2008; 24:265–272.
27. Kobayashi H, Mochizuki H, Morita T, Kotake K, Teramoto T, Kameoka S, et al. Timing of relapse and outcome after curative resection for colorectal cancer: a Japanese multicenter study. Dig Surg. 2009; 26:249–255.
28. Yie SM, Lou B, Ye SR, Cao M, He X, Li P, et al. Detection of survivin-expressing circulating cancer cells (CCCs) in peripheral blood of patients with gastric and colorectal cancer reveals high risks of relapse. Ann Surg Oncol. 2008; 15:3073–3082.
29. Lee SY, Min KS, Chung JK, Jung IM, Ahn YJ, Hwang KT, et al. Carcinoembryonic antigen level of draining venous blood as a predictor of recurrence in colorectal cancer patient. J Korean Surg Soc. 2011; 81:387–393.
30. Kusters M, Marijnen CA, van de Velde CJ, Rutten HJ, Lahaye MJ, Kim JH, et al. Patterns of local recurrence in rectal cancer; a study of the Dutch TME trial. Eur J Surg Oncol. 2010; 36:470–476.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download