Abstract
Purpose
The aim of the study was to determine clinical indications for performing minimally invasive surgery (MIS) with acceptable results by reviewing our experience in congenital diaphragmatic hernia (CDH) repair and comparing outcomes of MIS with open surgery.
Methods
Medical records of patients who underwent CDH repair were reviewed retrospectively between January 2008 and December 2012, and outcomes were compared between MIS and open repair of CDH.
Results
From 2008 to 2012, 35 patients were operated on for CDH. Among these patients, 20 patients underwent open surgery, and 15 patients underwent MIS. Patients with delayed presentations (60.0% [9/15] in the MIS group vs. 20.0% [4/20] in the open surgery group; P = 0.015) and small diaphragmatic defect less than 3 cm (80.0% [12/15] in the MIS group vs. 0.0% [0/20] in the open surgery group; P < 0.001) were more frequently in the MIS group than the open surgery group. All 10 patients who also had other anomalies underwent open surgery (P = 0.002). Moreover, nine patients who needed a patch for repair underwent open surgery (P = 0.003). Patients in the MIS group showed earlier enteral feeding and shorter hospital stays. There was no recurrence in either group.
Minimally invasive surgery (MIS) has become more common in the pediatric population, and this approach has been extended to patients with congenital diaphragmatic hernia (CDH) [1]. In addition to reducing pain, surgical stress and length of hospital stay, and encouraging early recovery, MIS for CDH repair has been thought to be beneficial over conventional open surgery, especially because of reduced duration of postoperative mechanical ventilation, less need for narcotics, and lower incidence of skeletal deformities [2-5]. Many reports comparing MIS and open surgery for CDH repair have been published. However, some issues about the operative outcome and patient selection criteria of MIS for CDH repair still remain controversial. Some reports have suggested better outcomes with MIS [4-6], but others have been more cautious, especially in terms of the recurrence rate of the hernia [2,3,7-10]. To achieve a safe procedure and acceptable results in terms of recurrence, recent reports have suggested some selection or exclusion criteria for performing MIS for CDH repair [2-5,10,11]. However, no consensus exists for the selec tion criteria of MIS for CDH repair. The purpose of this study was to compare the outcomes of MIS with open surgery in patients with CDH and to identify the clinical factors that determine the selection criteria of MIS for CDH repair.
Retrospective analysis of the medical records was performed for patients with CDH who were operated on at a single children's hospital between January 2008 and Decem ber 2012. Patients who underwent repeated surgery for a recurrent hernia after the first correction in other hospitals were excluded. The clinical data of the patients were reviewed, including patient characteristics, operative approach, intra operative findings, and postoperative outcomes. Data of pa tients who underwent open surgery were compared with those of patients who underwent MIS for CDH. The patient's charac teristics included sex, gestational age, Appearance, Pulse, Grimace, Activity, Respiration (APGAR) score at 5 minutes after birth, birth weight, age at surgery, delayed presentation (detected more than 30 days after birth), location of the CDH, and combined anomalies. The data for the operative approach and intraoperative findings included the type of surgery, operative time, size of diaphragmatic defect, presence of a her nial sac, use of a patch, and open conversion rate. The pos toperative outcomes included postoperative ventilation duration, time to initiation of enteral feeding, length of hospital stay, complication, recurrence, and mortality. All MIS approaches were performed by three experienced pediatric surgeons. The Institutional Review Board of our hospital approved this study (4-2012-0918).
Data are presented as the number (percentage) or median (range). Data for the open surgery group and the MIS group were compared with univariate analysis. Continuous parameters were analyzed using a Mann-Whitney U test. Categorical parameters were evaluated using χ2 analysis or Fisher exact test. A P-value less than 0.05 was considered statistically significant. Statistical analysis was conducted with IBM SPSS ver. 18.0 (IBM Co., Armonk, NY, USA).
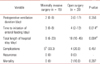
From January 2008 to December 2012, 35 patients were operated on for CDH in a single institution in Korea. Among these patients, 20 underwent open surgery, and 15 patients underwent MIS. The clinical characteristics of the patients are shown in Table 1. The median gestational age was 38.6 weeks (range, 31.7 to 41.1 weeks), and the median birth weight was 3.1 kg (range, 1.8 to 4.0 kg). The median age at surgery was 5 days (range, 1 to 300 days). The open surgery and MIS groups showed no differences in sex distribution, gestational age, birth weight, APGAR score at 5 minutes after birth, age at surgery, or location of the CDH.
However, patients who had a delayed presentation were more frequently in the MIS group than in the open surgery group (60.0% [9/15] in the MIS group vs. 20.0% [4/20] in the open surgery group; P = 0.015). All 10 patients who also had other anomalies, including pulmonary sequestration or another intra thoracic mass, imperforate anus, omphalocele, renal dupli cations, and anomalies of the extremities, underwent open surgery (P = 0.002). The median follow-up duration was 15 months without a difference between the two groups. No patients in this study required extracorporeal membrane oxygenation (ECMO) perioperatively.
Among the 15 patients in the MIS group, 12 patients (80.0%) underwent thoracoscopic repair. Two patients (13.3%) were treated using laparoscopic repair, and one patient (6.7%) was treated with robotic repair. Table 2 shows the operative findings. The size of the diaphragmatic defect was measured in 27 patients in the two groups. In the open surgery group, all patients had a large defect of more than 3 cm, whereas most patients in the MIS group (80.0% [12/15]) had a small defect of 3 cm or less (P < 0.001). Nine patients (45.0%) in the open surgery group and no patients in the MIS group underwent patch repair (P = 0.003). No differences were found in the operative time, the presence of a hernia sac, or diaphragmatic eventration between the two groups.
In the open surgery group, six patients were included who had undergone open conversion from MIS. Among these six patients, five underwent an initially attempted thoracoscopy and one a laparoscopy. The open conversion rate of MIS was 28.6% (6/21). The most common cause of open conversion was a defect that was too large to be repaired with MIS, as decided by the surgeon. In those patients (4/6) with a large diaphragmatic defect of more than 3 cm that was detected during MIS, the surgery was immediately converted to the open method. In one patient who underwent open conversion, esophageal injury during thoracoscopic surgery was the cause of the conversion to open surgery. In another patient, the initial MIS attempt was converted to open surgery because of the difficulty with MIS for combined pulmonary sequestration.
Multivariate analysis was performed to determine the selection criteria for MIS in CDH repair. From the above results, delayed presentation (a diagnosis more than 30 days after birth), combined anomalies, small diaphragmatic defect of 3 cm or less, and the need for patch repair were analyzed in the two groups. Among the four factors, only a small diaphragmatic defect was a significant factor between the MIS group and the open surgery group (P < 0.001).
Table 3 shows the postoperative outcomes of the patients. There was a significant difference in the MIS group compared to the open surgery group for initiation of enteral feeding after surgery with a median of 3 days versus 4 days, respectively (P = 0.014). The total length of the hospital stay was a median of 9 days in the MIS group compared to 18 days in the open surgery group (P = 0.004). Complications occurred in five patients during or after MIS and in four patients during or after open surgery (33.3% [5/15] in the MIS group vs. 20.0% [4/20] in the open surgery group; P = 0.451). Postoperative pneumothorax and/or pleural effusion occurred in three patients in the MIS group and in two patients in the open surgery group, respectively. One patient in the MIS group suffered postoperative subcutaneous emphysema. Esophageal injury occurred during MIS in one patient who underwent open conversion. Perforation of the small intestine and bleeding due to vena cava injury occurred in one patient during open surgery. Postoperative atelectasis of the lung on the herniated side occurred in one patient in the open surgery group. No recurrence has occurred in any patient. Two patients died after the open surgery because of a hypoplastic lung with a total diaphragmatic defect. The overall complication, recurrence, and mortality rates did not differ significantly between the two groups.
Since the first MIS repair of CDH in 1995 [12], many studies have reported comparable outcomes of MIS with open surgery to repair a CDH [4,5,10,13-17]. However, some concerns remain about the high recurrence rate of CDH after MIS repair [2,3,7-9]. The reported recurrence rate following MIS for CDH repair ranges from 0% to 39% with an overall recurrence rate of 12.3% [3-11,14,16,17]. To improve the recurrence rate or to complete successful MIS for CDH repair, a few reports have suggested selection criteria or exclusion criteria for MIS [2-5,10,11]. In one recent study, systematic quality improvement was conducted to reduce the recurrence rate following MIS for CDH [8]. In most reports, patients selected for MIS were hemodynamically stable and tolerated with the use of a ventilator without the need for ECMO. Severe pulmonary hypoplasia causing respiratory distress and pulmonary hypertension should also be considered contraindications for MIS [15,16]. A few reports of low recurrence rates have a common approach to MIS for CDH repair; they performed MIS only in patients with a small diaphragmatic defect using a primary repair and converted to open repair if a large defect was found during MIS, necessitating a patch repair [4,11,16]. In this study, all patients were stabilized preoperatively with ventilator care with or without high-frequency oscillatory ventilation or nitric oxide inhalation. ECMO was not needed in either group. Because primary repair of a large defect is difficult with MIS, we converted to the open method for a patch repair. These points could be considered selection criteria for MIS for CDH repair. For patients with preoperative stable hemodynamics, delayed presentation, or without comorbidity, MIS could be suggested as the primary treatment of choice. However, if a large diaphragmatic defect is found endoscopically during MIS and patch repair is necessary, open conversion should be considered to reduce the high recurrence rate following MIS for CDH. This idea is supported by a recent prospective, multicenter study in which the open patch repair group has a lower recurrence rate of 1.6% compared to the higher recurrence rate of 8.8% in the MIS patch repair group [7]. In addition, if a large diaphragmatic defect is observed, MIS repair should not continue. Although patch repair of a large defect is technically possible, the additional time required for patch repair using MIS can increase the risk to the patient during the course of the operation [15-17]. From these selection criteria of MIS, excluding a patient with a large diaphragmatic defect who was converted to open patch repair, no recurrence of CDH was reported in this study.
Among postoperative outcomes, time to initiation of enteral feeding and length of the hospital stay were much shorter with MIS compared with open surgery. Gourlay et al. [5] reported shorter postoperative days until full enteral feeding, leading to a shorter hospital stay and much lower hospital charges. Because of these successful results and financial benefits, more efforts are needed to select appropriate candidates for MIS.
The overall incidence rate of the postoperative complications in this study was 25.7%, which is comparable to what has been reported in the literature [2,5,8]. Although the rate of postoperative complications was not different between the groups, one patient in the MIS group suffered postoperative subcutaneous emphysema because of pneumothorax during thoracoscopy. The severity of the complications was also not different. Esophageal injury occurred in the MIS group that converted to open surgery, and bowel perforation and major vessel bleeding occurred in the open surgery group. In a recent systematic review, no evidence was found for a decreased risk of postoperative complications with MIS [2], and this study supports that finding.
One of the major limitations of this study is the retrospective nature. The size of the diaphragmatic defect was measured during the operation and noted in the medical chart. However, in eight of thirty-five patients (22.9%), no data about the size of the diaphragmatic defect were found. The second limi tation in this study is that it was not a randomized study, and selection bias between the two groups may have existed. The selection bias for patient grouping and preference of the surgeon for the surgical approach may have affected the results. In particular, patients who had combined anomalies or a large diaphragmatic defect necessitating a patch repair were included only in the open surgery group, which may have created a selection bias between the groups. Postoperative outcomes are affected by disease severity including pulmonary dysplasia, pulmonary hypertension, prematurity, or combined anomaly [18]. In this study, although no significant difference was found in the postoperative complication rate or mortality between the two groups, a larger diaphragmatic defect size in the open surgery group could induce pulmonary dysplasia or pulmonary hypertension, making the postoperative course poorer. Moreover, combined anomalies that were pre sent only in the open surgery group or the more frequent delayed presentation in the MIS group may have affected the postoperative outcome. Lastly, the follow-up duration was not long enough to evaluate differences in long-term effects between the two groups. Long-term follow-up is needed to compare late outcomes such as morbidity, recurrence rate, and functional results following both surgical approaches.
In conclusion, to achieve early enteral feeding and a short hospital stay without recurrence, MIS repair of CDH can be suggested as the treatment of choice in neonates with stable hemodynamics and without combined anomalies, or in infants with delayed presentation of CDH, if the diaphragmatic defect is small enough to be repaired primarily without the necessity of a patch repair.
References
1. Morini F, Bagolan P. Surgical techniques in congenital diaphragmatic hernia. Eur J Pediatr Surg. 2012. 22:355–363.
2. Vijfhuize S, Deden AC, Costerus SA, Sloots CE, Wijnen RM. Minimal access surgery for repair of congenital diaphragmatic hernia: is it advantageous?: an open review. Eur J Pediatr Surg. 2012. 22:364–373.
3. Szavay PO, Obermayr F, Maas C, Luenig H, Blumenstock G, Fuchs J. Perioperative outcome of patients with congenital diaphrag matic hernia undergoing open versus minimally invasive surgery. J Laparoendosc Adv Surg Tech A. 2012. 22:285–289.
4. Lao OB, Crouthamel MR, Goldin AB, Sawin RS, Waldhausen JH, Kim SS. Thoracoscopic repair of congenital diaphragmatic hernia in infancy. J Laparoendosc Adv Surg Tech A. 2010. 20:271–276.
5. Gourlay DM, Cassidy LD, Sato TT, Lal DR, Arca MJ. Beyond feasibility: a comparison of newborns undergoing thoracoscopic and open repair of congenital diaphragmatic hernias. J Pediatr Surg. 2009. 44:1702–1707.
6. Gander JW, Fisher JC, Gross ER, Reichstein AR, Cowles RA, Aspelund G, et al. Early recurrence of congenital diaphragmatic hernia is higher after thoracoscopic than open repair: a single institutional study. J Pediatr Surg. 2011. 46:1303–1308.
7. Tsao K, Lally PA, Lally KP. Congenital Diaphragmatic Hernia Study Group. Minimally invasive repair of congenital diaphragmatic hernia. J Pediatr Surg. 2011. 46:1158–1164.
8. Jancelewicz T, Langer JC, Chiang M, Bonnard A, Zamakhshary M, Chiu PP. Thoracoscopic repair of neonatal congenital diaphragmatic hernia (CDH): outcomes after a systematic quality im provement process. J Pediatr Surg. 2013. 48:321–325.
9. Lansdale N, Alam S, Losty PD, Jesudason EC. Neonatal endosurgical congenital diaphragmatic hernia repair: a syste matic review and meta-analysis. Ann Surg. 2010. 252:20–26.
10. Yang EY, Allmendinger N, Johnson SM, Chen C, Wilson JM, Fishman SJ. Neonatal thoracoscopic repair of congenital diaphragmatic hernia: selection criteria for successful outcome. J Pediatr Surg. 2005. 40:1369–1375.
11. Okazaki T, Nishimura K, Takahashi T, Shoji H, Shimizu T, Tanaka T, et al. Indications for thoracoscopic repair of congenital diaphragmatic hernia in neonates. Pediatr Surg Int. 2011. 27:35–38.
12. van der Zee DC, Bax NM. Laparoscopic repair of congenital diaphragmatic hernia in a 6-month-old child. Surg Endosc. 1995. 9:1001–1003.
13. Becmeur F, Jamali RR, Moog R, Keller L, Christmann D, Donato L, et al. Thoracoscopic treatment for delayed presentation of congenital diaphragmatic hernia in the infant: a report of three cases. Surg Endosc. 2001. 15:1163–1166.
14. Nguyen TL, Le AD. Thoracoscopic repair for congenital diaphrag matic hernia: lessons from 45 cases. J Pediatr Surg. 2006. 41:1713–1715.
15. Becmeur F, Reinberg O, Dimitriu C, Moog R, Philippe P. Thoracoscopic repair of congenital diaphragmatic hernia in children. Semin Pediatr Surg. 2007. 16:238–244.
16. Gomes Ferreira C, Reinberg O, Becmeur F, Allal H, De Lagausie P, Lardy H, et al. Neonatal minimally invasive surgery for cong enital diaphragmatic hernias: a multicenter study using thoracoscopy or laparoscopy. Surg Endosc. 2009. 23:1650–1659.
17. Arca MJ, Barnhart DC, Lelli JL Jr, Greenfeld J, Harmon CM, Hirschl RB, et al. Early experience with minimally invasive repair of congenital diaphragmatic hernias: results and lessons learned. J Pediatr Surg. 2003. 38:1563–1568.
18. Choi SY, Lee HW, Hong J. Late lung function in the repaired congenital diaphragmatic hernia. J Korean Surg Soc. 2010. 79:143–148.




 ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download