Abstract
Accessory scrotum is a rare congenital anomaly that is often associated with perineal tumor or other developmental abnormalities. Because most cases are diagnosed and treated in early childhood, little is known about the natural biologic course of this entity and associated lesions through time. We present a case of accessory scrotum associated with lipomatous hamartoma in a 46-year-old man who was born with a perineal mass. We evaluate the clinicopathologic features and discuss the pathogenesis with a review of the literature.
Accessory scrotum is the rarest developmental anomaly of scrotum [1]. Because it is usually associated with perineal lipomatous mass or anomalies in the anorectal and genitourinary system [2], early diagnosis and proper treatment are important to improve the quality of patients' lives. The majority of accessory scrotums are diagnosed in infancy. Here, we report a case of perineal accessory scrotum with a lipomatous hamartoma in a 46-year-old man. It is a good opportunity to know the natural course of both accessory scrotum and lipomatous hamartoma in an adult patient. We also discuss the pathogenesis of accessory scrotum.
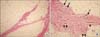
A 46-year-old male patient was admitted to Dongguk University Gyeongju Hospital because of a perineal mass. The patient was born with the mass but he didn't undergo any treatment. There was no history of rapid growth or other complications. Recently, he has felt discomfort from the mass, especially during defecation. He was a hepatitis B virus carrier and he had a 20-year history of rheumatoid arthritis. Physical examination revealed a round, pedunculated mass arising from the left lateral aspect of the anus. The mass was soft, nontender and movable, measuring 5 cm × 4 cm. There was a 3.5 cm × 1.5 cm sized elongated skin-tag-like protuberance on the left lateral portion of the main mass. The rugated skin of the protuberance was contiguous with the covering skin of the main mass. Anal sphincter was normal. There were no abnormalities in the anorectal and genitourinary system. Under the impression of a lipoma, we completely excised the mass. On section, the main mass was a lump of ill-defined yellow adipose tissue partly divided by whitish fibrous septa. The elongated small protuberance was composed of whitish soft tissue and had a rubbery texture (Fig. 1). At the junction of the two lesions, adipose tissue was intermingled with whitish soft tissue of the small nodule. Microscopically, the main mass consisted of predominant mature adipose tissue that was neither encapsulated nor well circumscribed from surrounding tissue (Fig. 2A). Small bundles of bland smooth muscle fibers, mature neural tissue and blood vessels were scattered within the adipose tissue mass (Fig. 2B). Atypical cells or malignant cells were absent. The main mass was diagnosed as a hamartoma with predominant adipose tissue (lipomatous hamartoma). The skin-tag-like protuberance was composed of numerous, irregularly oriented smooth muscle bundles, resembling the tunica dartos (Fig. 3). It was confirmed as an accessory scrotum. The perineal mass was diagnosed as perineal accessory scrotum with a lipomatous hamartoma. There was neither postoperative complications nor functional sequelae.
There are four representative developmental anomalies of the scrotum; penoscrotal transposition, bifid scrotum, ectopic scrotum, and accessory scrotum. Among them, accessory scrotum is extremely rare [1]. More than 40 cases have been reported in the English-language literature [2-6]. Accessory scrotum is a kind of ectopic scrotal tissue but never containing a testicle within it. Most of them are diagnosed in early childhood, especially in boys, and always arise in the perineum posterior to a normally developed original scrotum. Accessory scrotum may occur as an isolated anomaly but some could be associated with perineal lipoma/hamartoma or anomalies in the anorectal and genitourinary system. In a review of 23 cases of accessory scrotum, 19 cases (83%) were accompanied with perineal lipomatous mass [2]. Six out of 19 cases (32%) had anomalies such as anorectal malformations or penoscrotal transposition. Even though there was no perineal mass, accessory scrotum was associated with genitourinary and anorectal anomalies including VACTERL (vertebral, anal, cardiac, tracheoesophageal, renal and limb anomalies) association. Although accessory scrotum itself is a benign lesion, thorough physical examination and imaging studies to detect coexistent other anomalies is necessary. Prenatal early diagnosis can be made by an ultrasound examination, if we are aware of these rare congenital anomalies [3].
When accessory scrotum is accompanied with a perineal lipomatous mass, the two lesions are very contiguous. Accessory scrotum is usually attached to a lipomatous mass as a pedunculated skin tag or an incompletely separated protruding second nodule [4]. Occasionally, rugated scrotal skin simply covers a portion of the lipomatous mass. Close anatomic relationship as well as frequent coexistence of two lesions suggest the possibility that the lipomatous mass is involved in the pathogenesis of accessory scrotum. We support the hypothesis of Sule et al. [2] emphasizing the role of mesenchymal tissue within the perineal mass in the formation of accessory scrotum. Embryologically, scrotal tissue is derived from the labioscrotal swellings that are lateral to the genital tubercle. After 12 weeks of gestation, both labioscrotal swellings migrate inferomedially and fuse to form the scrotum. In our opinion, aberrantly developed fat tissue in the perineum may disrupt only minor cellular population in the inferior portion of a labioscrotal swelling. This trivial event does not affect normal development of original scrotum. But, continuous growth of intervening fat tissue forms a tumor-like mass and pushes the disrupted precursor scrotal cells. It results in an accessory scrotum over the lipomatous mass. However, we are not sure how some accessory scrotum is developed without perineal mass. In these cases, the pathogenesis may be more complex and multifactorial.
Perineal lipomatous masses are interesting in pathologic aspect as well as clinical presentation. They have been diagnosed as lipoma [2,3,5,6] or hamartoma [4,7]. Many authors named this lesion lipoma but detailed microscopic features and biologic nature were seldom described in the previous reports. In the present case, the lipomatous mass had no true capsule usually seen in typical lipoma. We noted some scattered mature neural tissue and smooth muscle bundles within the lipomatous mass. Histopathologic examination confirmed the perineal mass to be a lipomatous hamartoma.
Hamartoma is a benign tumor-like malformation and is composed of abnormally proliferated mature cells and tissue that normally present in the affected regions [8]. Hamartoma is usually asymptomatic but enlarged hamartoma can lead to complications such as mechanical obstruction, pressure effect, hemorrhage and fracture. Especially, clinicians and pathologists should take more interest when it is encountered in adult patients, because malignant transformation of hamartoma has been reported, albeit rarely [9]. In the present case, the hamartoma didn't cause any complications except discomfort.
Here, we present a 46-year-old man who was born with a perineal mass that consisted of accessory scrotum and lipomatous hamartoma. This case will be helpful for evaluation of perineal mass and the possibility of accessory scrotum should be kept in mind. The clinicopathologic features of accessory scrotum and lipomatous hamartoma in our adult patient were similar to those of children's cases.
Figures and Tables
Fig. 1
Macroscopic findings of a perineal mass. (A) Photograph reveals an elongated skin-tag-like protuberance (asterisks) over the round mass (arrows indicate base of main mass). (B) On section, the round mass is composed of yellow adipose tissue. The elongated protuberance has a rubbery texture.

References
1. Budhiraja S, Pandit SK. Accessory scrotum. Urol Int. 1999; 63:210–211.
2. Sule JD, Skoog SJ, Tank ES. Perineal lipoma and the accessory labioscrotal fold: an etiological relationship. J Urol. 1994; 151:475–477.
3. Wax JR, Pinette MG, Mallory B, Carpenter M, Winn S, Cartin A. Prenatal sonographic diagnosis of a perineal lipoma. J Ultrasound Med. 2010; 29:1257–1259.
4. Amann G, Berger A, Rokitansky A. Accessory scrotum or perineal collision-hamartoma: a case report to illustrate a misnomer. Pathol Res Pract. 1996; 192:1039–1043.
5. Göktas S, Aydur E, Yildirim I, Sumer F. Accessory scrotum attached to a perineal lipoma in an adult male. Int J Urol. 2003; 10:501–503.
6. Harada M, Udagawa A, Yoshimoto S, Ichinose M. A case of accessory scrotum with perineal lipoma. J Plast Reconstr Aesthet Surg. 2009; 62:e108–e109.
7. Ramzisham AR, Thambidorai CR. Perineal hamartoma with accessory scrotum, anorectal anomaly, and hypospadias-a rare association with embryological significance: case report. Pediatr Surg Int. 2005; 21:478–481.
8. Rosai J, Ackerman LV. Rosai and Ackerman's surgical pathology. 10th ed. New York: Mosby;2011. p. 385–386.
9. Song JS, Lee YJ, Kim KW, Huh J, Jang SJ, Yu E. Cholangiocarcinoma arising in von Meyenburg complexes: report of four cases. Pathol Int. 2008; 58:503–512.




 ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download