Abstract
Purpose
The present study is to investigate the clinical utility of tumor marker cutoff ratio (TMR) and develop a TMR combination scoring system based on preoperative tumor marker (TM) levels to prognosis prediction in gastric cancer.
Methods
We include 1,142 patients for whom two or more TMs were measured and who underwent radical gastrectomy between 1990 and 2003.
Results
Five-year risk of recurrence (5 YRR) for carcinoembryonic antigen (CEA) TMRs were 18.3%, 29.8%, 61.4% for TMR < 1.0, 1.0 ≤ TMR < 2.0, TMR ≥ 2.0 respectively. 5 YRR for carbohydrate antigen 19-9 (CA 19-9) TMR were 19.7%, 35.6%, 58.4% for TMR < 1.0, 1.0 ≤ TMR < 3.0, TMR ≥ 3.0, respectively. 5 YRR for carbohydrate antigen 72-4 (CA 72-4) TMR were 15.2% and 33.6% for TMR < 1.0 and TMR ≥ 1.0, respectively. We defined high TMR (TMR ≥ 2.0 for CEA, TMR ≥ 3.0 for CA19-9), low TMR (1.0 ≤ TMR < 2 for CEA, 1.0 ≤ TMR < 3.0 for CA 19-9 and 1.0 ≤ TMR for CA72-4) and negative TMR (TMR < 1.0 for all TMs). A TMR combination scoring system was devised with negative scored as zero points, low as 1 and high as 2 for each TMR. TMR scores were divided into four categories (score 0, 1, 2, 3 and above) based on the calculated TMR score and 5 YRR were found to be 12.8%, 23.9%, 45.5%, and 68.3%, respectively (P < 0.05). Multivariate analysis showed that our scoring system was a significant independent prognostic factor.
Gastric cancer is the fourth most common cancer and second most frequent cause of cancer-related death worldwide, with an estimated 650,000 deaths and 880,000 new cases each year [1]. Gastric cancer is particularly prevalent in Korea, being the second major cause of cancer-related deaths after lung cancer [2,3].
The TNM classification proposed by the International Union Against Cancer (UICC), consists of tumor depth (T), nodal status (N), and metastasis (M) is the most powerful and reliable factor in predicting cancer prognosis [4].
Other factors, such as tumor marker (TM), have been used as prognostic indicators as well as for postsurgical surveillance in gastric cancer [5-7]. The most commonly used TMs in clinical management of gastric cancer include carcinoembryonic antigen (CEA), carbohydrate antigen 19-9 (CA 19-9), and CA 72-4 [5,7-9]. However, there has been controversy over the use of these TMs as independent prognostic factors due to their low sensitivity and high false-positive rate [8,10]. Furthermore, there are limitations in applying these markers to clinical use.
Although they have limitations as independent prognostic factors, many studies have reported that high levels of specific TM that are above several times the upper cutoff value predict poor prognosis. The combinations of TMs can increase their prognostic sensitivity [8,11,12].
The purpose of our study is to investigate the clinical utility of tumor marker cutoff ratio (TMR) and develop a TMR combination scoring system based on preoperative TM levels that can be easily and clinically applied to prognosis prediction in gastric cancer.
We included 1,142 subjects who underwent testing for two or more TMs and who underwent radical gastrectomy from 1990 to 2003 at Chonbuk National University Hospital. We excluded 1,125 due to insufficient medical records (n = 279), R1 or 2 resection (n = 306), or insufficient TMs examined prior to gastrectomy (n = 540) (Fig. 1).
To be included, TMs must have been examined within two weeks prior to operation. We defined cutoff levels to be 5 ng/mL for CEA, 36 U/mL for CA 19-9, and 4 U/mL for CA 72-4. Also, we defined TMR as the ratio of multiples for upper normal limit of each TM. The study was approved by the Institutional Review Board of Chonbuk National University Hospital. We defined R0 resection as no gross or microscopic tumor remaining in the primary tumor bed with a pathologically confirmed margin-negative resection along with a lymph node dissection to at least level D2 and no distant metastasis (such as to the peritoneum or liver).
Risk of recurrence of all patients was analyzed according to the TMR of CEA, CA 19-9, and CA 72-4. TMR was stratified into five groups based on the TMR (TMR < 1.0, 1.0 ≤ TMR < 2.0, 2.0 ≤ TMR < 3.0, 3.0 ≤ TMR < 5.0, TMR ≥ 5.0). Significant TMR levels for each TM were confirmed.
We detected the recurrence of gastric cancer through a programmed follow-up schedule of physical examination, TM measurement, simple chest radiography, abdomen ultrasonography, abdominal computed tomography, gastrointestinal endoscopy, and, if necessary, liver magnetic resonance image every 6 months postoperatively.
The last follow-up date for the study sample was December 31, 2008. Median follow-up duration was 57 months (95% confidence interval [CI], 53.2 to 57.1; range, 1 to 175 months). The median follow-up duration of survivors was 69 months (95% CI, 68.7 to 73.2; range, 1 to 175 months).
The Kaplan-Meier method was used to calculate risk of recurrence for gastric cancer, and statistical comparisons of different factors were made based on the log-rank test. In multivariate analysis, regression analysis was performed using the Cox proportional hazards model. All statistical analyses were performed using the SPSS ver. 15.0 (SPSS Inc., Chicago, IL, USA). A P-value of less than 0.05 was considered to be significant.
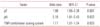
O f the 1,142 included subjects, the mean age was 57.1 years (range, 22 to 85 years) with 800 males (70%) and 342 females (30%). There were 613 patients with stage I (53.7%), 178 patients with stage II (15.6%), 204 patients with stage III (17.9%), and 147 patients with stage IV (12.8%) gastric carcinoma based on the 6th UICC TNM classification for malignant gastric tumors (Table 1) [4].
Positivity of CEA, CA 19-9, CA 72-4 was 12.7%, 9.0%, and 12.4%, respectively. There was a tendency toward increasing TM levels with advancing cancer stage with CEA being positive in 6.1% of stage I, 16,7% in stage II, 19.9% in stage III, and 24.7% in stage IV cancers (P < 0.001). For CA 19-9, a similar increasing pattern was found with 4.0% positive in stage I, 6.8% in stage II, 13.9% in stage III, and 24.1% in stage IV cancers (P < 0.001). CA 72-4 exceeded our defined threshold in 7.4% of stage I, 16.7% of stage II, 13.1% of stage III, and 33.3% of stage IV cancers, but there were no significant differences between the stages (P = 0.085) (Fig. 2).
Risk of recurrence by TMR of CEA, CA 19-9 and CA 72-4 are illustrated in Fig. 2. In the case of CEA, there was significant difference in 5-year risk of recurrence (5YRR) between the TMR < 1.0 group (n = 982) and 1.0 ≤ TMR < 2.0 group (n = 73) (18.3% vs. 29.8%, P < 0.05). There was no significant difference in 5YRR between groups with TMR above 2.0 with survival rates of 55.7% in 2.0 ≤ TMR < 3.0 (n = 17), 63% in 3.0 ≤ TMR < 5.0 (n = 19), and 63.9% in TMR ≥ 5.0 (n = 35) groups.
Based on these data, TMR groups in CEA could be divided into three categories TMR < 1.0, 1.0 ≤ TMR < 2.0, and TMR ≥ 2.0. Each category was classified as negative, low TMR, and high TMR. There were significant differences in 5YRR between these categories (18.3%, 29.8%, 61.4%, P < 0.001) (Fig. 3A).
TMR groups were also compared across CA 19-9, and there was no statistical difference in recurrence between the 1.0 ≤ TMR < 2.0 and 2.0 ≤ TMR < 3.0 groups nor between the 3.0 ≤ TMR < 5.0 and TMR ≥ 5.0 groups. We then defined three categories for CA 19-9 as TMR < 1.0, 1.0 ≤ TMR < 3.0, and TMR ≥ 3.0. Each category was classified as negative, low TMR, and high TMR. There were significant differences in 5YRR between these categories as well (19.7%, 35.6%, 58.4%, P < 0.001) (Fig. 3B).
For CA 72-4, there were no significant differences between groups with TMR greater than 1.0. Therefore, TMR groups were divided into 2 categories TMR < 1.0 and TMR ≥ 1.0 and classified as negative and low TMR. Comparison of 5YRR in the two categories showed a significant difference (15.2% and 33.6%, P < 0.001) (Fig. 3C).
CEA and CA 19-9 were divided into negative, low TMR, and high TMR groups. CA 72-4 was divided into negative and low TMR groups. We devised a combination scoring system in which negative TMR received a score of 0, low TMR a score of 1, and high a score of 2 points. An overall score was calculated from the sum of the scores for each subject.
The TMR combination scoring system (the sum of the scores) was divided into four categories (score 0, n=856; score 1, n=164; score 2, n=87; and score 3 and above, n=35). 5YRR for each category were 12.8%, 23.9%, 45.5%, and 68.3%, respectively (P < 0.05) (Fig. 4).
TMR combination scoring was compared with independent factors pT and pN staging on multivariate analysis. The odds ratio on for TMR combination scoring was 1.17 (95% CI, 1.01 to 1.34), showing TMR combination scoring to be an independent prognostic factor (Table 2).
The purpose of our study is to investigate the clinical utility of TMR and develop a TMR combination scoring system based on preoperative TM levels that can be easily and clinically applied to prognosis prediction in gastric cancer. TMs have been used to predict disease extent and for postsurgical surveillance of recurrence in gastric cancer. CEA, CA 19-9, and CA 72-4 are the most commonly used TMs in gastric cancer [6].
CEA, especially in colon cancer, is the most commonly used TM in tumors arising from the gastro-intestinal tract [5]. CEA, a glycoprotein extracted from colon cancer cells detected by Gold and Freedman in 1965 [13], is as a homophilic and heterophilic cell adhesion molecule on the surface of tumor cells and CEA is thought to protect cancer cells from undergoing apoptosis and promoting signal transduction [14-17].
CA 19-9 is a sialylated form of the Lewis A blood group antigen [18] obtained from colon cancer stem cells by Koprowski et al. [19] in 1979. CA 19-9 plays an important role in cell adhesion during tumor metastasis [5,20]. CA 19-9 was first used to detect cancers of the gastro-intestinal tract, but was found to be elevated in pancreatic cancer, bile duct cancer and gall bladder cancer as well [21].
CA 72-4 is a high molecular weight mucin-type glycoprotein, a human tumor-associated glycoprotein, detected by monoclonal antibody CC49 and B72.3 [9,22]. Despite the origins and roles of these TMs, there exists a controversy over their use as independent prognostic factors in human cancers, mainly due to their low sensitivity [10,23].
In our study, CEA, CA 19-9, and CA 72-4 levels exceeded the cutoff level in 12.7%, 9.0%, and 12.4% of subjects, respectively. These levels were lower than other previous studies [5,6]. These lower positive rates were probably due to the large proportion of early gastric cancer patients in this study that only includes the analysis of R0 resections.
Despite the low sensitivity, high serum levels of TMs suggest the possibility of microscopic metastasis [5]. When high levels of preoperative TMs are detected, tumor cells could have spread microscopically, even in the case of radical resection. This may lead to poorer prognosis than other patients with equivalent stages [5,10,24,25].
Takahashi et al. [12] reported that cancer recurrence is more frequent in patients with high preoperative CEA and CA 19-9 levels, especially when the ratios are higher than twofold the upper normal limit. Kim et al. [24] also reported that patients with CEA levels 2 times higher than normal limits show poorer prognosis. While a study done by Park et al. [26] demonstrated higher recurrence rates with positive CEA levels.
A study by Kochi et al. [25] showed poorer prognosis when both CEA and CA 19-9 were positive, compared to when they were both negative.
We analyzed prognosis by TMR in the current study and found poorer prognosis in patients with levels of CEA greater than twice the normal limit, levels of CA 19-9 greater than three times the normal limit, or when there is an increase in multiple TMs.
To improve the sensitivity of TMs in predicting cancer prognosis, studies have analyzed combinations of two or more TMs. Choi et al. [8] reported that the combinations of two or more TMs increased sensitivity to 68% in predicting recurrence of gastric carcinoma and proposed that TM combinations aided in predicting recurrence. Lai et al. [10] reported that preoperative TM combinations increased sensitivity to 49.1% in predicting recurrence. Marrelli et al. [27] reported 87% sensitivity when preoperative TMs were combined and found that TM combinations were positive in nearly 100% of subjects when cancer recurred in patients with positive TMs.
Accordingly, TM combinations are needed to increase overall sensitivity in predicting gastric carcinoma recurrence and to compensate for the limitations of using three TMs independently [5,8,27,28].
Despite mitigating the disadvantages of using TM independently, the clinical application of TM levels in predicting prognosis is difficult. Therefore, just as the Child-Turcotte-Pugh score is used to assess the severity of patients with liver cirrhosis, we propose a TMR combination scoring system to predict prognosis in gastric cancer that could be practically applied in clinical practice. The results of our study demonstrate poorer prognosis when TMR score is 2 points or higher. Consequently, this suggests the need for shorter-term follow-up in cases with high TMR scores to detect recurrence.
Although the TMR combination scoring system is a less powerful prognostic factor than TNM stage, this is a meaningful result that can be obtained from TMs with low sensitivity. If more powerful TMs are added to the list, the proposed scoring system could achieve more satisfactory results.
In conclusion, preoperative TMRs such as CEA, CA 19-9, and CA 72-4 show a correlation with prognosis. The TMR combination scoring system could be a useful tool for the prediction of prognosis in gastric cancer.
Figures and Tables
 | Fig. 1Diagram of patient selection. CEA, carcinoembryonic antigen; CA 19-9, carbohydrate antigen 19-9; CA 72-4, carbohydrate antigen 72-4; TM, tumor marker. |
 | Fig. 2Correlation of each stage and tumor marker cutoff ratio. There was a tendency toward increasing tumor marker levels with advancing cancer stage with (A) carcinoembryonic antigen (CEA) being positive in 6.1% of stage I, 16,7% in stage II, 19.9% in stage III, and 24.7% in stage IV cancers (P < 0.001). (B) For carbohydrate antigen 19-9 (CA 19-9), a similar increasing pattern was found with 4.0% positive in stage I, 6.8% in stage II, 13.9% in stage III, and 24.1% in stage IV cancers (P < 0.001). (C) Carbohydrate antigen 72-4 (CA 72-4) exceeded our defined threshold in 7.4% of stage I, 16.7% of stage II, 13.1% of stage III, and 33.3% of stage IV cancers, but there were no significant differences between the stages (P = 0.085). CI, confidence interval. |
 | Fig. 3Risk of recurrence by tumor marker cutoff ratio (TMR) of carcinoembryonic antigen (CEA), carbohydrate antigen 19-9 (CA 19-9), and carbohydrate antigen 72-4 (CA 72-4). (A) CEA shows significant difference in 5-year risk of recurrence between the TMR < 1.0, 1.0 ≤ TMR < 2.0, and 2.0 ≤ TMR groups, with results of 18.3%, 29.8%, 61.4% (P < 0.001). (B) CA 19-9 shows 5-year risk of recurrence of 19.7%, 35.6%, 58.4% between the TMR < 1.0, 1.0 ≤ TMR < 3.0, and 3.0 ≤ TMR groups, respectively with significant difference (P < 0.001). (C) CA 72-4 shows significant difference between the TMR (<1.0) group and groups with TMR higher than 1.0, resulting in of 15.2% and 33.6%, respectively (P < 0.001). NS, nonspecific. |
 | Fig. 4Risk of recurrence according to the tumor marker cutoff ratio (TMR) combination scoring system. TMR combination scoring system (the sum of the scores) was divided into four categories (score 0, score 1, score 2, score 3 and above). Five-year risk of recurrence for each category were 12.8%, 23.9%, 45.5%, and 68.3%, respectively (P < 0.05). |
References
1. Tsugane S, Sasazuki S. Diet and the risk of gastric cancer: review of epidemiological evidence. Gastric Cancer. 2007; 10:75–83.
2. Nam MJ, Oh SJ, Oh CA, Kim DH, Bae YS, Choi MG, et al. Frequency and predictive factors of lymph node metastasis in mucosal cancer. J Gastric Cancer. 2010; 10:162–167.
3. Ministry of Health and Welfare. 2002 Annual Report of the Korea Central Cancer Registry. Seoul: Ministry of Health and Welfare;2005.
4. Sobin LH, Wittekind CH. International Union Against Cancer (UICC). TNM classification of malignant tumours. 6th ed. New York: John Wiley-Liss;2002.
5. Marrelli D, Roviello F, De Stefano A, Farnetani M, Garosi L, Messano A, et al. Prognostic significance of CEA, CA 19-9 and CA 72-4 preoperative serum levels in gastric carcinoma. Oncology. 1999; 57:55–62.
6. Ucar E, Semerci E, Ustun H, Yetim T, Huzmeli C, Gullu M. Prognostic value of preoperative CEA, CA 19-9, CA 72-4, and AFP levels in gastric cancer. Adv Ther. 2008; 25:1075–1084.
7. Ychou M, Duffour J, Kramar A, Gourgou S, Grenier J. Clinical significance and prognostic value of CA72-4 compared with CEA and CA19-9 in patients with gastric cancer. Dis Markers. 2000; 16:105–110.
8. Choi SR, Jang JS, Lee JH, Roh MH, Kim MC, Lee WS, et al. Role of serum tumor markers in monitoring for recurrence of gastric cancer following radical gastrectomy. Dig Dis Sci. 2006; 51:2081–2086.
9. Choi KW, Kim HY, Park NG, Kwak NJ, Park KT, Eom JH, et al. Clinical value of serum CA 72-4 as a tumor marker for gastric carcinoma. Korean J Gastroenterol. 1996; 28:164–171.
10. Lai IR, Lee WJ, Huang MT, Lin HH. Comparison of serum CA72-4, CEA, TPA, CA19-9 and CA125 levels in gastric cancer patients and correlation with recurrence. Hepatogastroenterology. 2002; 49:1157–1160.
11. Na KY, Chang YS, Kim YH, Joo SH, Lee SH. The prognostic significance of the preoperative serum CEA, CA19-9 and AFP levels in gastric cancer patients. J Korean Surg Soc. 2008; 75:302–306.
12. Takahashi Y, Takeuchi T, Sakamoto J, Touge T, Mai M, Ohkura H, et al. The usefulness of CEA and/or CA19-9 in monitoring for recurrence in gastric cancer patients: a prospective clinical study. Gastric Cancer. 2003; 6:142–145.
13. Gold P, Freedman SO. Specific carcinoembryonic antigens of the human digestive system. J Exp Med. 1965; 122:467–481.
14. Zhou H, Stanners CP, Fuks A. Specificity of anti-carcinoembryonic antigen monoclonal antibodies and their effects on CEA-mediated adhesion. Cancer Res. 1993; 53:3817–3822.
15. Baek SW, Cho DH, Yoo CH, Han WK. Prognostic value of preoperative serum CEA and CA19-9 levels in gastric cancer patients. J Korean Surg Soc. 2004; 66:27–32.
16. Soeth E, Wirth T, List HJ, Kumbhani S, Petersen A, Neumaier M, et al. Controlled ribozyme targeting demonstrates an antiapoptotic effect of carcinoembryonic antigen in HT29 colon cancer cells. Clin Cancer Res. 2001; 7:2022–2030.
17. Obrink B. CEA adhesion molecules: multifunctional proteins with signal-regulatory properties. Curr Opin Cell Biol. 1997; 9:616–626.
18. Berg EL, Robinson MK, Mansson O, Butcher EC, Magnani JL. A carbohydrate domain common to both sialyl Le(a) and sialyl Le(X) is recognized by the endothelial cell leukocyte adhesion molecule ELAM-1. J Biol Chem. 1991; 266:14869–14872.
19. Koprowski H, Steplewski Z, Mitchell K, Herlyn M, Herlyn D, Fuhrer P. Colorectal carcinoma antigens detected by hybridoma antibodies. Somatic Cell Genet. 1979; 5:957–971.
20. Kannagi R. Molecular mechanism for cancer-associated induction of sialyl Lewis X and sialyl Lewis A expression-The Warburg effect revisited. Glycoconj J. 2004; 20:353–364.
21. Del Villano BC, Brennan S, Brock P, Bucher C, Liu V, McClure M, et al. Radioimmunometric assay for a monoclonal antibody-defined tumor marker, CA 19-9. Clin Chem. 1983; 29:549–552.
22. Johnson VG, Schlom J, Paterson AJ, Bennett J, Magnani JL, Colcher D. Analysis of a human tumor-associated glycoprotein (TAG-72) identified by monoclonal antibody B72.3. Cancer Res. 1986; 46:850–857.
23. Duraker N, Celik AN. The prognostic significance of preoperative serum CA 19-9 in patients with resectable gastric carcinoma: comparison with CEA. J Surg Oncol. 2001; 76:266–271.
24. Kim DY, Kim HR, Shim JH, Park CS, Kim SK, Kim YJ. Significance of serum and tissue carcinoembryonic antigen for the prognosis of gastric carcinoma patients. J Surg Oncol. 2000; 74:185–192.
25. Kochi M, Fujii M, Kanamori N, Kaiga T, Kawakami T, Aizaki K, et al. Evaluation of serum CEA and CA19-9 levels as prognostic factors in patients with gastric cancer. Gastric Cancer. 2000; 3:177–186.
26. Park SH, Kim DY, Heo JS, Lim DH, Park CK, Lee KW, et al. Postoperative chemoradiotherapy for gastric cancer. Ann Oncol. 2003; 14:1373–1377.
27. Marrelli D, Pinto E, De Stefano A, Farnetani M, Garosi L, Roviello F. Clinical utility of CEA, CA 19-9, and CA 72-4 in the follow-up of patients with resectable gastric cancer. Am J Surg. 2001; 181:16–19.
28. Yasasever V, Sengun Z, Saydan N, Onat H, Dalay N. Serum values of CA72.4 in patients with gastrointestinal system tumors comparison with CEA and CA 19.9. Eur J Gynaecol Oncol. 1992; 13:403–408.




 ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download