Abstract
Purpose
Studies of liver anatomy have developed alongside clinical achievements, as these types of research complement each other. The aim of this study is to determine whether or not the portal vein branches (P4d) in 'Nagino's trisectionectomy' exist, and to examine their characteristics using cadaver dissection.
Methods
From April 2012 to July 2012, 31 adult cadavers were delicately dissected. We defined a 'NewGP' as an extra glissonian pedicle (GP) other than the traditional GPs that supply segments II, III, IVa, and IVb in the ordinary direction, and anatomically located superior to the umbilical fissure (UF).
Controversies regarding the anatomy of the liver have not yet been fully resolved, even among liver surgeons. Classical anatomic classifications such as those of Couinaud [1] and Healey and Schroy [2] are based on the characteristics of the portal vein and bile duct, respectively. More recently, Ryu and Cho [3] provided a new anatomic description based on the portal segmentation and drainage veins. Universal terminology for hepatic anatomy and liver resection has only recently been adopted [4].
The left hemiliver is known to vary with regard to the number of glissonian pedicles (GPs) compared to those of the right hemiliver, which illustrates the sliding origin of the glissonian pedicle [5]. Strasberg [6,7] criticized Couinaud's classification, insisting that the umbilical fissure (UF) is a landmark for the border of the left medial and lateral sections as based on Healey's classification. Actually, the left medial section is much larger in area and volume than the lateral section according to Couinaud. On the contrary, when we consider the UF as a border landmark based on Healey's classification, the area and volume of the left medial and lateral sections are similar to each other. Couinaud [8] partly agreed with Strasberg's criticism, but he maintains that the umbilical fissure vein (UFV; tributary of the left hepatic vein) should be considered a portal fissure, and that resection of the academic lobe is a portal resection.
Meanwhile, many liver resection and liver transplantation surgeries are performed worldwide, and clinical outcomes have recently improved. Studies of liver anatomy have developed alongside clinical and technical achievements, and these types of research complement each other. One of the new pioneering technical advancements, 'the hanging maneuver', was recently introduced [9] and consequential anatomical studies have been published [10,11]. We developed 'a ventral hilum exposure method' for liver resection [12,13], which was based on anatomical studies relevant to this specific surgical technique [14,15].
Recently, Nagino et al. [16] reported an anatomic right liver trisectionectomy. Several branches of the umbilical portion of the portal vein (P4d) [17] were carefully ligated, and then the cranial side of the umbilical portion of the left portal vein was completely detached from the umbilical plate. This maneuver was one of the important points they emphasized in their article. However, P4d are somewhat odd and unfamiliar to many surgeons, and this may make them hesitant to accept and apply Nagino's procedure in patients undergoing liver trisectionectomy.
The aim of this study is to determine whether or not portal vein branches (P4d) exist, and evaluate their characteristics using cadaver dissection. We believe our study provides more scientific evidence in support of Nagino's anatomic trisectonectomy as did other anatomical studies for the hanging maneuver and our ventral hilum exposure method.
Here, we document for the first time new GPs, including P4d, observed superior to the UF during cadaver dissection, and we discuss the clinical significance of these structures in liver surgery.
We dissected thirty-one adult cadavers from April 2012 to July 2012. The specimens were delicately dissected simultaneously from the visceral (inferior) and diaphragmatic (superior) surfaces. The hepatic parenchyma was removed using mosquito clamps under direct vision in order to identify the GP and hepatic veins. Two hepatobiliary surgeons who each had ten years of experience operating on patients with liver disease participated in the dissections.
All identified GPs were dissected, except those with a diameter less than 1 mm. The left and middle hepatic veins and their branches were dissected, except in cases of vasculature with a diameter less than 1 mm. We estimated the number of II, III, Iva, and IVb segment GP. The number of 'additional pedicles' introduced by Launois and Jamieson [18] and their diameters were also determined. We followed the hepatic vein classification system described by Reichert et al. [19]. Type A is union of segment II and III hepatic veins to form the principal left hepatic vein at the UF. Type B involves separate large hepatic veins, each draining an individual segment that unite to form the left hepatic vein at the level of the inferior vena cava. Type C is a union of segment II and III draining hepatic veins in the liver parenchyma to form the left hepatic vein lateral to the UF.
Unexpectedly, we found variation or new GP during the cadaver dissection. We defined these newly identified GPs ('NewGPs') as extra glissonian pedicles other than the traditionally described GPs that supply the II, III, IVa, and IVb segments, and are anatomically located superior to the UF. We subdivided the 'NewGPs' into 'II NewGPs', 'III NewGPs', 'IVa NewGPs', 'IVb NewGPs', and 'central NewGPs' (neutral to traditional GP) according to their distance from the traditional GP origin. 'Central NewGPs' had the same or very similar distances from the traditional GP origin.
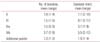
The characteristics of traditional GPs, including segments II, III, IVa, IVb, and the additional pedicles are reported in Table 1. One to four segment II GPs were found in each case, and had an average diameter of 7.7 mm. We found one to five segment III GPs in each case with average diameter of 9.7 mm. There were zero to three segment IVa GPs in each case, and the average diameter was 3.7 mm. Two to five segment IVb GPs were identified in each case, and they had an average diameter of 5.5 mm. The overall incidence of additional pedicles was one to two in each case, with an average diameter of 1.9 mm.
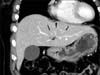
The II and III segment GPs of the left hemiliver are shown in Fig. 1, and the IVa and IVb segment GPs of the left hemiliver are shown in Fig. 2.
Additional pedicles are shown in Fig. 3. All cases in this study had the pedicles in addition to those of the IVa segment. These pedicles originated just before II GP origin, not just after the II GP origin. We analyzed the characteristics of the left hepatic vein and the UFV, and the results are reported in Table 2. Based on the methods described by Reichert et al. [19], all of the left and middle hepatic vein types can be seen in Fig. 4. All the left hepatic veins were mainly type A, with an incidence of 67.8%. The UFV was identified in only 83.8% of cases. The UFV mainly drained into the left hepatic vein, with an incidence of 88.5%. The incidence of drainage into the middle hepatic vein was 3.8%, and independent drainage from the left hepatic vein or middle hepatic vein was identified in 7.6% of cases. Case-by-case descriptions of the UFV are provided in Fig. 5. Five cases had no definite UFV.
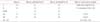
We identified a pedicle as a 'NewGP' based on the UF (Table 3). The incidence of 'NewGPs' was 30/31 (96.8%). 'Central NewGPs' were the most prevalent (28/31, 90.3%), and 'II NewGPs' were the least prevalent (6/31, 19.4%). The diameters of these 'NewGPs' ranged from 3.5 to 5.6 mm, which was not significantly different compared to traditional GPs, having a diameter ranging from 3.7 to 9.7 mm (Table 1). Typical 'NewGPs' are shown in Figs. 6, 7. These cases had several 'NewGPs' superior and perpendicular to the UF, which clearly differentiates them from the traditional GPs.
There are various methods for examining cadaver livers, including dissection, casting, radiology, and ultrasound [14,20]. Each of these methods has advantages and disadvantages. We believe that the most critical factor is how thoroughly the investigator examines the morphology in adherence to their intentions. We used the method of dissection to evaluate the anatomy of liver GPs. Without casting, we could not distinguish arteries, portal veins and bile ducts, but the GPs we dissected corresponded primarily to the portal vein anatomy. The dissectors in our study were hepatic surgeons who had been practicing for ten years each, and the dissection protocol was similar to that used for clinical hepatic resection; mainly the glissonian pedicle approach. This method of dissection is very familiar to many surgeons, and thus the contribution of anatomists need not be included in this study.
The characteristics of the GPs for segments II, III, IVa, and IVb were similar to those of findings described in other studies in terms of the number and structure of the pedicles [5,18,21]. We found 'NewGPs' through cadaver dissection. Multiple 'NewGPs' were noted, and were usually located between the left medial and left lateral sections. We analyzed the number of GPs, including 'NewGPs' based on the UF and the UFV (Table 4). When considering only traditional GPs in this study, the incidence of segments II, III, IVa, and IVb was 1.8, 1.5, 1.5, and 3.7, respectively. When considering 'NewGPs' based on both the UF and the UFV, the incidence of all GPs increased. A greater increase in segment III GPs was noted when 'NewGPs' were identified based on the UFV, because we found many UFVs were located very close to the origins of 'central NewGPs'. Most UFVs originated from the left hepatic vein, and we classified cases of 'central NewGP' that were very close to the UFV as part of the left lateral section. Of course, we think that these 'central NewGPs' could be segment IVb GPs rather than segment III GPs. Summing the number of 'NewGPs' and traditional pedicles indicated that we found many more pedicles than two previous studies [18,21], and a similar number to one prior study [5] (Table 4). Retrospectively, we believe that the absence of 'NewGPs' in our previous study [21] was by chance. One possible reason is that we dissected from only the visceral (inferior) surface. Couinaud [5] described multiple branches of the umbilical portion of GPs but he classified these branches into segment IVa or IVb GPs. We posit that all 'NewGPs' are not necessarily IVa or IVb GPs, and that they are partly II and III GPs as well as IVa or IVb GPs. Additionally, we did find that 'central NewGPs', 'II NewGPs', and 'III NewGPs' were not part of Couinaud's description.
We proposed that Healey's classification is superior to Couinaud's in its description of the left lateral section and the medial section [22]. When we used the UF as a landmark, we could almost always localize 'NewGPs' (30/31, 96.8%). In addition, it was frequently difficult to classify 'central NewGPs' as traditional III or IVb GP. This is one of the reasons we can insist that 'NewGPs' really are new. We believe that 'central NewGPs' together with the UF can serve as a new border between the left medial section and lateral section.
There was a problem using UFV as a landmark for 'NewGP' as much as using UF. There were several ambiguous situations with regard to variation in the characteristics of the UFV. Most 'central NewGPs' could be classified as one of the traditional GPs, III or IVb. In two cases, 'central NewGPs' could not be classified into any traditional category because the UFV was not apparent and all 'central NewGPs' had a similar distance from the left and middle hepatic veins (Fig. 5D). Couinaud [8] reported that only 29% of cases had a long tributary following the length of the UF, and Hwang et al. [23] reported that only 35.4% of cases had a prominent UFV.
The tip of the 'NewGP' can be seen clinically with commonly-used imaging techniques such as computed tomography. However, what is seen is only the portal vein of the 'NewGP' (Fig. 8). More studies focused on this specific area of liver anatomy are necessary to define this new GP or more accurately identify it as a variation or a branch of a GP.
When we perform anatomical resection of the liver with procedures such as left lateral sectionectomy or left hemihepatectomy, clinical outcomes of the surgery are rarely affected because the clamping and ligation of the 'NewGP' do not cause significant discoloration of the remnant liver. The 'NewGP' may also be comparably less prevalent and may not result in unfavorable patient progression. We believe the clinical significance of the 'NewGP' is supplementing the traditional GPs including II, III, IVa, and IVb pedicles in supplying the liver. For example, cases 9 and 13 had no IVa GP in the left medial section. Case 9 had its supply from the common origin of the IVb GP, and had one additional pedicle with no 'NewGP'. Case 13 had its supply from the common origin of the IVb GP, and had one additional pedicle with one instance of a 'IVa NewGP'. Thus, we can conclude that traditional GPs and additional pedicles as well as 'NewGPs' simultaneously supply this region of the liver.
We think Nagino's P4d [16] correspond to the 'IVa NewGP' in the present study and the additional pedicle described by Launois and Jamieson [18]. 'Additional pedicles' just before the segment II glissonian branch were found in all the cases in this study. These structures coursed over the left hepatic vein and linked to some portion of the IVa segment. We reported additional pedicles in a previous study [21]. We believe the characteristics reported in that study and those identified in the present study are consistent with the findings reported in Launois' textbook [18]. We suggest a schematic illustration (Fig. 9) for NewGP and additional pedicle, which is modified from Couinaud's description [5] based on this study.
In conclusion, we think that the P4d in Nagino's trisectionectomy [16] are the same as the 'IVa NewGPs' in the present study and the additional pedicles described by Launois and Jamieson [18]. This is the first study to report variations or new GPs, which could serve as part of the border between the left medial section and lateral section. We believe its clinical significance is supplementing the traditional II, III, IVa, and IVb pedicles in supplying the liver. Additionally, these findings can be applied to liver surgery such as right trisectionectomy using the conventional (separative) technique or glissonian approach.
Figures and Tables
 | Fig. 1Case 16 shows segment II and III GPs of the left hemiliver. Some part of the left hepatic vein was lifted upward in the field. The forcep indicates additional pedicle. GP, glissonian pedicle; LHV, left hepatic vein; LMS, left medial section. |
 | Fig. 2Case 10 shows segment IVa and IVb GPs of the left hemiliver. GP, glissonian pedicle; LMS, left medial section; LLS, left lateral section. |
 | Fig. 3Case 1 shows additional pedicle (arrow) and one of NewGP (arrowheads). GP, glissonian pedicle; LMS, left medial section. |
 | Fig. 4Drainage pattern of the left and middle hepatic vein according to Reichert et al. [12]. (A) Type A: Case 4 shows a union of segment II and III veins to form a principal left hepatic vein at the UF. (B) Type B: Case 16 shows separate large veins, each draining an individual segment, that united to form the left hepatic vein at the level of the inferior vena cava. (C) Type C: Case 21 shows a union of segment II and III draining veins in the parenchyma of the graft to form the left hepatic vein medial to the UF. LHV, left hepatic vein; MHV, middle hepatic vein; UF, umbilical fissure; LMS, left medial section. |
 | Fig. 5Multiple types of the UFV, case by case. (A) Case 3 shows the UFV (arrowheads) from left hepatic vein. (B) Case 22 shows the UFV (arrowheads) from the middle hepatic vein. (C) Case 1 shows the UFV (arrowheads) independent on the left hepatic vein or middle hepatic vein. (D) Case 2 shows no definite UFV related to the left hepatic vein or middle hepatic vein. Forceps indicates the branches of the left hepatic vein and middle hepatic vein, respectively. LHV, left hepatic vein; MHV, middle hepatic vein; UF, umbilical fissure; UFV, umbilical fissure vein; LMS, left medial section; LLS, left lateral section. |
 | Fig. 6NewGPs of case 8. Panels A and B show that three NewGPs are located superior (anatomically) and perpendicular to the UF between the UFV and III GP. (C) Two fingers push III NewGP and IVb NewGP. A 'central NewGP' appears between them. GP, glissonian pedicle; UF, umbilical fissure; UFV, umbilical fissure vein; LMS, left medial section; LLS, left lateral section. |
 | Fig. 7NewGPs of case 5. This panel shows that 'IVa NewGP' (arrows) is located superior (anatomically) to the UF near traditional IVa GP (arrowheads). GP, glissonian pedicle; UF, umbilical fissure; LMS, left medial section; LLS, left lateral section; MHV, middle hepatic vein; LHV, left hepatic vein. |
 | Fig. 8Computed tomography of a 54-year-old woman shows the only portal vein of 'NewGP' that was located anatomically superior to the umbilical fissure. From left to right, arrows and a long arrowhead indicate 'IVb NewGP', 'central NewGP', and 'III NewGP'. GP, glissonian pedicle. |
 | Fig. 9Schematic illustration of NewGP and additional pedicle compared with traditional GPs. 'A' (branches filled with black color) shows a traditional IVa GP, a IVa NewGP, an additional pedicle, and a II NewGP from left to right. 'B' (branches filled with black color) shows a IVb NewGP, a central NewGPs, and a III NewGP from left to right. GP, glissonian pedicle. |
References
1. Couinaud C. Controlled hepatectomies and exposure of the intrahepatic bile ducts: anatomical and technical study. Paris: C. Couinaud;1981.
2. Healey JE Jr, Schroy PC. Anatomy of the biliary ducts within the human liver; analysis of the prevailing pattern of branchings and the major variations of the biliary ducts. AMA Arch Surg. 1953; 66:599–616.
3. Ryu M, Cho A. New liver anatomy: portal segmentation and the drainage vein. New York: Springer;2009.
4. Strasberg SM. Nomenclature of hepatic anatomy and resections: a review of the Brisbane 2000 system. J Hepatobiliary Pancreat Surg. 2005; 12:351–355.
5. Couinaud C. Portal segmentation. In : Couinaud C, editor. Controlled hepatectomies and exposure of the intrahepatic bile ducts: anatomical and technical study. Paris: C. Couinaud;1981. p. 9–17.
6. Strasberg SM. Terminology of liver anatomy and liver resections: coming to grips with hepatic Babel. J Am Coll Surg. 1997; 184:413–434.
7. Botero AC, Strasberg SM. Division of the left hemiliver in man: segments, sectors, or sections. Liver Transpl Surg. 1998; 4:226–231.
8. Couinaud C. Liver anatomy: portal (and suprahepatic) or biliary segmentation. Dig Surg. 1999; 16:459–467.
9. Belghiti J, Guevara OA, Noun R, Saldinger PF, Kianmanesh R. Liver hanging maneuver: a safe approach to right hepatectomy without liver mobilization. J Am Coll Surg. 2001; 193:109–111.
10. Sato TJ, Hirai I, Murakami G, Kanamura T, Hata F, Hirata K. An anatomical study of short hepatic veins, with special reference to delineation of the caudate lobe for hanging maneuver of the liver without the usual mobilization. J Hepatobiliary Pancreat Surg. 2002; 9:55–60.
11. Hirai I, Murakami G, Kimura W, Kanamura T, Sato I. How should we treat short hepatic veins and paracaval branches in anterior hepatectomy using the hanging maneuver without mobilization of the liver? An anatomical and experimental study. Clin Anat. 2003; 16:224–232.
12. Kim BW, Wang HJ, Kim WH, Kim MW. Favorable outcomes of hilar duct oriented hepatic resection for high grade Tsunoda type hepatolithiasis. World J Gastroenterol. 2006; 12:431–436.
13. Kim IG, Jeon JY, Jung JP, Chon SE, Kim HJ, Kim DJ, et al. Totally laparoscopic left hemihepatectomy using ventral hilum exposure (VHE) for intrahepatic bile duct stone. J Laparoendosc Adv Surg Tech A. 2010; 20:143–146.
14. Kwon D, Murakami G, Hata F, Wang HJ, Chung MS, Hirata K. Location of the ventral margin of the paracaval portion of the caudate lobe of the human liver with special reference to the configuration of hepatic portal vein branches. Clin Anat. 2002; 15:387–401.
15. Kwon D, Murakami G, Wang HJ, Chung MS, Hata F, Hirata K. Ventral margin of the paracaval portion of human caudate lobe. J Hepatobiliary Pancreat Surg. 2001; 8:148–153.
16. Nagino M, Kamiya J, Arai T, Nishio H, Ebata T, Nimura Y. "Anatomic" right hepatic trisectionectomy (extended right hepatectomy) with caudate lobectomy for hilar cholangiocarcinoma. Ann Surg. 2006; 243:28–32.
17. Takayasu K, Moriyama N, Muramatsu Y, Shima Y, Goto H, Yamada T. Intrahepatic portal vein branches studied by percutaneous transhepatic portography. Radiology. 1985; 154:31–36.
18. Launois B, Jamieson GG. Segmentectomy procedures: the leftliver. In : Launois B, Jamieson GG, editors. Modern operative techniques in liver surgery. New York: Churchill Livingstone;1993. p. 51–65.
19. Reichert PR, Renz JF, D'Albuquerque LA, Rosenthal P, Lim RC, Roberts JP, et al. Surgical anatomy of the left lateral segment as applied to living-donor and split-liver transplantation: a clinicopathologic study. Ann Surg. 2000; 232:658–664.
20. Hata F, Hirata K, Murakami G, Mukaiya M. Identification of segments VI and VII of the liver based on the ramification patterns of the intrahepatic portal and hepatic veins. Clin Anat. 1999; 12:229–244.
21. Kim IG, Park JW, Kim BW, Wang HJ, Lee BH, Kim MW. Safety of 'isolated IVb (inferior) resection of the liver' by cadaver dissection. Korean J Hepatobiliary Pancreat Surg. 2005; 9:1–5.
22. Kim IG, Park JW, Lee TH, Kim BW, Wang HJ, Kim MW. Surgical anatomy of left lobe of the liver (Couinaud's and Healey's anatomy) through Korean cadaver liver dissection. Korean J Hepatobiliary Pancreat Surg. 2005; 9:73–77.
23. Hwang S, Lee SG, Choi ST, Moon DB, Ha TY, Lee YJ, et al. Hepatic vein anatomy of the medial segment for living donor liver transplantation using extended right lobe graft. Liver Transpl. 2005; 11:449–455.




 ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download