Abstract
Abdominal wall defect with large duodenal disruption after penetrating abdominal injury is a rare emergency situation that can result in life-threatening complications. We report on a 64-year-old man who had abdominal wall defect with large duodenal disruption after penetrating abdominal injury. The patient presented with intra-abdominal exsanguinating bleeding, duodenal disruption, and multiple small bowel perforation. The rarity of this complex injury and its initial presentation as a posttraumatic large duodenal disruption with abdominal wall defect warrant its description. The present case indicates that combining a free tissue flap with a covered expandable metallic stent can effectively and successfully repair an abdominal wall defect that is associated with a large duodenal disruption.
Traumatic duodenal injuries with significant tissue loss are rarely seen but are a potentially challenging problem when they occur in either children or adults [1-3]. The incidence of duodenal injury in the literature ranges from 3.7% to 5.0% and it is often accompanied by other abdominal injuries because of its close anatomic relationship with the liver, pancreas, gallbladder, and ampulla of Vater [4]. In uncomplicated cases, the duodenal defect can simply be closed primarily. However, more complex injuries require pyloric exclusion with a gastrojejunostomy or a pancreaticoduodenectomy [5,6]. Several experimental studies have also examined whether other approaches could reduce the morbidity and mortality that is associated with the management of complicated large duodenal defects [7,8].
Several flaps have been used successfully to repair abdominal wall defects, including the rectus femoris muscle, antero-lateral thigh fasciocutaneous, and Sartorius muscle or myocutaneous flaps [9]. However, the reconstruction of an abdominal wall defect that is associated with a large duodenal disruption is clinically challenging and technically demanding. In the present report, we describe an alternative technique for closing an abdominal wall defect that is associated with a large duodenal disruption: a free flap was used with the help of the temporary placement of a covered expandable metallic stent. To our knowledge, this is the first time this approach has been reported.
A 64-year-old man underwent emergency surgery after penetrating abdominal trauma. He had intra-abdominal exsanguinating bleeding, duodenal disruption, and multiple small bowel perforation. Duodenojejunostomy, the resection of about 150 cm of small bowel followed by anastomosis, and bleeding control were performed. Despite of repeated reanastomosis due to anastomosis failure, he developed sepsis and multiorgan failure. Therefore, he was referred to our institution 22 days after the first surgery. A surgical reexploration was performed and it revealed duodenojejunal disruption and multiple enteroenteric anastomosis failure; there was a large amount of bilestained fluid in the abdomen. Since less than 1 m of the small bowel remained, pyloric exclusion or pancreaticoduodenectomy could no longer be considered. Therefore, we performed enteroenterostomy and duodenal primary repair, and placed a feeding tube distal to the perforated duodenum. After massive irrigation, the multiple drain tube was placed.
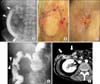
Fortunately, after intensive care, the patient could be transferred to the general ward after ventilator weaning. Enteral feeding through the jejunal feeding tube worked well. However, due to severe retraction of the duodenum, a duodenal disruption gap that was approximately 5 cm long developed. This was associated with an abdominal wall defect (Fig. 1). It was impossible to close either the duodenum or the wall defect primarily. We decided to use a free flap to repair the abdominal wall defect. However, because of persistent leakage of gastric, bile, and pancreatic juice through the duodenal defect, the abdominal wall defect could not be repaired directly with a free flap.
Therefore, the bile and pancreatic juices were diverted first by placing separate pancreatic duct and bile duct drainage tubes by endoscopic retrograde cholangiopancreaticography. Thereafter, the interventional radiologist placed a 16-mm diameter, 90-mm long covered expandable metallic stent (S&G Biotech, Seongnam, Korea) from the duodenal bulb to the jejunum. This successfully reestablished duodenal continuity. Bile and pancreatic juices were diverted through endoscopic nasobiliary drainage and endoscopic nasopancreatic drainage completely. The stent migrated downward 5 days after placement. It was removed through the abdominal defect without difficulty. A second stent was placed from the gastric antrum to the jejunum. It was 16 mm in diameter and 130 mm long (Fig. 2), and thus was much longer than the first stent. The stent was tightly sutured to the duodenum to prevent stent migration.
Seven days after stent placement, the patient underwent debridement and closure of the abdominal wall defect with a free flap. Duodenostomy was performed by placing a drainage tube that decompressed the duodenum and prevented infection. Endoscopic images obtained 3 months after stent placement revealed a widely patent stent, although granulation tissue had formed above the stent. The stent was electively removed 112 days after placement by using a stent removal set. Stent placement and stent removal techniques have been described in detail previously [10]. The pancreatic duct and bile duct drainage tubes were removed 13 days after stent removal.
The patient was able to take food orally after stent removal. The abdominal wall defect had healed completely. A small enterocutaneous fistula was observed. On the 234 th postoperative day, an upper gastrointestinal water-soluble contrast study was performed and showed good passage of contrast with a small enterocutaneous fistula and no significant obstruction (Fig. 3).
Various treatment options have been reported to be effective for the surgical management of large duodenal defects. These include duodenal resection with end-to-end anastomosis, Roux-en-Y duodenojejunostomy, diverticulization, polytetrafluoroethylene patching, omental plug closure, jejunal serosal patching, and pedicled grafts [7,8]. In the present report, a free flap was used with the help of a temporary stent to close a large duodenal defect and an abdominal wall defect. In this case, the patient had less than 1 m of small bowel left due to several previous small bowel resections. Therefore, pyloric exclusion or pancreaticoduodenectomy could not be considered. The main advantage of the alternative technique described in the present report is that it did not involve intestinal resection. It also prevented the possible risk of gastrointestinal contamination, peritoneal soiling, and organ injury.
In our case, severe retraction of the duodenum led to a duodenal disruption that was approximately 5 cm long. Contact between the free flap and the bowel appeared to be an important factor in duodenal prefabrication. An expandable metallic stent successfully reestablished duodenal continuity until the abdominal wall defect had been repaired. The stent was removed 112 days after its placement because of granulation tissue formation above the stent. A postoperative upper gastrointestinal water-soluble contrast study revealed good repair of the abdominal wall defect and the large duodenal disruption. However, the repaired duodenal wall is surrounded with a free flap, and we remain concerned that a fibrotic stricture could occur.
In recent years, expandable metallic stents have been used in many hospitals for the palliative treatment of inoperable malignant gastroduodenal strictures [10]. However, intestinal stent implantation remains potentially controversial because these stents cannot always be removed easily after placement. Stents used to treat a benign gastrointestinal stricture should be designed to be retrievable to prevent long-term complications such as granulation tissue formation and stent migration. In this patient with large duodenal disruption and abdominal wall defect, we placed a fully covered expandable stent to prevent leakage of bile juice and to establish duodenal continuity. We could remove the stent through per-oral route after repair of abdominal wall defect.
Although further clinical trials and extended follow-up studies are needed, the present case indicates that combining a free flap with a covered expandable metallic stent can effectively and successfully repair an abdominal wall defect that is associated with a large duodenal disruption.
Figures and Tables
 | Fig. 1(A) The photograph shows a duodenojejunostomy anastomosis disruption with bile-stained fluid (arrows) and an abdominal wall defect. (B) Fistulography through the two holes at the wound site shows disruption of the duodenum at the duodenojejunostomy anastomosis (arrows). (C) Computed tomographic image shows an open wound at the right abdominal wall (arrows). |
 | Fig. 3(A) A contrast study with a coil catheter that was performed 107 days after surgery shows good flow of contrast medium through the expanded stent (arrows) without leakage of the contrast medium through the defective duodenum (arrowhead). (B) A photograph shows closure of the abdominal wall defect with a free flap with endoscopic nasobiliary drainage and endoscopic nasopancreatic drainage. (C) A photograph made 168 days after surgery shows the complete closure of the abdominal wall defect. (D) A contrast study performed 234 days after surgery shows good passage of the contrast with a small enterocutaneous fistula (arrowheads). (E) Computed tomographic image shows healing of an abdominal wall defect. |
References
1. Asensio JA, Feliciano DV, Britt LD, Kerstein MD. Management of duodenal injuries. Curr Probl Surg. 1993; 30:1023–1093.
2. Ladd AP, West KW, Rouse TM, Scherer LR 3rd, Rescorla FJ, Engum SA, et al. Surgical management of duodenal injuries in children. Surgery. 2002; 132:748–752.
3. Aslan A, Elpek O. The repair of a large duodenal defect by a pedicled gastric seromuscular flap. Surg Today. 2009; 39:689–694.
4. Chen GQ, Yang H. Management of duodenal trauma. Chin J Traumatol. 2011; 14:61–64.
5. Fang JF, Chen RJ, Lin BC. Surgical treatment and outcome after delayed diagnosis of blunt duodenal injury. Eur J Surg. 1999; 165:133–139.
6. Ivatury RR, Nassoura ZE, Simon RJ, Rodriguez A. Complex duodenal injuries. Surg Clin North Am. 1996; 76:797–812.
7. Astarcioglu H, Kocdor MA, Sokmen S, Karademir S, Ozer E, Bora S. Comparison of different surgical repairs in the treatment of experimental duodenal injuries. Am J Surg. 2001; 181:309–312.
8. Nikeghbalian S, Atefi S, Kazemi K, Jalaeian H, Roshan N, Naderi N, et al. Repairing large duodenal injuries in dogs by expanded polytetrafluoroethylene patch. J Surg Res. 2008; 144:17–21.
9. Lin SJ, Butler CE. Subtotal thigh flap and bioprosthetic mesh reconstruction for large, composite abdominal wall defects. Plast Reconstr Surg. 2010; 125:1146–1156.
10. Song HY, Jung HY, Park SI, Kim SB, Lee DH, Kang SG, et al. Covered retrievable expandable nitinol stents in patients with benign esophageal strictures: initial experience. Radiology. 2000; 217:551–557.




 ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download