Abstract
Purpose
Hepatopulmonary syndrome is an arterial oxygenation disorder brought about by advanced liver failure and pulmonary vascular dilatations. The reason why hypoxia develops in hepatopulmonary syndrome depends on the broadening of perialveolar capillary veins. Our study aims to investigate the effects of Flavanoid on hepatopulmonary syndrome through its inhibition of nitric oxide.
Methods
Three groups, each having 8 rats, were formed within the scope of our study. Group I (the control group) only received laparatomy, group II received choledoch ligation, and group III was administered Flavanoid (90% flavonoid diosmin, 10% flavonoid hesperidin) following choledoch ligation. The rats were administered Flavanoid at week two following choledoch ligation. The rats' livers and lungs were examined histopathologically following a five-week follow-up and the perialveolar vein diameters were measured. Arterial blood gases and biochemical parameters were evaluated.
The clinical interactions between the liver and the lungs were first put forward by Flukiger [1] in 1884. Kennedy and Knudson defined hepatopulmonary syndrome (HPS) for the first time in 1977 [2] while it was Krowka and Cortese [3] who determined the diagnosis criteria for HPS.
All the systems in the organism are affected to a certain degree in patients with chronic liver diseases. The lungs are among the most affected organs by the systemic effect brought about by liver failure. HPS is characterized by arterial oxygenation disorder seen with advanced liver failure and pulmonary vascular dilatations [4-6]. The literature states that HPS incidence varies between 12% and 47% [7,8]. The oxygenation problem seen in a significant number of cirrhosis patients is caused by HPS. Fifteen percent of patients with chronic liver failure had PO2 <70 mmHg. Oxygenation is interrupted by the elevation in alveolar-arterial oxygen gradient, which develops following enlargements in pulmonary microcirculation [6,9]. The relationship between the level of liver disease and HPS is still not clear. Although most of the patients have portal hypertension, HPS may develop without the existence of portal hypertension [4,10,11]. The formation mechanism of the syndrome with liver failure, intrapulmonary vascular dilatation, and arterial oxygenation disorder is yet to be known but some theories have been put forward. Studies up to date have reported that arterial oxygenation is disrupted because of intrapulmonary vascular dilatations, pulmonary ateriovenous shunts, low vascular resistance, and increased systemic circulation caused by chronic liver failure.
The reason intrapulmonary vascular dilatation takes place has been the subject of intensive research and many reasons have been investigated within this framework. Experimental studies have focused on endothelium derived nitric oxide and endotelin-1. Some other agents other than these have also been claimed to be responsible but it has been agreed that vascular dilatations were brought about by the common effect of many factors. We, in our study, have aimed to experimentally investigate the effectiveness of Flavanoid, which has a nitric oxide (NO) inhibiting effect, on HPS treatment.
The study was conducted with the consent of Ethics at the Experimental Animal Research Center (April 6, 2010/35).
Twenty-four adult male/female Sprague Dawley rats were divided into 3 groups of 8 rats for the experiments. The rats were anesthetized by intramuscular injection of Ketamine Hydrochloride (2 mg/kg, 10 mg/mL). Only laparatomy was performed on group I (the control group). Ductus choledochus of the rats in group II was dissected, tied with 4/0 silk twice, and cut. Ductus choledochus of the rats in group III was dissected, tied with 4/0 silk twice, and cut between the sutures, and after two weeks Flavanoid (Daflon 500 mg; Les Laboratoires Servier SAS, Neuilly Sur Seine, France) (100 mg/kg) was administered twice daily through a feeding tube. All the rats were fed with standard rat feed. Experimental animals were checked every 12 hours. At the end of week five, all the rats were sacrificed by high dose of Ketamine Hydrochloride anesthesia intramuscularly.
Five milliliters of blood was drawn from the heart for biochemical parameters while 1 mL of blood was drawn from the aorta abdominalis for blood gas evaluations through an injector with heparin. Total bilirubin, direct bilirubin, aspartate aminotransferase (AST), alanin aminotransferase (ALT), and alkaline phosphatase (ALP) values were measured by Olympus/AU 5200 (Konsesyum, Alternative Biomedical Services, Dallas, TX, USA). Blood gas analyses were performed by GEM Premier Plus (Instrumentation Laboratory, Lexington, MA, USA) analyzer.
The dissected tissue was fixed in 10% formaldehyde solution for the histopathological analysis of liver and lung tissues. The dissected sections were processed in an Autotechnicon device and they were stained with hematoxylin-eosine. The evaluation was carried out by a light microscope (×100). The pathologist who performed the evaluation was blind to the group information.
Cirrhosis contraction was determined by the observation of pleomorphism, atypical mitosis, periductal proliferation, and fibrosis in rat livers. The pathological findings were classified as follows: absent, 0; minimal, 1; moderate, 2; severe, 3. Intergroup pathological findings were compared. Pulmonary findings-inflammatory cell infiltration, bronchial wall damage, perialveolar capillary vein enlargement-were compared among the groups. Perialveolar capillary vein diameters were measured by an occulometer by the pathologist. Veins from 6 different lung sections were selected and measured for each rat.
The data collected from the experimental animals were summarized in the form of mean ± standard deviation (SD). The Kruskal-Wallis one-way analysis of variance test, which is a nonparametric test, was used for the statistical analysis. Following that the Mann-Whitney U Test was used with post hoc Bonferroni adjustment. P < 0.05 was set to be the significance level.
No rats were lost during the study. Decrease in daily nutrition and water consumption, weight loss and slowdown in movement were observed in groups II and III.
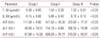
Total bilirubin, direct bilirubin, AST, ALT, and ALP values of groups II and III, which developed cirrhosis by choledoch binding, were significantly higher than group I (P < 0.05). It was seen that biochemical parameters were better in rats that were administered Flavanoid in the choledoch ligation groups (P < 0.05) (Table 1).
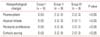
When the cirrhotic rats were compared to the control group, the PO2 value was found to be significantly lower (P < 0.05) (Table 2). When the Flavanoid group was compared to group II it was seen that the PO2 value was significantly better (P < 0.05).
It was observed that the measured oxygen saturation level in cirrhotic groups was significantly worse than the control group. When the Flavanoid group was compared with group II, we saw that O2 saturation value was better. It was also seen that the pH values of the rats in all groups were similar.
Normal liver and lung tissues were seen in the control group (Fig. 1A, D). In the cirrhotic groups II and III, there were neutrophile and mononuclear inflammatory cells (chronic active hepatitis) infiltrated into the parenchyma in the liver around the vena centralis and at periportal distances. Portoportal, porto-central fibrotic bands and cirrhotic nodules were seen (Fig. 1B, C). The perialveolar vein lumens were enlarged and congested in comparison to the control group. Partial damage, neutrophile and mononuclear inflammatory cell infiltration in the pulmonary bronchial walls; fibrin accumulation, thickening and break up on alveolar walls; distinctive congestion and edema in the veins and distinctive dilatation in vein sizes were observed. There were fibrin accumulations and partial thickening in the interstitial field and the capillary walls (Fig. 1E, F).
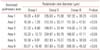
Significantly less parenchymal damage was seen in the Flavanoid (group III) administered rats in comparison to the nonadministered cirrhotic group (group II) (Tables 3, 4). All the histopathological data are summarized in Tables 3 and 4.
It was agreed that the cirrhosis contraction was complete following the evaluation of pleomorphism, atypical mitosis, and periductal proliferation findings in groups II and III. The experimental animals that received choledoch ligation had worse results regarding biochemical and blood gas values and histopathological evaluation results in comparison to the control group (P < 0.05) (Tables 1-3). Group III had better results than group II concerning biochemical, blood gas, and histopathological values (P < 0.05). All the experimental groups had similar pH values.
All the rats with formed obstruction icterus showed increase in the perialveolar vein diameters in the histopathological evaluation of the lungs. This value was statistically significant when compared to the control group (P < 0.05). This increase was the highest in group II and there was a significant difference when compared to group III (P < 0.05). While there was no fibrosis in group I, it was seen that it increased distinctively in groups II and III.
HPS is defined as an arterial oxygenation defect caused by intrapulmonary vascular dilatations related to liver disease [4,5]. The vascular component covers typically diffuse or localized dilated pulmonary capillaries and to a lesser extent pleural and pulmonary arteriovenous links. As a result, HPS includes a clinical triad composed of arterial deoxygenation, intrapulmonary vascular dilatation, and liver malfunction [5]. Although portal hypertension is present in most HPS cases, HPS may be contracted without portal hypertension formation [4]. The fact that HPS did not develop in rats that had only portal hypertension suggests that enlargements in pulmonary veins develop based on the direct and indirect effects of liver failure not based on direct pressure interactivity.
In our study we used a cirrhosis model achieved by the tying of the choledoch duct in rats in order to experimentally investigate the effectiveness of Flavanoid in decreasing intrapulmonary vascular dilatations in HPS and in HPS treatment. This model is compatible with HPS in humans [6,7]. We observed secondary biliary cirrhosis findings in the liver and perialveolar capillary dilatations in the lung at the end of week 5 in rats with bound choledochs. We demonstrated HPS and cirrhosis in these groups of rats in histopathological and biochemical regards.
Perialveolar dilatations in HPS are the main causes of hypoxemia. Enlargements in the veins move the erythrocytes found in the middle of the flow from the endothelia and this, in turn, causes oxygenation failure at different levels [8]. The hyperdynamic condition developing at the final stage liver failure makes the binding of oxygen with hemoglobin in the high-speed blood flow hard [9,10]. The results of our study revealed that there was a significant enlargement in the perialveolar vein diameters and hypoxia in blood gas values in cirrhotic rats in comparison to the control group (P < 0.05). We also saw that this change was significantly better in the Flavanoid administered group in contrast to the group with choledoch ligation, which did not receive Flavanoid (P < 0.05).
The mechanism of pulmonary capillary dilatation in HPS is not exactly known. It is possible that vasodilator agents like platelet activating factor and nitric oxide, atrial natriuretic peptide, and prostacycline are responsible for this condition [6,11]. NO is an important mediator responsible for hyperdynamic circulation in serious liver failure. Animal and human studies have reported that NO production increased in the lungs in cirrhotic patients and that this was an important vasodilator [12,13]. Further, an ample number of studies have shown that NO inhibition would bring about an active benefit in HPS treatment. We used Flavanoid in HPS treatment departing from the fact that it inhibits NO.
Intrapulmonary vascular dilatations in cirrhotic rats through choledoch ligation have been reported with high NO amounts found in the pulmonary homogenates of these rats [13,14]. In the same way, experimental cirrhotic animals achieved through the binding of the main biliary duct have shown increased levels of endotelin-1 (ET-1) in circulation excreted from the biliary epithelia [14]. In direct proportion to this increase, there were also elevations in pulmonary endothelial NO levels and intrapulmonary vascular dilatations. An increase was also seen in ET-1 secretion from the biliary epithelial cells and the related ET-1 levels in human cirrhoses [15]. In HPS, with the secretion of ET-1, which is normally known as a vasoconstructive agent, into the vein lumen, endothelial nitric oxide synthesis is activated and NO levels are elevated. This effect is caused by the ET-1 receptor interactivity in the endothelium. This condition is called endocrine vasodilation and it is only seen in HPS through the systemic effect of ET-1 [6,11,16].
Recent studies suggest that the prevention of oxidative stress may play an important role in the prevention of cholestatic liver damage and the related secondary pathologies. In a study by Kawada et al. [17] concerning the effects of antioxidants on biliary duct obstructions, the authors investigated the effects of antioxidant agents on rat hepatic stellate cell and Kupffer cell functions in a cell culture environment. The regulating functions of both cells are also held responsible for liver damage. As it is seen in the literature, the prevention of oxidative damage in obstruction icterus by antioxidants prevents hepatic damage formation and exerts a cytoprotective effect on the tissue. An ample number of studies in the literature have reported that Flavanoid, which we used in our study, has cytoprotective, antioxidant, and anti-inflammatory effects [18,19]. There is, however, no study that investigates the effects of Flavanoid on HPS and cirrhosis related to cholestatic jaundice. Flavanoid has an antioxidant effect by neutralizing reactive oxygen metabolites and reactive nitrogen metabolites. Besides its antioxidant effect, it becomes effective by inhibiting the activities of inflammatory enzymes and increasing intracellular glutathione synthesis. We determined the positive effects of Flavanoid on liver cirrhosis in rats with formed obstruction icterus through the results of biochemical parameters and histopathological findings. We observed that Flavanoid decreased wide biliary canaliculi, bridging necroses at the periportal distance and around vena centralis, fibroses, and mononuclear cell infiltrations in cirrhotic rats' liver parencyhmal tissues (P < 0.05). This study is the first study that demonstrates the positive effects of Flavanoid on the obstruction icterus and HPS.
In conclusion, the results of our experimental study show that Flavanoid administration significantly decreases fibrosis and oxidative damage in the liver in obstructive jaundice alongside perialveolar vein diameters in the lungs. More comprehensive comparative experimental and clinical studies need to be conducted, however, in order to use Flavanoid clinically in HPS treatment.
Figures and Tables
Fig. 1
(A) Normal parenchymal liver tissue of the rats in control group. (B) Secondary biliary cirrhosis findings developed following choledoch ligation. (C) Wide biliary canaliculi, bridging necrosis at periportal distance and around vena centralis, fibrosis and mononuclear cell infiltration in liver parenchymal tissue of rats in group III. (D) Normal pulmonary tissue of rats in control group. (E) Increase in enlarged perialveolar vein diameter following choledoch ligation in rats of group II. (F) Pulmonary tissue of rats in group III. Increase in perialveolar vein diameter, perialveolar damage, neutrophile and mononuclear cell infiltration findings (H&E, ×100).

References
1. Flukiger M. Vorkommen von Trommelschlagel-formigen Fingerend-phalangen ohne chronische Veranderungen an der Lungen oder an Herzen. Wien Med Wochenschr. 1884; 34:1457.
2. Kennedy TC, Knudson RJ. Exercise-aggravated hypoxemia and orthodeoxia in cirrhosis. Chest. 1977; 72:305–309.
3. Krowka MJ, Cortese DA. Hepatopulmonary syndrome. Current concepts in diagnostic and therapeutic considerations. Chest. 1994; 105:1528–1537.
4. Ho V. Current concepts in the management of hepatopulmonary syndrome. Vasc Health Risk Manag. 2008; 4:1035–1041.
5. Fallon MB. Mechanisms of pulmonary vascular complications of liver disease: hepatopulmonary syndrome. J Clin Gastroenterol. 2005; 39:4 Suppl 2. S138–S142.
6. Chang SW, Ohara N. Pulmonary circulatory dysfunction in rats with biliary cirrhosis: an animal model of the hepatopulmonary syndrome. Am Rev Respir Dis. 1992; 145(4 Pt 1):798–805.
7. Tieppo J, Vercelino R, Dias AS, Silva Vaz MF, Silveira TR, Marroni CA, et al. Evaluation of the protective effects of quercetin in the hepatopulmonary syndrome. Food Chem Toxicol. 2007; 45:1140–1146.
8. Krowka MJ, Cortese DA. Severe hypoxemia associated with liver disease: Mayo Clinic experience and the experimental use of almitrine bismesylate. Mayo Clin Proc. 1987; 62:164–173.
9. Singh C, Sager JS. Pulmonary complications of cirrhosis. Med Clin North Am. 2009; 93:871–883.
10. Rodriguez-Roisin R, Krowka MJ, Herve P, Fallon MB. ERS Task Force Pulmonary-Hepatic Vascular Disorders (PHD) Scientific Committee. Pulmonary-hepatic vascular disorders (PHD). Eur Respir J. 2004; 24:861–880.
11. Lee KN, Yoon SK, Lee JW, Kim KN, Park BH, Kwak JY, et al. Hepatopulmonary syndrome induced by common bile duct ligation in a rabbit model: correlation between pulmonary vascular dilatation on thin-section CT and angiography and serum nitrite concentration or endothelial nitric oxide synthase (eNOS)1 expression. Korean J Radiol. 2004; 5:149–156.
12. Rolla G, Brussino L, Colagrande P, Scappaticci E, Morello M, Bergerone S, et al. Exhaled nitric oxide and impaired oxygenation in cirrhotic patients before and after liver transplantation. Ann Intern Med. 1998; 129:375–378.
13. Fallon MB, Abrams GA, Luo B, Hou Z, Dai J, Ku DD. The role of endothelial nitric oxide synthase in the pathogenesis of a rat model of hepatopulmonary syndrome. Gastroenterology. 1997; 113:606–614.
14. Zhang HY, Han de W, Su AR, Zhang LT, Zhao ZF, Ji JQ, et al. In testinal endotoxemia plays a central role in development of hepatopulmonary syndrome in a cirrhotic rat model induced by multiple pathogenic factors. World J Gastroenterol. 2007; 13:6385–6395.
15. Zhang HY, Han DW, Wang XG, Zhao YC, Zhou X, Zhao HZ. Experimental study on the role of endotoxin in the development of hepatopulmonary syndrome. World J Gastroenterol. 2005; 11:567–572.
16. Sztrymf B, Rabiller A, Nunes H, Savale L, Lebrec D, Le Pape A, et al. Prevention of hepatopulmonary syndrome and hyperdynamic state by pentoxifylline in cirrhotic rats. Eur Respir J. 2004; 23:752–758.
17. Kawada N, Seki S, Inoue M, Kuroki T. Effect of antioxidants, resveratrol, quercetin, and N-acetylcysteine, on the functions of cultured rat hepatic stellate cells and Kupffer cells. Hepatology. 1998; 27:1265–1274.
18. Santus R, Perdrix L, Haigle J, Morliere P, Maziere JC, Maziere C, et al. Daflon as a cellular antioxidant and a membrane-stabilizing agent in human fibroblasts irradiated by ultraviolet A radiation. Photodermatol Photoimmunol Photomed. 1991; 8:200–205.
19. Robak J, Gryglewski RJ. Flavonoids are scavengers of superoxide anions. Biochem Pharmacol. 1988; 37:837–841.




 ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download