Abstract
Preduodenal portal vein, a rare anomaly, could be found in any age groups. In pediatrics it may present with a duodenal obstruction by itself or other coexisting anomalies; however it usually present with an asymptomatic or incidental findings during other surgery in adults. This anomaly has a clinical importance due to the possibility of accidental damage to portal vein. In addition to describing a series of 3 cases with different manifestation in infants, discuss about this anomaly with a review of relevant literature.
Preduodenal portal vein (PDPV) is a rare anomaly presenting an abnormal vascular course, where an anteriorly placed portal vein results from the embryonic mal-development of the portal venous system [1,2]. Although PDPV can occur as an isolated defect, it is typically associated with other congenital anomalies, including heterotaxia or polysplenia syndrome, situs inversus, cardiac defects, malrotation, biliary or duodenal atresia, and annular pancreas. Clinically, symptomatic duodenal obstruction occurs in approximately 50% of patients with this anomaly, caused by itself or coexisting anomalies such as duodenal web, malrotation, and annular pancreas. Most such symptomatic cases occur in the pediatric age group. In the remaining 50% of asymptomatic patients, PDPV is an incidental finding during surgery, typically in adults.
We describe here our experience with 3 cases of PDPV in infants manifesting with varied clinical presentations along with a review of current literature.
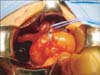
A 10-month-old boy presented to the emergency room with abrupt onset of bilious vomiting. He was born at 39 weeks of gestation by normal vaginal delivery. A complex cardiac anomaly with complete atrioventricular septal defect and malposition of the great arteries was identified during prenatal care, which was surgically corrected at 8 months of age. No obvious gastrointestinal symptoms had occurred previously. Clinical evaluation for vomiting - included upper gastrointestinal (UGI) series radiography, endoscopy, and abdominal computed tomography, these suggested a duodenal obstruction, such as a web. Surgical exploration revealed nonfixation of the midgut without volvulus and no dilatation of the duodenum, however vascular structures and the bile duct were observed to cross over the duodenum with compressing it. The vascular structures were confirmed to be a portal vein and hepatic artery (Fig. 1). Subsequently, gastroduodenostomy was performed to allow these structure lie posterior to the anastomosis site after full mobilization of the duodenum. The postoperative course was uneventful and discharged at 10 days after operation.
An 11-day-old neonate girl presented with severe regurgitation and cyanosis during feeding. She was born at 39 weeks of gestation by cesarean section with a birth weight of 2,730 g. Dextrocardia was identified prenatally. UGI contrast study was performed and showed severe gastroesophageal reflux with delayed passage of contrast to the small bowel. Laparotomy for the reflux was planned before correction of the cardiac problem. During exploratory surgery, we found a vascular structure crossing the duodenum along with hiatal hernia. The vascular structure was confirmed to be a portal vein (Fig. 2). There were also malrotation of intestine and complete situs inversus. After repair of the hiatal defect with accompanying a Nissen fundoplication, a gastroduodenosotmy was performed. The postoperative clinical course was uneventful and she was discharged after undergoing a cardiac operation at 1 month.
A 41-day-old girl presented with jaundice and increased levels of hepatic enzymes. She was born at 37 weeks of gestation by normal vaginal delivery with a birth weight of 2,700 g. Prenatally, a cardiac anomaly with complete atrioventricular septal defect, ambiguous left atrial isomerism, and a large patent ductus arteriosus were identified. On the 7th day after birth, she underwent a correction operation for the cardiac problems with subsequent complete atrioventricular blockade. Jaundice was clinically evaluated and the presence of a choledochal cyst was suggested. During surgical exploration, a portal vein crossing the bulb of the duodenum and a dilated common bile duct was found (Fig. 3). There was also malrotation of intestine. Hepaticojejunostomy after complete excision of a choledochal cyst was performed followed by side-to-side duodenoduodenostomy. She was discharged at 14 days after operation without complication.
The occurrence of PDPV can be explained as an embryonic anomaly resulting from persistent caudal anastomosis between the vitelline veins [1,2]. Although it is an uncommon congenital anomaly, its management is surgically important when encounter. Since the first report concerning this congenital disorder in 1921 [3], less than 100 cases have been described in the literature thus far. Clinically, PDPV can cause a duodenal obstruction by itself or in combination with typically coexisting anomalies [4,5]. As mentioned previously, approximately 50% of patients remain asymptomatic, with PDPV being an incidental finding during other operations or on radiologic studies [6,7].
PDPV in infants has been occasionally reported; however, only a single case presenting with symptomatic duodenal obstruction is usually described. In this case series, PDPV was directly responsible for duodenal obstruction in only 1 of 3 cases. PDPV is typically associated with coexisting cardiac, duodenal, biliary, pancreatic, or splenic anomalies; similar coexistence of these anomalies was also found in our 3 cases. In 1 patient, PDPV was associated with the presence of a preduodenal common bile duct (PDCBD), an extremely rare condition [8]. From an embryologic perspective and considering previous reports of PDCBD, all cases of PDCBD are associated with PDPV, as observed in this case.
The treatment for duodenal obstruction cause by PDPV is bypass surgery. Duodenoduodenostomy or gastroduodenostomy that anteriorly bypasses the portal vein is the preferred method with good clinical outcomes [9,10]. All our cases patients showed an uneventful courses after the bypass surgeries performed.
Although PDPV may be found in adults, given its clinical presentation, it can be regarded as an exclusively pediatric surgical issue. Congenital duodenal obstruction may occur due to various causes; however, it typically presents during the neonatal period. In our series, delayed presentation was observed only in 1 patient with cardiac anomaly; however, most previous cases of symptomatic duodenal obstruction associated with PDPV and other anomalies have been described in infants.
In the present report, we have described 3 different manifestations of PDPV in infants that directly or indirectly caused a duodenal obstruction, with a delayed, uncharacteristic presentation in 1 case. Therefore, this condition should be suspected and focused upon in infants presenting with bilious vomiting and/or poor oral feeding, particular in the presence of coexisting cardiac defects. Moreover, the surgeon should bear in mind the possibility of other coexisting gastrointestinal anomalies, which can lead to the occurrence of surgical accidents. In our series, all the patients showed satisfactory outcomes after surgical correction; however, it is generally difficult to assess the long-term results of such surgeries. We determined that appropriate and timely surgical management of PDPV in infants led to good early clinical outcomes without complications.
We conclude that in infants with severe cardiac anomalies presenting with duodenal obstruction, the possibility of PDPV should be considered.
Figures and Tables
References
1. Marks C. Developmental basis of the portal venous system. Am J Surg. 1969; 117:671–681.
2. Walsh G, Williams MP. Congenital anomalies of the portal venous system: CT appearances with embryological considerations. Clin Radiol. 1995; 50:174–176.
3. Knight HO. An anomalous portal vein with its surgical dangers. Ann Surg. 1921; 74:697–699.
4. Mordehai J, Cohen Z, Kurzbart E, Mares AJ. Preduodenal portal vein causing duodenal obstruction associated with situs inversus, intestinal malrotation, and polysplenia: a case report. J Pediatr Surg. 2002; 37:E5.
5. Esscher T. Preduodenal portal vein: a cause of intestinal obstruction? J Pediatr Surg. 1980; 15:609–612.
6. Ishizaki Y, Tanaka M, Okuyama T. Surgical implications of preduodenal portal vein in the adult. Case report and review of the literature. Arch Surg. 1994; 129:773–775.
7. Ooshima I, Maruyama T, Ootsuki K, Ozaki M. Preduodenal portal vein in the adult. J Hepatobiliary Pancreat Surg. 1998; 5:455–458.
8. Shah OJ, Robbani I, Khuroo MS. Preduodenal portal vein with preduodenal common bile duct: an extremely rare anomaly. Am J Surg. 2009; 197:e43–e45.
9. Georgacopulo P, Vigi V. Duodenal obstruction due to a preduodenal portal vein in a newborn. J Pediatr Surg. 1980; 15:339–340.
10. Choi SO, Park WH. Preduodenal portal vein: a cause of prenatally diagnosed duodenal obstruction. J Pediatr Surg. 1995; 30:1521–1522.




 ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download