Abstract
Xanthogranulomatous cholecystitis (XGC) is a rare form of chronic cholecystitis that is accompanied by xanthomatous histiocytes and chronic inflammation. A 2-month-old boy presented with a right upper abdominal palpable mass. Cholecystectomy with liver wedge resection was done, under the impression that the mass might be a hepatic tumor or liver abscess. Pathologic examination showed XGC with abscess formation. Most cases of XGC were observed in adult and only a few cases were reported in children. We describe a very rare case of XGC in infancy.
Xanthogranulomatous cholecystitis (XGC) is an unusual form of cholecystitis that is accompanied by xanthomatous histiocytes, chronic inflammatory cells, and fibrosis, with varying degrees of involvement of one or all of the layers of the gallbladder wall. XGC is most frequently observed in elderly women aged 50-70 years and is very rare in children [1]. We report a very rare case of XGC in infancy.
A 2-month-old boy presented with a right upper abdominal palpable mass 3 days previously. He was born weighing 2,960 g at the 38th gestational week and no significant event occurred in the gestational period. He had no previous medical problem and appeared well-developed and well-nourished. On physical examination, the mass in the right upper quadrant was firm and palpable, and the patient did not show any pain or tenderness. His body temperature was normal.
Laboratory findings showed the white blood cell count was 35,350/mL with 71% neutrophils, serum C-reactive protein level was elevated at 5.36 mg/dL (normal, 0 to 0.5 mg/dL) and serum alpha fetoprotein level was 1,316.41 ng/mL. Other laboratory findings were unremarkable. There was no evidence of hepatitis B virus, hepatitis C virus, cytomegalovirus or Epstein-Barr virus.
An ultrasonographic scan revealed a 4.5 cm × 4.5 cm × 4.7 cm heterogeneous hypoechoic mass with a lobulated contour at the gallbladder fossa (Fig. 1). The mass was suspected of having anterior subcapsular extension, and neither the gallbladder nor cholelithiasis were visible. Abdominal magnetic resonance imaging (MRI) suggested a probable extrahepatic lesion, 5.3 cm × 4.2 cm × 3.4 cm in size and lobulated, involving the inferior aspect of S4 and S5 of the liver and anterior abdominal wall (Fig. 2). There were multiple nonenhancing areas suggesting abscess pockets were within the mass. The gallbladder was not depicted on MRI. Under the impression that the mass might be a hepatoblastoma, ultrasono-guided biopsy was performed. Only whitish pus and chronic inflamed tissue were aspirated and these findings caused us to change our impression and diagnose liver abscess. Methicillin-resistant Staphylococcus aureus was diagnosed in bacterial culture test of the pus. We used intravenous antibiotics for 11 days but there was no improvement of the lesion.
On exploration, the gallbladder was severely inflamed with spreading of granulation to the liver, ascending colon and abdominal wall. Cholecystectomy with liver wedge resection and curettage of inflammatory tissue at the abdominal wall were performed. No gallstones were identified. Pathologic examination showed XGC with abscess formation and chronic active inflammation with fibrosis in the liver bed (Fig. 3). There were no evidence of perforation of gallbladder and bile duct.
The patient was discharged at 14 days after the surgery. He was planned to be undergone abdominal sonography after 6 months for follow-up with the potential possible malignant change.
XGC was first described by Christensen and Ishak [2] in 1970, and named by McCoy et al. [3] in 1976. The exact cause of XGC is not proven, but according to the commonly accepted hypothesis, this disease starts with obstruction and acute inflammation of the gallbladder. Over 80% of patients with XGC had gallstones that were estimated to be related to the onset of the disease [1,3,4]. When the gallstones or some other factor obstruct the gallbladder and cause acute inflammation, bile enters the stroma through the Aschoff-Rotitansky sinus or inflamed mucosa of gallbladder. Then histiocytes take up and ingest the bile and turn into xanthoma cells that lead to XGC [5].
Clinically, XGC presents as acute or chronic cholecystitis, but biliary colicky pain is not common. XGC is accompanied by severe inflammation and fibrosis that lead to tumor-like thickening of the wall and may form an adhesion with the connective tissue of neighboring organs of the gallbladder such as liver, small intestine, colon, and stomach [6,7]. Adhesions to the abdominal wall are also seen and a case with a fistula to the skin has been reported [8]. These conditions make preoperative diagnosis difficult and sometimes raise suspicion of the presence of a tumorous condition such as advanced gallbladder cancer [6,7]. This case also showed severe adhesion with the liver, ascending colon and abdominal wall, and these findings led to the erroneous diagnosis of hepatoblastoma or other tumorous condition.
Cholecystectomy is considered to be the treatment of choice, because XGC is usually confined to the gallbladder [4,6]. But in cases with extensive involvement of the surrounding organs, some authors recommend resection of all affected tissue [6,9]. Sometimes gallbladder carcinoma may accompany XGC. Intraoperative frozen-section investigation has been suggested as being necessary in diagnosing accompanying gallbladder carcinoma [9].
Figures and Tables
Fig. 1
Transverse ultrasonographic scan shows a heterogeneous hypoechoic mass at the gallbladder (GB) fossa. Small hypoechoic lesion is also noted at the anterior abdominal wall (arrow). Neither GB nor cholelithiasis is visible.

Fig. 2
(A, B) Axial and sagittal enhanced T1-weighted images show a multilobulated mass with heterogeneous enhancement at the inferior and anterior aspect of the liver. There are multiple nonenhancing areas suggesting abscess pockets within the mass. Anterior abdominal wall adjacent to the mass is also involved (arrowheads). The surface of the liver shows indentation by the mass. The gallbladder is not seen on magnetic resonance imaging.
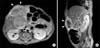
Fig. 3
(A) Gallbladder is surrounded by mononuclear inflammatory cells such as lymphoplasma cells and foamy macrophages (H&E, ×40). (B) Xanthoid cell (foamy macrophage) infiltration is remarkable (H&E, ×600). (C) CD68 immunostaining for macrophages shows heavy infiltration of macrophages around gallbladder wall (×2). (D) CK 7 immunostaining revealed gallbladder mucosa and bile ducts (arrows) in liver parenchyma (×1).

References
1. Goodman ZD, Ishak KG. Xanthogranulomatous cholecystitis. Am J Surg Pathol. 1981; 5:653–659.
2. Christensen AH, Ishak KG. Benign tumors and pseudotumors of the gallbladder. Report of 180 cases. Arch Pathol. 1970; 90:423–432.
3. McCoy JJ Jr, Vila R, Petrossian G, McCall RA, Reddy KS. Xanthogranulomatous cholecystitis: report of two cases. J S C Med Assoc. 1976; 72:78–79.
4. Kim H, Cho Y, Park J. Xanthogranulomatous cholecystitis not associated with gallstone in a 9-year-old girl. J Korean Surg Soc. 2009; 77:72–74.
5. Dixit VK, Prakash A, Gupta A, Pandey M, Gautam A, Kumar M, et al. Xanthogranulomatous cholecystitis. Dig Dis Sci. 1998; 43:940–942.
6. Pinocy J, Lange A, Konig C, Kaiserling E, Becker HD, Krober SM. Xanthogranulomatous cholecystitis resembling carcinoma with extensive tumorous infiltration of the liver and colon. Langenbecks Arch Surg. 2003; 388:48–51.
7. Roberts KM, Parsons MA. Xanthogranulomatous cholecystitis: clinicopathological study of 13 cases. J Clin Pathol. 1987; 40:412–417.
8. Benbow EW. Xanthogranulomatous cholecystitis. Br J Surg. 1990; 77:255–256.
9. Houston JP, Collins MC, Cameron I, Reed MW, Parsons MA, Roberts KM. Xanthogranulomatous cholecystitis. Br J Surg. 1994; 81:1030–1032.
10. Kawana T, Suita S, Arima T, Hirayama Y, Ishii K, Minamishima I, et al. Xanthogranulomatous cholecystitis in an infant with obstructive jaundice. Eur J Pediatr. 1990; 149:765–767.




 ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download