Abstract
Common iliac artery aneurysm (CIA) often occurs in conjunction with an abdominal aortic aneurysm (AAA), which extends into one or both CIAs in 20% to 30% of patients. Conventional endovascular treatment includes coil embolization of the internal iliac artery (IIA), followed by extension of the main bifurcated AAA stent-graft into the external iliac artery. However, complications from intentional occlusion of unilateral or bilateral IIAs are frequent and sometimes serious. Several methods try to preserve the unilateral or bilateral IIA. Here we report a case of concomitant bilateral CIA and AAA successfully treated with bilateral branched iliac stent-grafts.
Common iliac artery aneurysm (CIA) often occurs in conjunction with an abdominal aortic aneurysm (AAA), which extends into one or both of the CIAs in 20% to 30% of patients [1]. Currently, the standard endovascular treatment includes coil embolization of the internal iliac artery (IIA), followed by extension of the main bifurcated AAA stent-graft into the external iliac artery (EIA), which does not allow preservation of the IIA.
Several reports indicated that complications from intentional occlusion of unilateral or bilateral IIAs are frequent in the setting of endovascular aortic repair (EVAR), such as buttock claudication, erectile dysfunction, bowel ischemia, sloughing of the scrotal skin or ischemic injury to the lumbosacral plexus [2,3]. Use of a branched iliac stent-graft is an appealing option, and preliminary data seem promising. However, few cases are reported of bilateral branched graft-stent implantation in iliac artery aneurysms. Here we report a case of concomitant bilateral iliac artery aneurysm and AAA treated successfully with branched stent-grafts.
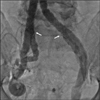
A 65-year-old man was admitted for iliac artery aneurysm, detected during coronary angiogram via femoral artery in another hospital. His electrocardiography and echocardiography were within normal range. Computed tomographic scan showed significant aneurismal dilatation of both iliac arteries and abdominal aorta (Fig. 1). The patient was asymptomatic and underwent elective repair without sign of rupture. The size of right and left CIA was 3.7 mm × 40 mm, 3.7 mm × 41 mm in maximal diameter and length, respectively. Left and right IIA was 36 mm, 15 mm in maximal diameter, respectively. The angulation between left and right CIA and IIA was 40° and 36° respectively. Calcification in both CIA and IIA was not significant. Size of AAA was 37 mm but in risk of further dilatation of the AAA and the difficulty of EVAR after both iliac artery graft stenting, we decided to perform branched iliac bifurcated stenting and EVAR simultaneously.
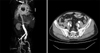
Initially, a custom-made 15-Fr delivery right internal iliac branched device (IIBD, SEAL Bifurcated stent graft, S&G Biotech, Seoul, Korea) was introduced in right femoral artery and oriented under fluoroscopic guidance with the aid of the gold markers. The delivery sheath was withdrawn, and a 0.035-inch guidewire was reintroduced through the branched limb under fluoroscopic guidance from the contralateral femoral artery. After exchange for a stiff guidewire, an 8-Fr internal iliac stent-graft (IISG, SEAL Branched limb extension, S&G biotech, Seoul, Korea) was placed in the IIA to extend the IIBD into proximal IIA. The custom-made left IIBD was then placed from the ipsilateral femoral artery and IISG from the contralateral femoral artery same as above. Finally, conventional EVAR was performed successfully in AAA. The final aortogram showed abdominal and both iliac aneurysms were successfully sealed without any endoleak (Fig. 2). Procedure time was 325 minutes and dose of contrast dye was 160 g. The patient was discharged without complications. Follow-up computed tomography after 1 month showed patent stent but did not showed right renal artery. It might be caused by higher position or stent migration during or after EVAR. However, the patient did not express any discomfort and level of creatinine did not change (Fig. 3).
The distal extension of aneurismal disease to iliac branches of the aorta increases the complexity of EVAR and its consequent morbidity and mortality. Unilateral aortoiliac aneurysms are present in 43%, and bilateral CIA aneurysms in 11% of patients with intact AAA [4]. In such cases EVAR requires distal extension of the aortoiliac endograft beyond the ostium of the IIA and into the EIA, conventionally necessitating the embolization of one or both internal iliac arteries. Unilateral IIA occlusion could be associated with a risk of complications similar to bilateral IIA occlusion, which hypothesizes the use of bilateral IIBDs [5]. Many techniques described for preservation of IIA include relocation of the IIA origin, IIA bypass, bell-bottom grafts, and external-to-internal iliac stent graft with femoro-femoral cross-over [2]. In comparison to these more invasive techniques, the use of internal iliac branch-graft devices offers an appealing endovascular solution. The IIBDs are recently developed devices that offer the possibility of preserving unilateral flow to the IIA during EVAR in patients with aortoiliac aneurysm.
However, complexity of these procedures resulted in prolonged procedural times and increased blood loss in some patients. Furthermore, side branches are unlikely to confer significant device fixation and resistance to migration; therefore, a secure proximal fixation system is of utmost importance.
In previous study, standard morphologic criteria have not been defined or validated. Suggestive criteria include the presence of aneurismal CIA of diameter >24 mm [6,7], the presence of a patent CIA lumen of diameter >18 to 20 mm [7,8], an adequate length of EIA for distal landing of >15 to 20 mm [9], and sufficient length of IIA of >10 mm [10] to secure the branch device. Finally, IIA must be up to 11 mm [8] to receive the iliac branched device (IBD).
Previous reports showed that the rate of technical success varied between 85% and 100% for modern IBDs in current use [2,6-10]. The technical success rate has been shown to improve with time, secondary to the learning curve with IBD deployment and the development of second-generation modular IBDs. The clinical success rate varied 63% to 88% [2,6-10]. Occluded IBDs did not cause aneurysm rupture or sac expansion [2]. In patients whose postoperative IBD occlusion followed initial technical success, 50% manifested symptomatic buttock claudication. Factors associated with technical difficulty predisposing to IBD occlusion include a sharp aortic bifurcation, iliac tortuosity or calcification, the presence of intraluminal CIA thrombi, severe EIA kinking, stenosis of the IIA ostium, IIA atherosclerosis or IIA aneurysm [2]. There was a low endoleak rate. The type I endoleak occurred at the distal sealing zone of the IBD and was managed with additional stent-graft [6]. Type III endoleak occurred at the junction of the IIA limb of the IBD with its main body, which also managed with an interposition of endovascular stent graft [6,10]. Especially, operating time was 101 to 290 minutes, contrast dose was 58 to 108 g in previous studies [1,2]. We took more time and contrast dye compared to previous reports because this is the first experience of bilateral IIBD in Korea. This could change with more experience. The previous report also showed that operating time and contrast dose are different for unilateral or bilateral IIBDs [2].
However, data are limited, and long-term data such as endoleak incidence, sac size changes, and the potential effect of morphologic change should be further investigated. Moreover, patient-tailored graft-stent could be another obstacle to be solved.
In conclusion, IIBD procedures may be performed with relatively safety. Branched devices preserving internal iliac flow do not markedly complicate endograft planning. However, it remains critical to conduct further investigations to evaluate long-term safety and efficacy.
Figures and Tables
 | Fig. 1Maximum intensity projection image shows significant aneurismal dilatation of abdominal aorta and both iliac arteries. |
References
1. Malina M, Dirven M, Sonesson B, Resch T, Dias N, Ivancev K. Feasibility of a branched stent-graft in common iliac artery aneurysms. J Endovasc Ther. 2006; 13:496–500.
2. Karthikesalingam A, Hinchliffe RJ, Holt PJ, Boyle JR, Loftus IM, Thompson MM. Endovascular aneurysm repair with preservation of the internal iliac artery using the iliac branch graft device. Eur J Vasc Endovasc Surg. 2010; 39:285–294.
3. Yun WS, Kim DI, Park UJ, Lee KB, Kim YW, Park KB, et al. Tips for delayed open conversion in patients with a type III endoleak after endovascular aortic aneurysm repair. J Korean Surg Soc. 2010; 78:262–266.
4. Hinchliffe RJ, Alric P, Rose D, Owen V, Davidson IR, Armon MP, et al. Comparison of morphologic features of intact and ruptured aneurysms of infrarenal abdominal aorta. J Vasc Surg. 2003; 38:88–92.
5. Rayt HS, Bown MJ, Lambert KV, Fishwick NG, McCarthy MJ, London NJ, et al. Buttock claudication and erectile dysfunction after internal iliac artery embolization in patients prior to endovascular aortic aneurysm repair. Cardiovasc Intervent Radiol. 2008; 31:728–734.
6. Verzini F, Parlani G, Romano L, De Rango P, Panuccio G, Cao P. Endovascular treatment of iliac aneurysm: Concurrent comparison of side branch endograft versus hypogastric exclusion. J Vasc Surg. 2009; 49:1154–1161.
7. Ziegler P, Avgerinos ED, Umscheid T, Perdikides T, Erz K, Stelter WJ. Branched iliac bifurcation: 6 years experience with endovascular preservation of internal iliac artery flow. J Vasc Surg. 2007; 46:204–210.
8. Tielliu IF, Bos WT, Zeebregts CJ, Prins TR, Van Den Dungen JJ, Verhoeven EL. The role of branched endografts in preserving internal iliac arteries. J Cardiovasc Surg (Torino). 2009; 50:213–218.
9. Serracino-Inglott F, Bray AE, Myers P. Endovascular abdominal aortic aneurysm repair in patients with common iliac artery aneurysms: initial experience with the Zenith bifurcated iliac side branch device. J Vasc Surg. 2007; 46:211–217.
10. Dias NV, Resch TA, Sonesson B, Ivancev K, Malina M. EVAR of aortoiliac aneurysms with branched stent-grafts. Eur J Vasc Endovasc Surg. 2008; 35:677–684.




 ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download