Abstract
Purpose
The goals of this study are to evaluate the effect of duodenojejunal bypass (DJB) for type 2 diabetes mellitus (T2DM) patients below body mass index (BMI) 25 kg/m2 in one year follow-up, and to compare the results of 1 week which we have reported in 2011.
Methods
In this prospective observational study, there were 31 type 2 diabetic patients who underwent DJB at Inha University Hospital from July 2009 to January 2011. We did laboratories such as 75-g oral glucose tolerance test (OGTT), insulin level and hemoglobin A1c (HbA1c), etc. and compared their changes of preoperative, a week, 3 months, and 12 months.
Results
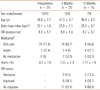
Mean BMI was 23.1 ± 1.3 kg/m2, mean duration of T2DM was 8.3 ± 4.7 and mean age was 46.6 ± 7.7 years. There were a significant decrease of 75-g OGTT levels and increase of insulin secretion after 3 months. 13.3% showed diabetic remission (HbA1c < 6.0, medication cessation) and 26.7% showed diabetic improvement. The rates of remission and improvement much declined comparing with that of postoperative 1 week although those were determined by fasting and postprandial 2 hour level of glucose.
Conclusion
This is the first study of metabolic surgery in Korean diabetes patients in the healthy weight range. DJB exerted positive influences on insulin resistance as well as beta cell function. Early effects on T2DM after DJB could be estimated as one of good modalities, although the effectiveness seems to be unacceptable. Further studies are mandatory for evaluation of the effectiveness of metabolic surgery and finding prognostic factors.
The prevalence of diabetes mellitus is growing globally. According to the 2012 Report on Korean Diabetes Research presented by The Korean Diabetes Association, based on 2010 figures, one in every 10 adults (10.1%) over the age of 30 in Korea suffer from diabetes, while the total number of patients nationwide has reached 3.2 million and this will reach 4.24 million in 2020 and 5.91 million in 2050.
Diabetes mellitus is categorized into types 1 and 2, of which 90% of diabetes patients are type 2 diabetes mellitus (T2DM) and is giving rise to various and serious complications. T2DM is traditionally controlled by changes in lifestyle, dietary measures, oral hypoglycemic agents (OHA) and insulin. Nonsurgical and medical therapy has been a regular method of achieving glycemic 'control', with even the best treatment reducing the hemoglobin A1c (HbA1c) by only 1-2% [1].
Although bariatric surgery was originally developed as a weight-reduction therapy, it has been reported to improve T2DM [2]. Furthermore, experimental studies in rodents [3] and humans [4-7] suggest that certain bariatric procedures may improve diabetes control.
In T2DM patients of a healthy weight (body mass index [BMI] < 30 kg/m2, mainly BMI < 25 kg/m2) who underwent a gastrectomy due to stomach cancer, the authors observed that patients who underwent Roux en Y and Billroth II reconstruction showed a better improvement in blood sugar levels and even the disappearance of diabetes comparative to patients who underwent a Billroth I reconstruction [8]. In that study, it was analyzed that in comparison to the Billroth I, the adjusted prevalence odds ratio is seven times higher in cases of Roux en Y and Billroth II, which bypasses the duodenum and proximal small intestine.
Based on several reports, we performed duodenojejunal bypass (DJB) on T2DM patients with a BMI below 25 kg/m2 and have reported the results observed at postoperative 1 week following the surgery [9]. That study presented improvements of 75-g oral glucose tolerance test (OGTT) as well as being decrease in the levels of insulin secretion with statistical significance. Moreover, 11 patients (44%) showed resolution which was determined just by the glucose level of fasting and postprandial 2 hours, while the duration with diabetes was reported to be the most important predicting factor.
This study presents the results observed one year after surgery, in the form of a follow-up study for the results observed at postoperative 1 week. The primary goal of this study is to evaluate the effect of the DJB for T2DM patients below BMI 25 kg/m2 in the one year follow-up. The second goal is to compare the results of 1 week after the operation with those after 1 year.
This is a prospective study with 31 patients who visited Inha University Hospital from July 2009 to January 2011 due to T2DM. The inclusion criteria were patients of T2DM with a BMI under 25 kg/m2, aged between 20-60 years and who had consented to surgery. Patients of type 1 diabetes, those with severe cardiovascular disorders or malignant tumors, a past medical history indicating an incidence of diabetic coma, problems with the functioning of the liver or other organs, internal secretion illnesses, positive for antiglutamic acid decarboxylase antibodies, as well as the pregnant or those planning pregnancy were excluded. Institutional Review Board approval was obtained and the study was thus commenced (No. Inha 09-58).
In regard to clinical characteristics such as age, gender, presurgery BMI, duration with diabetes and diabetes-related treatment undergone prior to surgery were surveyed, and blood samples for 75-g OGTT, insulin levels, HbA1C and laboratory tests were examined. Changes in DM management methods were assessed in order to determine postoperative status of DM. Each clinical factor was analyzed in both groups of patients who showed an improvement in their diabetes condition following surgery as well as those who did not. Out of the 31 subjects, 21 were tested at postoperative 3 months while 15 were available at 12 months. As for the outliers, the majority of them were located far from the hospital or claimed that there was no need to visit the hospital as their diabetes had improved, and such patients were thus excluded from this study.
All samples were taken after 48 hours without taking DM medication following admission to hospital, for the purpose of minimizing the effects of diabetes control medications in use at the time. Seventy-five-gram OGTT and insulin level were measured in at fasting, 30, 60, 90 and 120 minutes, while HbA1c was also measured at preoperative, postoperative 3 months and 12 months.
The DJB was performed in all patients. All patients chose the open method although it was owed to each patient to choose open or laparoscopic surgery.
A median incision of approximately 8 cm was made in upper abdomen. The greater omentum was opened and dissection between the posterior wall of duodenal bulb and head of the pancreas was performed to distal of duodenum as much as possible. After having the posterior wall of duodenum dissected sufficiently duodenum was stapled and divided at a distance of at least 4 cm from pylorus. Preservation of the right gastric and right gastroepiploic vessels was successful in all patients.
After transecting jejunum 80 cm from the Treitz ligament, end-to-end anastomosis of distal jejunum and duodenum was made. About 80 cm from this anastomosis, end-to-side jejuno-jejunostomy was made. Therefore the common limb began in the lower 160 cm from Treitz ligament.
After surgery, blood sugar was controlled by DM sliding from the day of surgery until postoperative 3rd day by intravenous shorting-acting insulin trying to control and maintain blood sugar levels within the range of 70-130 mg/dL. On postoperative 4th day patients were allowed on to a soft diet, since that, blood sugar levels were only tested and not controlled during admission. On the 7th day 75-g OGTT and insulin were measured and the patient discharged. Patients continued to make regular outpatient visits to undergo checks on whether it was necessary to control their blood sugar levels, and in the case that the blood glucose level exceeded 7.5, prescription of an OHA or insulin were planned in order to control blood sugar levels. 75-g OGTT, insulin and HbA1c were measured at 3 and 12 months.
The definitions for remission are defined as cases HbA1c is below 6% without DM medication. Improvement is defined as in cases in which medication is quitted and HbA1c is below 7%, or when medication is reduced and HbA1c is below 6.5%.
The mean values of 75-g OGTT and insulin in the preoperative period and at postoperative 3 and 12 months were compared using the Wilcoxon signed rank test. Patients were divided into the groups of remission, improvement and nonresponder, The mean values of the resulting clinical factors were compared using the Wilcoxon rank sum test.
All statistical analysis was performed using the IBM SPSS ver. 19.0 (IBM Co., Armonk, NY, USA), and P-values less than 0.05 were considered as results to be kept in mind for statistical purposes.
Clinical parameters of the patients are summarized in Table 1. A total of 31 patients (19 men and 12 women) were included. But we could follow-up just 21 patients at 3 months and 15 patients at 12 months. Demographic data of each time period did not show statistically significant difference and the remission was shown in 2 cases at 3 months and 12 months. One of 2 remissions at 3 months was not followed up and 1 of 8 improved at 3 months was converted into remission. Three improved and 2 nonresponders at 3 months were lost the follow-up. Although we have lost so many patients in following-up, the remission rate would be estimated about 10% and the improvement rate, over 40%. The status of diabetic medication changed significantly. Percentage of no medication increased from 0% to 33.3% for a year.
Fig. 1. is showing the glucose level of 75-g OGTT at each time period. Almost of the levels significantly changed after the surgery (P < 0.05, except basal, 30 minutes at 3 months and basal at 12 months). All of glucose levels at any time period were below that at preoperative. Especially, the curves of 75-g OGTT were transformed more parabolically with time, i.e., the peak level was shown at 120 minutes in the preoperative graph but it was shown earlier in 3 months and 12 months graph as well as the level lowered. That means that DJB got the control of glucose be more physiological.
Fasting glucose level of 12 months showed almost same as that of preoperative but 120 minutes glucose level lowered below 200 mg/dL although the rate of remission or improvement at 12 months was just 40.0%.
Among 15 patients who were followed up till 12 months, none presented higher glucose level than that of preoperative, even in the patients who were classified as nonresponder.
Fig. 2. is presenting insulin level matching with 75-g OGTT. A week after surgery, the levels of insulin were significantly decreased (P < 0.05 at all time) and increased at 3 months and 12 months (P < 0.05, except 60 minutes at 3 months and 12 months). Moreover, all insulin levels after 3 months were higher than that at preoperative. As shown in graph of 75-g OGTT, the graphs were transformed into parabolic pattern as well.
On the contrary, glucose level of 75-g OGTT, insulin level of 1 week was lower than that of preoperative and also, glucose level of that time was lower. Meanwhile, glucose levels of 3 months and 12 months were lower than that of preoperative, but insulin levels of those times were higher than that of preoperative.
Among 15 patients who were followed up till 12 months, none presented lower insulin level than that of preoperative even though the patients were classified as nonresponder, as observed in changes of glucose level.
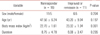
We tried to classify the patients into remission, improved and nonresponder and assess their features. But any clinical parameter was not found to have significant relation with remission or improvement. The reason was thought that the number of patients followed up was too small. Then, we included 12 cases which were not followed up completely and we had the data of HbA1C only, in order to find some meaningful clinical parameters. But we could not find any related clinical parameter for improvement or remission (Table 2).
Actually, we reported that age and diabetic duration would be prognostic factor for improvement or remission in previous paper. In this study the number of the patients who were followed up was too small to find any clinical factor with the statistical significance.
Three patients were admitted to hospital due to marginal ulcer. Two of them were presented abrupt hyperglycemia over 300 mg/dL and 1 of them was presented abrupt hyperglycemia and upper gastrointestinal bleeding. All of them were examined endoscopy and found marginal ulcer. They were prescribed proton pump inhibitor and cured the ulcer and improved hyperglycemia. All of them were the cases early after this study started. (before 15th case) After 15th case, it was mandatory to prescribe proton pump inhibitor (PPI) for 2 months and there was no case of marginal ulcer as of then. We could not meet the abrupt hyperglycemia except in the patients with marginal ulcer. One patient underwent conservative management due to urinary infection. One patient visited outpatient clinic for stitch abscess.
In 2011, authors presented findings showing statistical improvements in the 75-g OGTT following DJB surgery undergone by T2DM patients who were below BMI 25 kg/m2 in the early postoperative period [9]. In that study which is the first report of Asian low BMI patients for DJB, 44% patients in that study showed resolution, not remission which is needed 1-year follow-up. That study was just a week observation and the criteria for resolution was based on 75-g OGTT results. Because these results were obtained only one week following operation, further research into long term results was deemed necessary. Then, we performed this study.
First of all, we cannot help talking about the follow-up loss. This is the most critical weakness of this study. We lost 10 patients' follow-up (32.3%) in 3 months and 6 more (19.4%) additionally in next 9 months. The most common reason why the patients did not follow-up, is remission or improvement which let them need no follow-up, although we checked it up juts via a phone call. The second most reason was too far from home to our clinic. Whatever the reason, too many follow-up losses is the fatal weakness of this study and which can be regarded as a defect to be published. But, this is the first study to perform DJB on Asian low BMI patients with T2DM and relatively long term follow-up. Although the follow-up loss makes assessment and interpretation of the results difficult, this study would deserve in offering some pieces of information as follows; 1) DJB can induce remission which cannot get by conventional medical treatment; 2) DJB or bypass of foregut would make beta cell function improve; 3) The remission rate was lower than expected.
The treatment goals for those with T2DM are the maintenance of blood sugar levels through exercise, dieting, OHA and supplemental insulin, etc., as well as prevention of complications. However, the secretory function of beta-cells in T2DM decreases with time, and the nature of the condition becomes more like that of type 1 diabetes. Then its management becomes difficult and the effect of OHAs decrease [10].
All patients of this study had had some medications for T2DM, but 33.3% of patients could quit the medications after DJB.
In 1995, Pories et al. [11] reported that out of 146 T2DM patients and 152 patients with a disturbed glucose tolerance who underwent Roux en Y gastric bypass (RYGBP) for reducing body weight, 83% and 99% respectively were able to maintain complete remission in the 14 years of observation follow-up, and suggested that obesity surgery could be performed on purpose of treating T2DM.
In the process of observing the effects of RYGBP, improvements of T2DM were seen within days, even before significant weight loss occurred. Meanwhile, the improvement of T2DM after gastric banding (GB) was observed in proportion to weight loss, with time. Furthermore, the disease in patients of RYGBP showed significant improvement comparative to patients of GB. That suggests bypassing of foregut have some role in control of T2DM. Several researchers came to make the assertion that it could be used as a surgical treatment also in nonobese patients as well as obese patients so as to improve the diabetic condition [3,11-16].
Following this, the researchers presented results showing that T2DM was improved while almost no weight loss occurred when DJB was performed [17,18].
The hypotheses supporting these results are the involvement that the entero-insular axis and changes in the secretion of incretin induce the improvement of the control of blood sugar levels [3,18,19]. Entero-insular axis refers to the effect of hormones secreted from the small intestine on pancreas beta-cells, whereas incretin, a hormone group secreted from the small intestine, plays the role for the secretion of insulin. Foods and liquids do not pass through the duodenum and upper part of the small intestine after RYGBP. When bypassing down the jejunum or ileum, the secretion of incretin increases from the early stages (hindgut hypothesis) or insulin resistance decreases due to change of gastrointestinal hormone milieu (foregut hypothesis) [20,21]. Additionally, some researchers reported that these changes may induce the improvement of beta cell function [10,18-21].
Currently, it remains in dispute what is the main contributor to control glycemia after metabolic surgery: 1) reduced insulin resistance or 2) increased beta cell function. Advocates for metabolic surgery insist that metabolic surgery can exert effect on both. Opponents suspect that metabolic surgery can reduce insulin resistance and which can be accomplished by weight reduction. This study shows that DJB reduces insulin resistance, which can be explained by abrupt decrease of glucose and insulin level a week after operation. And also, DJB improve beta cell function, which can be explained by increase of insulin and decrease of glucose at 3, 12 months.
We can see the evidence of improvement of beta cell function in other aspects. The curves of glucose and insulin level in 75-g OGTT were transformed into parabolic pattern, i.e., preoperative curves presented the level of both were getting higher while reaching 120 minutes. But, after surgery, the curves had a peak at 60 minutes. although the peak of normal persons can be seen at 30 minutes. Those would be the evidences of beta cell improvement.
Moreover, all patients, even if nonresponder, showed improved glucose and insulin level at 12 months. That means DJB has an effect on improvement of T2DM and improvement or remission depend on the degree of effect.
We wanted to have a chance to find some parameters to predict the improvement or remission but the number of enrolled patients and remission were too small to evaluate. Then we presented just the data of change of clinical parameters for other studies.
As for complications, foregut bypass is considered as a ulcerogenic procedure, for the acidity of duodenum is always alkali, while other complications were minor and expectable (1 urinary infection and 1 stitch abscess). Two-month prescription of PPI after surgery is a routine in bariatric surgery, especially RYGBP. After this routine prescription, there was no patient undergone marginal ulcer. Although, the reposts for marginal ulcer after DJB are rare, this procedure is thought to be vulnerable to marginal ulcer. DJB has been thought as an experimental operation, which had not been fully estimated in the aspect of physiology. Additionally, many reports presented the remission rate about 10% [22] whereas the GBP showing that over 70% [23] as well as well-established physiology. Then, many metabolic surgeons including us, insist that new metabolic procedure including GBP should be studied.
In conclusion, this study observed the changes in glucose and insulin levels with 75-g OGTT till one year after DJB in patients of T2DM with a BMI of <25 kg/m2. This is the first study in Korea on the surgical approach of diabetes patients in the healthy weight range. About 10% of patients showed diabetic remission and about 30% showed improvement. DJB exerted positive influences on insulin resistance as well as beta cell function. Although early effects on T2DM after DJB could be estimated as one of good modalities, the effectiveness seems to be unacceptable comparing with other metabolic procedures. Further studied are mandatory for evaluation of metabolic surgery and finding prognostic factors for remission of T2DM.
Figures and Tables
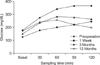 | Fig. 1Comparison of 75-g oral glucose tolerance test between preoperation, postoperation, 3 months, and 12 months. Glucose levels compared with those of preoperative: all level are P < 0.05, except 30 minutes at 3 months and basal at 12 months. |
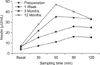 | Fig. 2Comparison of Insulin level between preoperation, postoperation, 3 months, and 12 months. Insulin levels compared with those of preoperative: P < 0.05 in all of 1 week, 60 minutes at 3 months and 12 months. |
References
1. Inzucchi SE. Oral antihyperglycemic therapy for type 2 diabetes: scientific review. JAMA. 2002; 287:360–372.
2. Sjostrom L, Lindroos AK, Peltonen M, Torgerson J, Bouchard C, Carlsson B, et al. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med. 2004; 351:2683–2693.
3. Rubino F, Forgione A, Cummings DE, Vix M, Gnuli D, Mingrone G, et al. The mechanism of diabetes control after gastrointestinal bypass surgery reveals a role of the proximal small intestine in the pathophysiology of type 2 diabetes. Ann Surg. 2006; 244:741–749.
4. Salinari S, Bertuzzi A, Asnaghi S, Guidone C, Manco M, Mingrone G. First-phase insulin secretion restoration and differential response to glucose load depending on the route of administration in type 2 diabetic subjects after bariatric surgery. Diabetes Care. 2009; 32:375–380.
5. Guidone C, Manco M, Valera-Mora E, Iaconelli A, Gniuli D, Mari A, et al. Mechanisms of recovery from type 2 diabetes after malabsorptive bariatric surgery. Diabetes. 2006; 55:2025–2031.
6. Laferrere B, Teixeira J, McGinty J, Tran H, Egger JR, Colarusso A, et al. Effect of weight loss by gastric bypass surgery versus hypocaloric diet on glucose and incretin levels in patients with type 2 diabetes. J Clin Endocrinol Metab. 2008; 93:2479–2485.
7. Pories WJ, Caro JF, Flickinger EG, Meelheim HD, Swanson MS. The control of diabetes mellitus (NIDDM) in the morbidly obese with the Greenville Gastric Bypass. Ann Surg. 1987; 206:316–323.
8. Kang KC, Shin SH, Lee YJ, Heo YS. Influence of gastrectomy for stomach cancer on type 2 diabetes mellitus for patients with a body mass index less than 30 kg/m2. J Korean Surg Soc. 2012; 82:347–355.
9. Hong IK, Kim JY, Lee YJ, Choe YM, Choi SK, Heo YS, et al. The effect of duodenojejunal bypass for T2DM patients below BMI 25 kg/m2 in early postoperative period. J Korean Surg Soc. 2011; 80:103–110.
10. Prentki M, Nolan CJ. Islet beta cell failure in type 2 diabetes. J Clin Invest. 2006; 116:1802–1812.
11. Pories WJ, Swanson MS, MacDonald KG, Long SB, Morris PG, Brown BM, et al. Who would have thought it? An operation proves to be the most effective therapy for adult-onset diabetes mellitus. Ann Surg. 1995; 222:339–350.
12. Pories WJ, MacDonald KG Jr, Flickinger EG, Dohm GL, Sinha MK, Barakat HA, et al. Is type II diabetes mellitus (NIDDM) a surgical disease? Ann Surg. 1992; 215:633–642.
13. Lee WJ, Huang MT, Wang W, Lin CM, Chen TC, Lai IR. Effects of obesity surgery on the metabolic syndrome. Arch Surg. 2004; 139:1088–1092.
14. Madan AK, Orth W, Ternovits CA, Tichansky DS. Metabolic syndrome: yet another co-morbidity gastric bypass helps cure. Surg Obes Relat Dis. 2006; 2:48–51.
15. Mottin CC, Vontobel Padoin A, Schroer CE, Barancelli FT, Glock L, Repetto G. Behavior of type 2 diabetes mellitus in morbid obese patients submitted to gastric bypass. Obes Surg. 2008; 18:179–181.
16. Rubino F, Marescaux J. Effect of duodenal-jejunal exclusion in a non-obese animal model of type 2 diabetes: a new perspective for an old disease. Ann Surg. 2004; 239:1–11.
17. Cohen R, Pinheiro JS, Correa JL, Schiavon CA. Laparoscopic Roux-en-Y gastric bypass for BMI < 35 kg/m(2): a tailored approach. Surg Obes Relat Dis. 2006; 2:401–404.
18. Patriti A, Facchiano E, Sanna A, Gulla N, Donini A. The enteroinsular axis and the recovery from type 2 diabetes after bariatric surgery. Obes Surg. 2004; 14:840–848.
19. Gutniak M, Orskov C, Holst JJ, Ahren B, Efendic S. Antidiabetogenic effect of glucagon-like peptide-1 (7-36) amide in normal subjects and patients with diabetes mellitus. N Engl J Med. 1992; 326:1316–1322.
20. Drucker DJ. Biological actions and therapeutic potential of the glucagon-like peptides. Gastroenterology. 2002; 122:531–544.
21. Gautier JF, Fetita S, Sobngwi E, Salaun-Martin C. Biological actions of the incretins GIP and GLP-1 and therapeutic perspectives in patients with type 2 diabetes. Diabetes Metab. 2005; 31(3 Pt 1):233–242.
22. Geloneze B, Geloneze SR, Chaim E, Hirsch FF, Felici AC, Lambert G, et al. Metabolic surgery for non-obese type 2 diabetes: incretins, adipocytokines, and insulin secretion/resistance changes in a 1-year interventional clinical controlled study. Ann Surg. 2012; 256:72–78.
23. Garcia-Caballero M, Valle M, Martinez-Moreno JM, Miralles F, Toval JA, Mata JM, et al. Resolution of diabetes mellitus and metabolic syndrome in normal weight 24-29 BMI patients with One Anastomosis Gastric Bypass. Nutr Hosp. 2012; 27:623–631.




 ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download