Abstract
Symptomatic gastrointestinal metastasis from lung malignancy is rarely reported. In this report, we present a case of lung adenocarcinoma with acute abdominal pain from small bowel perforation. The patient underwent small bowel resection and the final diagnosis was metastatic adenocarcinoma originating from lung. Immunohistochemistry was positive for thyroid transcription factor-1 and cytokeratin 7 (CK7), and negative for CK20. We present this rare case and briefly review the literature.
In Korea, primary lung cancer is the third most common malignancy in incidence and is more common in people over 65 years old. Approximately 50% of patients have metastases at the time of diagnosis. Frequently involved extrapulmonary metastatic sites of lung cancer are lymph nodes, liver, brain, adrenal glands, and bones, but metastasis to the gastrointestinal track is rarely reported, ranging from 0.2% to 1.7% in reported studies [1,2]. However, it is very difficult to detect gastrointestinal metastasis without symptoms [2,3] and autopsy reports state the prevalence of gastrointestinal (GI) metastasis of lung cancer is 4.7% to 14% [4], much higher than expected.
We report a case of metastatic adenocarcinoma of the lung with accompanying small bowel perforation. Also, we reviewed the literature relevant to the occurrence, diagnosis and outcome of GI metastasis of lung cancer.
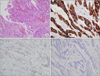
A 79-year-old male was admitted to the emergency department with complaints of abdominal pain starting a day prior. Six months earlier, he was diagnosed with lung cancer and liver metastasis (Fig. 1A, B). Chest computed tomography (CT) showed a 2.0 × 1.6 cm sized spiculated mass in the posterior segment of the right upper lobe with an adjacent 1 cm sized metastatic mass. Liver magnetic resonance imaging showed a 1 cm sized nodule in S2 of the liver. The histologic subtype of the lung cancer was poorly differentiated adenocarcinoma. After diagnosis, he refused chemotherapy and only took medicine to control his cough and sputum. According to operation history, he underwent antrectomy with gastrojejunal anastomosis due to gastric ulcer perforation, over 20 years ago. As soon as he arrived at emergency room, we checked the abdominal CT and it showed pneumoperitoneum and aggravation of hepatic metastasis (Fig. 2A, B). Considering disease status and physical status we decided to do an emergency laparotomy. We initially thought the perforation focus was the stomach, but it was a distal ileum located 100 cm proximal from the ileocecal valve. In the abdominal cavity, there was a 1 cm sized free perforation in the ileum, and edematous change of the small bowel with no evidence of peritoneal seeding. We resected about 10 cm length distal ileum and conducted ileoileal end-to-end hand-sewn anastomosis. Postoperative pathological results showed metastatic adenocarcinoma originating from lung cancer. Immunohistochemical (IHC) staining revealed that the tumor cells were positive for cytokeratin 7 (CK7) and thyroid transcription factor (TTF) but negative for CK20 (Fig. 3A-D).
Postoperatively, the patient was treated in the intensive care unit for pulmonary care with a ventilator, and there was no sign of anastomosis leakage. Five weeks later, he was discharged from the hospital in healthy condition, contrary to our expectations.
Symptomatic small bowel metastases from lung cancer have been rarely reported. Berger et al. [5] reported 6 patients among 1,399 (0.5%) consecutively operated on for lung cancer developing clinically apparent small bowel metastasis.
Over 80% of the cases with small bowel metastasis were male, with ages ranging from 36 to 78 years old; and metastasis presented as perforation (59%), obstruction (29%) and hemorrhage (10%) [6].
Small bowel metastasis may occur in every cell type of primary lung cancer. Nevertheless, Antler et al. [7] reported that squamous cell and undifferentiated large cell carcinoma lead to gastrointestinal tract metastasis more often than other histological types. In contrast, in the series by McNeil et al. [8] and Yoshimoto et al. [1], large cell carcinoma was the more frequent histological type.
On the basis of the findings of 1,775 patient autopsies, Antler et al. [7] reported that metastasis to the digestive system from primary lung cancer occurs at a rate of 47% in the esophagus, 9% in the stomach, 19% in the small intestine, and 5% in the colon.
The confirmational diagnosis of small bowel metastasis from lung cancer is pathologic analysis, with IHC staining of TTF-1 (+), CK7 (+), CK20 (-) and CDX2 (-). Usually CK7 is expressed not in gastrointestinal tract malignancy but in lung and breast malignancy. CK20 is expressed in GI epithelium and urinary epithelium, besides TTF-1 is only expressed in lung and thyroid malignancies [2]. All adenocarcinomas, except lung adenocarcinoma, lack expression of TTF-1; so, TTF-1 is an important marker to differentiate primary adenocarcinoma from metastatic adenocarcinoma.
Symptomatic small bowel metastasis may require a surgical approach. The procedure of choice is generally resection of the involved small intestine with primary enterostomy [6]. However, the prognosis is considered to be very poor and reported perioperative mortality varies from 60% to 100% [8]. The average survival duration is under 16 weeks [9].
In summary, clinically apparent gastrointestinal metastasis is unusual, although the actual prevalence appears to be higher based on autopsy results. Physicians should be aware of this rare evolution and surgical treatment is usually required in patients with small bowel metastasis leading to perforation, obstruction and hemorrhage. In selected patients relatively long-term survival could be expected through aggressive treatment with surgery of both primary and metastatic tumors.
Figures and Tables
Fig. 1
(A) Chest computed tomography scan shows high density mass in right upper lobe. (B) Liver magnetic resonance imaging scan shows 1 cm sized nodule in segment 2.
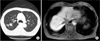
Fig. 2
Abdomen computed tomography scans show liver metastasis with pneumoperitoneum (A) and small bowel edematous change with fluid collection in distal ileum (B).
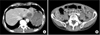
Fig. 3
Microscopic findings of small bowel. (A) The small bowel mucosa shows infiltration of tumor cells (H&E, ×100). (B) The malignant cells show positive stain for cytokeratin 7 (CK7), suggesting not primary colon origin (immunohistochemical [IHC] stain, ×100). (C) Negative satin for thyroid transcription factor-1, suggesting lung cancer origin (IHC stain, ×100). (D) Negative stain for CK20 (IHC stain, ×100).
References
1. Yoshimoto A, Kasahara K, Kawashima A. Gastrointestinal metastases from primary lung cancer. Eur J Cancer. 2006. 42:3157–3160.
2. Rossi G, Marchioni A, Romagnani E, Bertolini F, Longo L, Cavazza A, et al. Primary lung cancer presenting with gastrointestinal tract involvement: clinicopathologic and immunohistochemical features in a series of 18 consecutive cases. J Thorac Oncol. 2007. 2:115–120.
3. Yamamoto M, Matsuzaki K, Kusumoto H, Uchida H, Mine H, Kabashima A, et al. Gastric metastasis from lung carcinoma: case report. Hepatogastroenterology. 2002. 49:363–365.
4. Lermite E, Pessaux P, Du Plessis R, Brehant O, Hennekinne-Mucci S, Michalak-Provost S, et al. Small bowel metastasis from primary lung carcinoma. Gastroenterol Clin Biol. 2004. 28:307–309.
5. Berger A, Cellier C, Daniel C, Kron C, Riquet M, Barbier JP, et al. Small bowel metastases from primary carcinoma of the lung: clinical findings and outcome. Am J Gastroenterol. 1999. 94:1884–1887.
6. Hillenbrand A, Strater J, Henne-Bruns D. Frequency, symptoms and outcome of intestinal metastases of bronchopulmonary cancer: case report and review of the literature. Int Semin Surg Oncol. 2005. 2:13.
7. Antler AS, Ough Y, Pitchumoni CS, Davidian M, Thelmo W. Gastrointestinal metastases from malignant tumors of the lung. Cancer. 1982. 49:170–172.
8. McNeill PM, Wagman LD, Neifeld JP. Small bowel metastases from primary carcinoma of the lung. Cancer. 1987. 59:1486–1489.
9. Rouhanimanesh Y, Vanderstighelen Y, Vanderputte S, Cools P, Wassenaar H, Vallaeys J. Intra-abdominal metastases from primary carcinoma of the lung. Acta Chir Belg. 2001. 101:300–303.




 ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download