Abstract
Purpose
Laparoscopic techniques have gained wide clinical acceptance in surgical practice today. The laparoscopic approach has been established as the technique of choice for elective splenectomies performed on normal sized spleens. The purpose of this study was to evaluate the outcome of patients undergoing laparoscopic splenectomy (LS) at the TOBB University of Economics and Technology (ETU) Hospital and Kecioren Training and Research Hospital.
Methods
One hundred and thirty-five patients underwent splenectomy between January 2000 and July 2010. For comparison, the records of 130 patients undergoing splenectomy were evaluated for age, gender, hospital stay, time to start of diet, conversion rate, operation time and wound infection.
Results
Mean operation time means the time interval between surgeon commencing operation to end of operation. Mean operation time in patients treated by LS was 132 minutes and 121 minutes in open splenectomy (OS). Mean hospital stay was 5.65 days in patients undergoing LS and starting of diet was 1.21 days. In patients treated by OS, mean hospital stay was 9.17 days, starting of diet was 2.37 days. Four patients were converted to open surgery. Conversion rate was 6.4 percent. In the early post operative period (within 10 days of surgery) 9.2%, LS group had lower incidences of wound infection rate after surgery than OS group (4.8%, 7.4%, respectively; P = 0.06).
Laparoscopic techniques have gained wide acceptance with growing surgical experience and technological development. Laparoscopy has also been applied to other abdominal operations including Fundoplication, cholecystectomy, totally extraperitoneal/transabdominal preperitoneal, and appendectomy [1]. Laparoscopic splenectomy (LS) is an advanced minimally invasive procedure and first reported in 1991 [2,3].
Several factors make LS more difficult than other advanced laparoscopic procedures. Exposure of the spleen on the left upper quadrant can be difficult, especially in obese patients, and control of the splenic blood supply demands advanced technical skills and equipment. Injury to the tail of the pancreas during dissection of the splenic hilum may cause pancreatitis and pancreatic fistula.
LS has several advantages over open splenectomy (OS), despite these risks [4]. There are several prospective nonrandomized studies comparing OS and LS in the literature. LS results in less pain, shorter hospital stay, less morbidity and mortality, earlier return to job, and earlier start to diet [1,5-7].
Indications for LS are similar to those for open procedure with only a few exceptions. LS is especially used in hematologic diseases like idiopathic thrombocytopenic purpura (ITP). These patients generally use corticosteroids predisposing patients to wound infection and dehiscence [1,8]. Because of this, LS is the gold standard for splenectomy for normal-sized spleens. The aim of this study was to share our experience and encourage the usage of LS in our country.
One hundred and thirty-five patients underwent splenectomy at General Surgery Clinic between January 2000 and July 2010. Splenectomies for trauma and carcinoma were not included in the study. Precise contraindications for the laparoscopic approach were no different from other laparoscopic procedures and included portal hypertension and severe cardiopulmonary disease. No patients were pregnant. Computed tomography scans demonstrated splenic masses in all the patients. Ultrasonography was performed in patients with heterotopic splenosis to identify cholelithiasis. For comparison, the records of 130 patients undergoing splenectomy were evaluated for age, gender, hospital stay, time to start of diet, operation time, and wound infection rate.
Patients received pneumococcal and hemophilus influenzae vaccine 1 day before surgery. Surgery was performed under general anesthesia and right lateral decubitus position. The surgeon stood on the patient's right side, with the first assistant on the patient's left side and the camera assistant to the surgeon's left. The open Hasson technique was used to enter the peritoneal cavity and place the first port (12 mm), about 4 to 7 cm below the costal margin along the midclavicular line. Two 5-mm ports were then inserted under direct vision below the left subcostal margin. One was placed in the subxiphoid area and the other along the anterior axillary line. A 10-mm 30° laparoscope was used for visualization. Dissection was performed using a Harmonic Scalpel (Ethicon Endo-Surgery Inc., Cincinnati, OH, USA).
The abdomen is thoroughly inspected for accessory splenic tissue and additional pathologies. After extraction of liver and stomach, dissection is started. Gastrosplenic ligament was controlled with clips or endoscopic vascular stapler in our first experiences. The lateral peritoneal attachments of the spleen are divided with laparoscopic shear. The splenic hilar vessels were divided using the vascular endostapler ATW45 (Ethicon Endo-Surgery Inc.) introduced through the 12-mm port. The spleen is extracted by morcellation within a plastic bag and pulled out through the umbilical incision. The umbilical (usually 5 to 6 cm) incision was enlarged to allow for the removal of the bag without the risk of tearing. The fascia of umbilical incision is sutured.
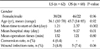
Of the 130 patients, 62 patients (47.7%) were operated on using the laparoscopic procedure. Of these, 38 were female and 26 were male. Age ranged between 10 and 70 years. Mean age was 36.1 years. Of the 68 patients (53.3%) undergoing OS, 46 (67.7%) were female and 22 (32.3%) were male. Mean age was 45.7 years and ranged between 14 and 85 years. All patients were readmitted for follow up 1 month later (Table 1).
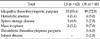
The indications for splenectomies were ITP in 53 patients (85.4%), spleen storage disease in 3 patients (4.8%), mass in spleen in 2 patients (3.2%) and hemolytic anemia in 4 patients (6.4%). OS was performed in 66 patients. Forty-nine patients (72%) had ITP, 4 patients (5%) had hemolytic anemia, 5 patients (7%) had spleen storage disease, 5 patients (7%) had mass in the spleen, 3 patients (4%) had TTP and infarct with abscess formation in 2 patients (2%) (Table 2). LS was successfully performed in 58 patients (93.5%). Four patients were converted to open surgery. The reason for conversion was bleeding in 2 patients and advanced adhesions in 2 patients. The conversion rate was 6.4 percent. Four patients were found to have accessory spleens and these were extracted. In early postoperative period, pancreatic fistula developed in one patient and percutaneously drained. In OS group, 1 patient was reoperated due to postoperative bleeding, left lung lobe basal atelectasis developed in 3 patients and deep venous thrombosis developed in 1 patient. All patients benefited from the medical treatment they had received. Mean hospital stay was 5.65 days in patients undergoing LS and starting of diet was 1.21 days. In patients treated by OS, mean hospital stay was 9.17 days, starting of diet was 2.37 days. There were statistically significant differences in terms of mean hospital stay and mean time of starting diet in the two groups, favouring LS (P = 0.01, P = 0.002, respectively) (Table 1).
Mean operation time means the time interval between surgeon commencing operation to end of operation. Mean operation time in patients treated by LS was 132 minutes and 121 minutes in OS. This difference was not statistically significant (Table 1).
In the early post operative period (within 10 days of surgery) incidences of wound infection rate after surgery 12.1%, LS group had lower incidences of wound infection rate after surgery than the OS group (4.8%, 7.4%, respectively; P = 0.06).
LS is indicated especially for elective splenectomies performed on normal-sized spleens. There are only limited prospective randomized studies comparing OS and LS, although there are several nonrandomized studies.
LS results in shorter hospital stay, less perioperative morbidity, less postoperative pain, better cosmesis and shorter time to start of diet compared to OS. In our study, we compared operation time, hospital stay, conversion rate, start to diet between OS and LS [9]. Nowadays, splenectomy is indicated in cases with hematologic diseases that are unresponsive to medical therapy and have recurrence after medical therapy. When this operation has been performed laparoscopically, it results in the advantages mentioned above. The application of LS has become the standard technique, especially in hematologic diseases.
LS is especially used in patients with hemotologic diseases including ITP, hemolytic anemia and hemoglobinopathies. In our study, 58 patients operated for ITP, 4 for hemolytic anemia, 3 for spleen storage disease, and 2 for mass in spleen. Operation was completed laparoscopically in 93.5 percent and converted to open surgery in 6.4 percent of patients.
In several studies comparing LS and OS, LS has several advantages over OS [1,2,6,8,10,11]. LS is the standard splenectomy method for normal-sized spleen in large centers [1-4,5,6]. There are 3 controversial issues in LS for enlarged spleen. First is feasibility in enlarged spleen, second is detection of accessory spleen, and the third is long-term follow up results.
LS was started in our clinic since 1994 as in developed countries. Operation time was longer and mean time was 150 minutes in our early experiences. Operation time has been shortened and the mean time has dropped down to 60 to 80 minutes as experience with LS has been gained. However, 62 of 130 splenectomies were started laparoscopically, when we looked at our splenectomy series in the last five years.
Splenomegaly is a contraindication for LS in our center like in most centers. This is due to difficulties in controlling of spleen and technical insufficiency [10,12]. Because of this, the number of OS was higher than LS in the last 5 years. But LS is being performed more frequently with growing experiences and technical improvements. With the technological development and increase in our experience, we have performed LS in patients with splenomegalies. But in this study, we did not compare the size of the spleens in the two groups. Operation time is longer in enlarged spleen compared to normal-sized spleen [8]. In our study, mean operation time was 132 minutes in LS and 121 minutes in OS.
Accessory spleen is another subject of debate in LS. Although accessory spleens are found in 10% of the general population, they are more common (30%) in patients with hematologic disease [13]. Donini et al. [14] reported that there was no significant difference in detecting accessory spleens between LS and OS. It is easier to detect accessory spleens in LS due to the magnifying effect of laparoscopy. In some studies, accessory spleens were detected in 11 to 21% of patients undergoing LS and in 4 to 27% of patients undergoing OS with the same indications [15]. In our study, accessory spleens were found in 4 patients (6.6%) and were extracted laparoscopically.
In long-term follow-up of patients, remission rates of 80 to 90% were reported in LS. There were similar results in OS patients [16]. In our study, recurrence was detected in 7 patients (8.8%) in short-term follow-up. Recurrence was because of accessory spleen. Most of the patients that need splenectomy were those that had hematologic diseases and cardiovascular diseases. Minimally invasive procedures are more advantageous to these patients [17].
Hospital stay and time at which oral intake was started were shorter in LS group. Also liquid diets may be given to patients in the morning of operation day [18]. In order to reduce post operative nausea we had given the patients 400 mL of carbohydrate solution 90 minutes before the operation morning. In our study, mean hospital stay was 5.65 days and start time to diet 1.21 days in LS patients. These data were 9.17 and 2.37 days in OS patients, respectively. The differences between LS and OS were statistically significant in favour of LS.
In conclusion, LS is a safe and effective procedure in experienced hands. LS is superior with regard to hospital stay, start time to diet, wound infection and cosmesis. Finding of accessory spleen that creates difficulty in LS is not different from OS in long-term follow-up studies. Enlarged spleen is not a contraindication in selected cases nowadays. LS can be performed safely in appropriate cases.
Figures and Tables
References
1. Glasgow RE, Yee LF, Mulvihill SJ. Laparoscopic splenectomy. The emerging standard. Surg Endosc. 1997. 11:108–112.
2. Delaitre B, Maignien B. Splenectomy by the laparoscopic approach. Report of a case. Presse Med. 1991. 20:2263.
3. Hashizume M, Sugimachi K, Ueno K. Laparoscopic splenectomy with an ultrasonic dissector. N Engl J Med. 1992. 327:438.
4. Glasgow RE, Mulvihill SJ. Laparoscopic splenectomy. World J Surg. 1999. 23:384–388.
5. Tsiotos G, Schlinkert RT. Laparoscopic splenectomy for immune thrombocytopenic purpura. Arch Surg. 1997. 132:642–646.
6. Watson DI, Coventry BJ, Chin T, Gill PG, Malycha P. Laparoscopic versus open splenectomy for immune thrombocytopenic purpura. Surgery. 1997. 121:18–22.
7. Brunt LM, Langer JC, Quasebarth MA, Whitman ED. Comparative analysis of laparoscopic versus open splenectomy. Am J Surg. 1996. 172:596–599.
8. Delaitre B, Pitre J. Laparoscopic splenectomy versus open splenectomy: a comparative study. Hepatogastroenterology. 1997. 44:45–49.
9. Winslow ER, Brunt LM. Perioperative outcomes of laparoscopic versus open splenectomy: a meta-analysis with an emphasis on complications. Surgery. 2003. 134:647–653.
10. Diaz J, Eisenstat M, Chung R. A case-controlled study of laparoscopic splenectomy. Am J Surg. 1997. 173:348–350.
11. Smith CD, Meyer TA, Goretsky MJ, Hyams D, Luchette FA, Fegelman EJ, et al. Laparoscopic splenectomy by the lateral approach: a safe and effective alternative to open splenectomy for hematologic diseases. Surgery. 1996. 120:789–794.
12. Olsen WR, Beaudoin DE. Increased incidence of accessory spleens in hematologic disease. Arch Surg. 1969. 98:762–763.
13. Janu PG, Rogers DA, Lobe TE. A comparison of laparoscopic and traditional open splenectomy in childhood. J Pediatr Surg. 1996. 31:109–113.
14. Donini A, Baccarani U, Terrosu G, Corno V, Ermacora A, Pasqualucci A, et al. Laparoscopic vs open splenectomy in the management of hematologic diseases. Surg Endosc. 1999. 13:1220–1225.
15. Rudowski WJ. Accessory spleens: clinical significance with particular reference to the recurrence of idiopathic thrombocytopenic purpura. World J Surg. 1985. 9:422–430.
16. Katkhouda N, Hurwitz MB, Rivera RT, Chandra M, Waldrep DJ, Gugenheim J, et al. Laparoscopic splenectomy: outcome and efficacy in 103 consecutive patients. Ann Surg. 1998. 228:568–578.
17. Akwari OE, Itani KM, Coleman RE, Rosse WF. Splenectomy for primary and recurrent immune thrombocytopenic purpura (ITP): current criteria for patient selection and results. Ann Surg. 1987. 206:529–541.
18. Mintz SJ, Petersen SR, Cheson B, Cordell LJ, Richards RC. Splenectomy for immune thrombocytopenic purpura. Arch Surg. 1981. 116:645–650.




 ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download