Abstract
Meckel's diverticulum (MD) is a true congenital diverticulum that is remnant by incomplete obliteration of the omphalomesenteric duct. It is the most common congenital anomaly of the gastrointestinal tract, with an estimated prevalence of 2% (0.3% to 3% in autopsy studies). About 90% of MD occurs within 100 cm of the ileocecal valve. A primary malignant tumor arising within an MD is extremely uncommon. Malignancies are reported to account for only 0.5% to 3.2% of the complications. Carcinoids are the most common malignant tumors occurring in MD. Adenocarcinomas are extremely uncommon and very poor prognosis has been reported. We report a case of radiographically diagnosed chronic inflammatory mass caused by adenocarcinoma arising from MD in the ileum with malrotation of the midgut incidentally discovered at exploration.
Meckel's diverticulum (MD) is remnant by incomplete obliteration of the vitelline or omphalomesenteric duct around the seventh or eighth week of gestation [1-3]. It is a true diverticulum that usually arises from the antimesenteric border of the distal part of ileum and contains all layers of the normal intestinal wall. It is the most common congenital anomaly of the Gastrointestinal tract, with an estimated prevalence of 2% (0.14% to 4.5% in autopsy studies) [3]. About 90% of MDs occur within 60 to 100 cm of the ileocecal valve (ICV) and mean distance from the ICV varies with age and measures about 3 cm in length [4-6]. A primary malignant tumor arising within an MD is extremely uncommon. Malignancies are reported to account for only 0.5% to 3.2% of the complications [1,6,7]. Carcinoids are the most common malignant tumors occurring in MD [8]. Adenocarcinomas are extremely uncommon and very poor prognosis has been reported [9]. We report a case of radiographically diagnosed chronic inflammatory mass caused by adenocarcinoma arising from MD in the ileum.
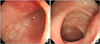
A 19-year-old woman received an examination from the department of gynecology with complaints of pain in the left lower abdomen. Laboratory test results included the following: carbohydrate antigen (CA) 125, 38.75 U/mL (normal, 0 to 35.0 U/mL); CA 19-9, 2,038.0 U/mL (normal, 0 to 36.10 U/mL). Serum electrolytes, tests of liver and renal function were within normal ranges. A sonography by the gynecologist revealed a right ovarian cyst (8.2 cm × 7.4 cm) but computed tomography (CT) revealed a chronic inflammatory mass (abscess from unknown etiology, 6.7 cm × 6.4 cm × 6.3 cm) with severe inflammatory infiltrations into adjacent mesentery, sigmoid colon and small bowel loops and magnetic resonance imaging indicated the same findings (Fig. 1). Positron emission tomography (PET)-CT revealed a malignant tumor in the pelvic cavity abutting the small bowel and rectum (Fig. 2). Colonoscopy revealed erythematous masses like external indentations on the distal descending colon (50 cm from anal verge) and sigmoid colon (15 cm from anal verge) (Fig. 3).
She underwent laparoscopic exploration. During operation, a 6 cm-sized mass in the antimesenteric border of the ileum was noted, approximately 40 cm proximal from the ICV. Adult malrotation of the midgut was found incidentally at exploration. She underwent laparoscopic Ladd procedure and segmental resection of the ileum (Fig. 4). Intraoperative frozen biopsy was performed and the temporary pathologic report showed metastatic adenocarcinoma, probably originating from the colon or endometrium. Intraoperative endometrial biopsy was performed by the gynecologist and a frozen biopsy showed no tumor on endometrium. The final pathological diagnosis was adenocarcinoma, moderately differentiated (6.0 cm × 4.0 cm) from MD with serosa invasion and one regional lymph node metastasis (T4N1M0, stage IIIA according to the 7th American Joint Committee on Cancer classification). She was discharged uneventfully on post-operative day 6.
In 1598, Wilhelm Fabricius Hildanus, a German surgeon, first described the presence of a diverticulum of the small bowel occurring in the distal part of the ileum, which later came to be called by the last name of the German anatomist, Johann Friedrich Meckel who first described its embryological origin in 1809 [3,4].
The total lifetime risk of complication in patients with a Meckel's diverticulum is not greater than 4% [7] with a high male predominance (male-to-female ratio ranging from 1.8:1 to 3:1) [2,5].
Acute or intermittent intestinal obstruction is the most common complication in adult patients and incidence rates of obstruction varied from 22% to 50% [5,6,10]. It usually results from intussusception, invagination, volvulus, or internal hernia [5,6]. It may be caused by neoplasm, less frequently.
Neoplasms arising from Meckel's diverticulum are uncommon and quoted to be 0.5% to 3.2% [5,8] with carcinoids as the most common malignant tumors occurring in this site. Other reported cases include sarcomas, adenocarcinomas, benign mesenchymal tumors, melanoma, and lymphoma [4].
Adenocarcinomas are extremely rare. A Pubmed search was performed for all articles with the following words in the title, abstract, or keywords: "Meckel's diverticulum", "adenocarcinoma". Since 1992, 30 people with adenocarcinoma were reported with nine people having been additionally reported so far. In the Surveillance, Epidemiology and End Results (SEER) program in the United States from 1973 to 2006, 18 people have been reported. It may arise mainly from heterotopic tissue within the diverticulum, including pancreatic tissue, duodenal, jejunal, colonic and gastric mucosa. In the few cases described so far, prognosis has been reported as very poor [9].
It is extremely difficult to diagnose, preoperatively, malignancies in a Meckel's diverticulum. The suspicion of its malignancies is often difficult at the initial stage of patient management. When malignancies are suspected or diagnosed as malignancies before surgery, it is more likely to be advanced stage [9].
There were some reports about the coincidence of Meckel's diverticulum with intestinal malrotation in children. Ford et al. [10] had reported the coincidence of Meckel's diverticulum up to 11% in children diagnosed with intestinal rotation. In adults, there are few reports about Meckel's diverticulum associated with intestinal malrotation; especially, no report associated with malignant tumor.
In our case, the patient had chronic inflammatory mass on the left lower abdomen that was suspected as a malignant tumor in the pelvic cavity by PET-CT. During operation, we found a 6 cm-sized Meckel's diverticulum in the antimesenteric border of the ileum with malrotation of the midgut incidentally at exploration. Final pathologic diagnosis was advanced stage of adenocarcinoma with lymphatic metastasis.
In conclusion, our case demonstrates that adenocarcinoma arising from Meckel's diverticulum is difficult to diagnose preoperatively and has poor prognosis. We accidentally found an intestinal malrotation in this case, first reported in the literature.
Figures and Tables
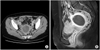 | Fig. 1Initial computed tomography (A, axial view) and magnetic resonance imaging (B, sagittal view) shows an approximately 6.7 cm × 6.4 cm × 6.3 cm sized chronic inflammatory mass with severe inflammatory infiltration into adjacent mesentery, sigmoid colon and small bowel loop. |
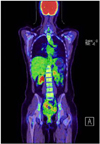 | Fig. 2Positron emission tomography-computed tomography shows malignant tumor in pelvic cavity abutting small bowel and rectum. |
ACKNOWLEDGEMENTS
This research was supported by Seoul St. Mary's Clinical Medicine Research Program year of 2011 through the Catholic University of Korea.
References
1. Dumper J, Mackenzie S, Mitchell P, Sutherland F, Quan ML, Mew D. Complications of Meckel's diverticula in adults. Can J Surg. 2006. 49:353–357.
2. Stone PA, Hofeldt MJ, Campbell JE, Vedula G, DeLuca JA, Flaherty SK. Meckel diverticulum: ten-year experience in adults. South Med J. 2004. 97:1038–1041.
3. Jay GD 3rd, Margulis RR, McGraw AB, Northrip RR. Meckel's diverticulum; a survey of one hundred and three cases. Arch Surg. 1950. 61:158–169.
4. Yahchouchy EK, Marano AF, Etienne JC, Fingerhut AL. Meckel's diverticulum. J Am Coll Surg. 2001. 192:658–662.
5. Mackey WC, Dineen P. A fifty year experience with Meckel's diverticulum. Surg Gynecol Obstet. 1983. 156:56–64.
6. Ymaguchi M, Takeuchi S, Awazu S. Meckel's diverticulum. Investigation of 600 patients in Japanese literature. Am J Surg. 1978. 136:247–249.
7. Turgeon DK, Barnett JL. Meckel's diverticulum. Am J Gastroenterol. 1990. 85:777–781.
8. Dixon AY, McAnaw M, McGregor DH, Keushkerian S, Miller LK, Pierce PD. Dual carcinoid tumors of Meckel's diverticulum presenting as metastasis in an inguinal hernia sac: case report with literature review. Am J Gastroenterol. 1988. 83:1283–1288.
9. Kusumoto H, Yoshida M, Takahashi I, Anai H, Maehara Y, Sugimachi K. Complications and diagnosis of Meckel's diverticulum in 776 patients. Am J Surg. 1992. 164:382–383.
10. Ford PV, Bartold SP, Fink-Bennet DM, Jolles PR, Lull RJ, Maurer AH, et al. Procedure guideline for gastrointestinal bleeding and Meckel's diverticulum scintigraphy. Society of Nuclear Medicine. J Nucl Med. 1999. 40:1226–1232.




 ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download