Abstract
Purpose
Diverticulitis of vermiform appendix is known as a rare cause of acute appendicitis, most of which are diagnosed after surgery. We compared appendiceal diverticulitis with acute appendicitis to study the clinical characteristics of appendiceal diverticulitis.
Methods
Among 1,029 patients who received appendectomy from January 2009 to May 2011, 38 patients with appendiceal diverticulitis (diverticulitis group) were compared with 98 randomly collected patients with acute appendicitis (appendicitis group) during the same period. Patients' characteristics, clinical features, laboratory findings, operative findings, and postoperative course were compared between the two groups.
Results
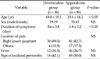
Thirty-eight patients (3.7%) were pathologically diagnosed with acute appendiceal diverticulitis among 1,029 cases of appendectomy. The mean age of patients in the diverticulitis group was significantly older than that of the appendicitis group (49.0 ± 15.2 years vs. 25.4 ± 14.2 years, P < 0.05). Mean duration of preoperative symptoms was longer in the diverticulitis group (3.6 ± 3.8 days vs. 1.8 ± 3.2 days, P < 0.05). The site of abdominal pain, fever, signs of localized peritonitis, accompanying gastrointestinal symptoms, and white blood cell count showed no differences between the two groups. Twenty-five patients (65.8%) of the diverticulitis group and 10 patients (10.2%) of the appendicitis group showed perforation of appendix (P < 0.05). Mean operating time and postoperative hospital stay were longer in the diverticulitis group (55.3 ± 28.8 minutes vs. 41.4 ± 17.8 minutes, 6.8 ± 3.4 days vs. 4.9 ± 1.5 days, P < 0.05).
Acute appendiceal diverticulitis is reported as a rare cause of appendicitis with a frequency of 0.004% to 2.1% [1]. It can be easily overlooked by surgeons and pathologists, with most of them are diagnosed after surgery.
Clinical features of appendiceal diverticulitis are similar to conventional acute appendicitis. However, it is known that patients with appendiceal diverticulitis are relatively older and risk of complications such as perforation is higher due to delay of diagnosis and the anatomical features of diverticulum. Therefore, diverticulitis of the appendix must be regarded as a different disease entity, features between two groups but clinical characteristics are still not well known and most studies are confined to case reports [2-4].
We compared appendiceal diverticulitis with acute appendicitis to study the clinical characteristics of diverticulitis of the appendix.
From Jan 2009 to May 2011, 1,029 patients received appendectomies with clinical suspicion of acute appendicitis in Eulji Medical Center. Thirty-eight patients were pathologically diagnosed with acute diverticulitis of the appendix after surgery (diverticulitis group). Ninety-eight patients who underwent appendectomy for acute appendicitis during the same period were enrolled in a control group (appendicitis group). The control group was collected among total cases of appendicitis using computerized simple random sampling to minimize selection bias. Patients of both groups underwent appendectomy only and drain tubes were inserted if necessary. Patients' characteristics, clinical features, laboratory findings, operative findings, and postoperative course were compared between the two groups by retrospective analysis of medical records.
For statistical processing, we used SPSS ver. 12.0 (SPSS Inc. Chicago, IL, USA) to perform simple random sampling of control group, Student's t-test and chi-square test. Statistical significance was determined when the P-value was lower than 0.05.
Thirty-eight patients (3.7%) were pathologically confirmed with acute diverticulitis of the appendix after surgery among 1,029 cases of appendectomy. There was no significant difference between the two groups in gender ratio (19 males in diverticulitis group and 55 males in appendicitis group). Mean age of patients was 49.0 ± 15.2 years in diverticulitis group and significantly older than 25.4 ± 14.2 years in appendicitis group (P < 0.05).
Mean duration of preoperative symptoms was 3.6 ± 3.8 days in diverticulitis group and 1.8 ± 3.2 days in appendicitis group (P < 0.05). Thirty-four patients (89.5%) of diverticulitis group and 81 patients (82.7%) of appendicitis group complained of right lower quadrant abdominal pain, showing no difference in location of pain; fever (higher than 37.5℃) was observed in 12 patients (31.6%) and 36 patients (36.7%), respectively. Signs of localized peritonitis such as tenderness, rebound tenderness and muscle guarding were found in 16 patients (42.1%) and 49 patients (50.0%), respectively, showing no statistical difference (Table 1).
Accompanying gastrointestinal symptoms were found in 22 patients (57.9%) of diverticulitis group including nausea (47.4%), vomiting (21.1%) and diarrhea (10.5%). Fifty-four patients (65.1%) of appendicitis group complained gastrointestinal symptoms such as nausea (33.7%), vomiting (25.5%) and diarrhea (17.3%), others (5.1%). The white blood cell (WBC) count at the time of admission was 13,038/mm3 in diverticulitis group and 13,272/mm3 in appendicitis group but showed no difference.
The rate of perforation of diverticulitis group was significantly higher than that of appendicitis group. Twenty-five patients (65.8%) of diverticulitis group and 10 patients (10.2%) of appendicitis group showed perforation of the appendix and formation of localized abscess during operation. Mean operating time was longer in diverticulitis group (55.3 ± 28.8 minutes vs. 41.4 ± 17.8 minutes, P < 0.05). Drain tube was inserted in 28 patients (73.7%) of diverticulitis group and in 19 patients (19.4%) of appendicitis group (P < 0.05).
Since first described by Kelynack in 1893 (quoted from [1]), acute diverticulitis of vermiform appendix has been overlooked by surgeons and pathologists because of its rare incidence and similar clinical features and mode of treatment with that of conventional acute appendicitis.
Although few studies reported that pathophysiology and clinical features of acute diverticulitis of appendix is different from appendicitis, most studies have been confined to case reports, and clinicopathologic characteristics are not well established.
The majority of appendiceal diverticulitis is acquired diverticulum with incidence is ranging between 0.004% and 2.1%. Congenital diverticulum is very rare and reported with an incidence of 0.014% [1]. Collins [5] reported an incidence of 1.4% with 50,000 autopsy and surgical specimen studies. In our study, an incidence of 3.7% was reported; relatively higher compared with previous reports.
Appendiceal diverticulitis is known to occur in older ages than acute appendicitis. Acute appendicitis most frequently occurs in one's twenties, whereas appendiceal diverticulitis is known to occur in the 5th decade of life. In our study, the mean age of patients in diverticulitis group was significantly older than that of appendicitis group (49.0 ± 15.2 vs. 25.4 ± 14.2, P < 0.05). Yamana et al. [6] reported a mean age of patients of 42.7 years in his study with most case studies [2-4,7,8] reporting patients older than 40 years. Consequently, aging might be a causative factor in the pathophysiology of appendiceal diverticulitis.
Duration of symptom of diverticulitis group was 3.6 days, which is longer than that of appendicitis group; and this result was similar with other studies. Lipton et al. [9] reported that older age (>30), longer interval of disease, fewer or absent symptoms of the gastrointestinal tract and failure of typical abdominal pain progression are the characteristics of appendiceal diverticulitis.
In Korea, Shin et al. [10] reported that appendiceal diverticula was diagnosed in patients who had complained of chronic right lower quadrant abdominal pain and showed improvement of symptoms after appendectomy. There was no significant difference in other clinical features such as accompanying gastrointestinal symptoms, fever, location of pain and WBC counts in this study.
Diverticulum of appendix can be divided into two histologic types, congenital and acquired diverticulum. Congenital type is true diverticulum consisting of all appendix layers (mucosa, submucosa, muscle layer and serosa), whereas acquired type is false diverticulum which lacks muscle layers.
Congenital diverticulum is recognized as a developmental abnormality. Its pathogenesis remains unclear but several mechanisms may be involved. Failure of recanalization of appendiceal lumen, duplication of appendix, failure of obliteration of vitelline duct or adhesion between the appendix and plica vascularis can be possible etiologies of congenital diverticulum. Favara [11] proposed that D13-15 trisomy symdrome can be involved with congenital appendiceal diverticular diseases.
The pathogenesis of acquired appendiceal diverticula may be related to inflammatory or noninflammatory theories. Inflammatory theory explains that previous recurrent inflammatory attacks or infections narrow the lumen and lead to atrophy of the lymphoid tissue (Fig. 2). This can make the appendiceal wall thinner and weaker causing diverticulum. Noninflammatory theory can be explained with the obstruction of the lumen and active muscular contraction. Luminal obstruction can be caused by inflammation, stricture, fecalith, mucosal fold, polyp and tumors (carcinoid, ademona, mucinous tumors and adenocarcinomas) [1].
Herniation of diverticulum is most likely to occur through the weak point of the appendiceal wall that can be caused by inflammation, atrophy of muscle by the aging process or vascular hiatus in the submucosa. The fact that most diverticula are located in mesenteric border supports the theory that vascular hiatus is closely related to the pathogenesis of diverticula [1,4].
Higher rate of perforation of appendiceal diverticulitis is most important compared with conventional appendicitis. A delay of diagnosis and absence of a thick muscle coat of the appendix are thought to be contributing factors. Our results showed that perforation of the appendix was found in 65.8% of diverticulitis group, which was more than six times higher than in appendicitis group. Therefore, we think that longer operation time, higher need for surgical drain, longer postoperative hospital stay were the result of the higher rate of perforation. Lipton et al. [9] reported that 66% patients with appendiceal diverticulitis showed perforation, which was a four-times higher perforation rate than appendicitis. Yamana et al. [6] reported a 33% perforation rate.
Diverticular diseases of the appendix can be divided into five microscopic types that can be defined as 1) primary acute diverticulitis, with or without acute peridiverticulitis, 2) acute diverticulitis secondary to acute appendicitis, 3) diverticulum without inflammation, 4) diverticulum with acute appendicitis, and 5) chronic peridiverticulitis with acute appendicitis [9,12].
Preoperative diagnosis of acute appendiceal diverticulitis is very difficult and most diagnoses are established by pathologic examination after surgery because the diverticulum is usually small, located in mesenteric border and has similar clinical features with acute appendicitis. Kubota et al. [13] reported the sonographic findings that the appendix wall layers are thickened and echogenic in appendiceal diverticulitis due to the presence of air. Osada et al. [14] reported that multi-detector computed tomography (MDCT) could find acute appendiceal diverticulitis in 6 of 7 case (86%) of pathologically confirmed appendiceal diverticulitis and insisted that MDCT has potential in the preoperative diagnosis of appendiceal diverticulitis.
Acute appendiceal diverticulitis can cause several complications such as intraperitoneal abscess, pelvic pseudocyst and vesicocecal fistula etc. In a domestic study, Choi et al. [15] reported hemorrhage from a diverticulum of the appendix and Lee et al. [16] reported intussusception combined with appendiceal diverticulosis. Also, appendiceal diverticulum accompanied with mucinous neoplasm of the appendix may play a possible role in the pathogenesis of pseudomyxoma peritonei [17].
Prompt surgical appendectomy is the treatment of choice for symptomatic acute appendiceal diverticulitis. Along with conventional appendectomy, recent laparoscopic procedure including single port surgery can be helpful. There is still controversy regarding incidentally discovered nonsymptomatic diverticulum during radiologic examinations or abdominal surgery. But, prophylactic, elective appendectomy is recommended because of the progression of 2/3 of appendiceal diverticulum into diverticulitis [8], high rates of perforation shown by previous studies and the possibility of coexisting appendiceal neoplasms.
In conclusion, acute diverticulitis of the appendix can be classified into quite different disease entities compared with conventional acute appendicitis. Patients with older age and longer duration of symptoms suspected of appendicitis should be given more attention and suspicion for appendiceal diverticulitis. Regarding high rates of perforation, immediate surgical treatment is needed for patients with a high index of suspicion of acute diverticulitis of the appendix.
Figures and Tables
Fig. 2
Herniated mucosa shows dense inflammatory cell infiltration with lymphoid aggregates (H&E, ×100).
References
1. Abdullgaffar B. Diverticulosis and diverticulitis of the appendix. Int J Surg Pathol. 2009. 17:231–237.
2. Heffernan DS, Saqib N, Terry M. A case of appendiceal diverticulitis, and a review of the literature. Ir J Med Sci. 2009. 178:519–521.
3. Kabiri H, Clarke LE, Tzarnas CD. Appendiceal diverticulitis. Am Surg. 2006. 72:221–223.
4. Simpson J, Lobo DN, Spiller RC, Scholefield JH. Diverticular abscess of the appendix: report of a case and review of the literature. Dis Colon Rectum. 2003. 46:832–834.
5. Collins DC. A study of 50,000 specimens of the human vermiform appendix. Surg Gynecol Obstet. 1955. 101:437–445.
6. Yamana I, Kawamoto S, Inada K, Nagao S, Yoshida T, Yamashita Y. Clinical characteristics of 12 cases of appendiceal diverticulitis: a comparison with 378 cases of acute appendicitis. Surg Today. 2012. 42:363–367.
7. Buffo GC, Clair MR, Bonheim P. Diverticulosis of the vermiform appendix. Gastrointest Radiol. 1986. 11:108–109.
8. Fitzer PM, Rao KG, Bundrick TJ. Diverticulosis of the appendix: radiographic and clinical features. South Med J. 1985. 78:1512–1514.
9. Lipton S, Estrin J, Glasser I. Diverticular disease of the appendix. Surg Gynecol Obstet. 1989. 168:13–16.
10. Shin IY, Ahn CJ, Cheon JS, Kim JG, Lee DH, You YK, et al. Diverticula of appendix associated with chronic abdominal pain: a case report. J Korean Soc Coloproctol. 2006. 22:58–61.
11. Favara BE. Multiple congenital diverticula of the vermiform appendix. Am J Clin Pathol. 1968. 49:60–64.
12. Phillips BJ, Perry CW. Appendiceal diverticulitis. Mayo Clin Proc. 1999. 74:890–892.
13. Kubota T, Omori T, Yamamoto J, Nagai M, Tamaki S, Sasaki K. Sonographic findings of acute appendiceal diverticulitis. World J Gastroenterol. 2006. 12:4104–4105.
14. Osada H, Ohno H, Saiga K, Watanabe W, Okada T, Honda N. Appendiceal diverticulitis: multidetector CT features. Jpn J Radiol. 2012. 30:242–248.
15. Choi SI, Shin JK, Lee SH, Kim DS, Lee DH, Kang YS. A case of hemorrhage from a diverticulum of the appendix. J Korean Soc Coloproctol. 2005. 21:48–51.
16. Lee YS, Lee IK, Kim JJ, Lee KH, Oh SJ, Park SM, et al. Intussusception combined with appendiceal diverticulosis in adult. J Korean Surg Soc. 2007. 72:319–322.
17. Lamps LW, Gray GF Jr, Dilday BR, Washington MK. The coexistence of low-grade mucinous neoplasms of the appendix and appendiceal diverticula: a possible role in the pathogenesis of pseudomyxoma peritonei. Mod Pathol. 2000. 13:495–501.




 ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download