Abstract
Heterotopic pancreas in the gallbladder is extremely rare and usually incidentally discovered at the pathologic examination followed by cholecystectomy for symptomatic gallbladder disease. Up to the presents, only about 30 cases have been reported. We report the case of a 36-year-old female who presented with symptoms of cholecystitis. The histological analysis followed by cholecystectomy revealed heterotopic pancreas of the cystic duct.
A heterotopic pancreas is defined as the presence of pancreatic tissue outside the boundaries of the pancreas that show no anatomical or vascular connection with the pancreatic structure [1]. The most common site of an ectopic pancreas is the upper gastrointestinal tract [2]. A heterotopic pancreas in the gallbladder is an extremely rare and usually incidentally discovered during a pathologic examination followed by cholecystectomy for symptomatic gallbladder disease. Up to the presents, only about 30 cases have been reported [3,4]. We report a case of heterotopic pancreas which presented with the clinical symptoms of cholecystitis.
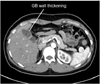
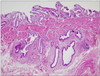
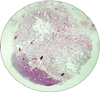
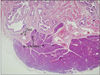
A 36-year-old female patient visited Pusan National University Hospital complaining of dyspepsia and right upper quadrant discomfort. Physical examination and laboratory results revealed no abnormal findings. The computed tomographic (CT) scan showed a segmental adenomyomatosis (ADM) (Figs. 1, 2). After one year follow-up, the symptoms of the patient had worsened. At that time a laparoscopic cholecystectomy was performed. In the gross finding of resected specimen, the wall of the gallbladder body showed gross focal thickening and luminal narrowing and the cystic duct showed nodular extraluminal thickening. Microscopically the wall of the gallbladder body demonstrated adenomyomatous hyperplasia (Fig. 3). In the examination of the cystic duct normal pancreatic tissue was revealed in subserosal layer, and the pancreatic duct lay on the muscle layer of the cystic duct. Also the pancreatic lobules were grouped on the subserosa (Fig. 4). In the high power microscopic findings, the lobules were found to contain acini and islets in normal proportions (Fig. 5).
An autopsy series demonstrated a heterotopic pancreas in 0.55% to 13.7% of patients and only 1% had ectopic pancreatic tissue in the gallbladder [5]. Heterotopic pancreas is a congenital anomaly characterized by the growth of aberrant tissue mimicking a normal pancreas without ductal or vascular continuity to the original gland. A recent theory suggested that abnormalities in the Notch signaling system, a main factor for lesion-appropriate pancreatic differentiation in the development of the foregut endoderm, lead to the development of heterotopic pancreatic tissue [6]. But there is no accepted theory that explains the exact origin of a heterotopic pancreas.
A heterotopic pancreas of the gallbladder presents with an exophytic growth that may be similar to polypoid lesions, varying in dimension from a few millimeters to 4 cm. Fifty percent of the lesions arise in the neck of gallbladder and submucosal presentation is the most common form [7]. Histologically, acinar and ductal tissues are always present, whereas islet cells are found in only one third of cases [8]. In our case, the heterotopic pancreas was a 5 mm sized subserosal lesion of the cystic duct and exocrine acinar and ductal components with islets of Langerhans were found on immunohistochemical examinations.
A heterotopic pancreas is asymptomatic and found incidentally after cholecystectomy. Generally, a preoperative diagnosis of hetrotopic pancreas in the gallbladder is difficult because of its rarity and nonspecific symptoms. In this case, we could not discriminate whether the patient's symptoms were caused by a segmental ADM or by ectopic pancreas of cystic duct.
During one-year-follow up of segmental ADM, gallbladder wall thickness had not changed but the patient's symptoms had worsened. All symptoms of the patient had disappeared after a cholecystectomy. A high level of pancreatic enzyme in gallbladder bile with an ectopic pancreas can cause pain and eventually damage the gallbladder mucosa, leading to the development of gallbladder cancer [9,10]. Therefore an ectopic pancreas of the gallbladder may be a risk factor of the development of gallbladder cancer.
In the patients who show the symptoms of benign gallbladder disease without a definitive associated lesion in imaging studies, the consideration of possible presence of ectopic pancreas of gallbladder is recommended for the diagnosis of the disease, even though it is very rare instance.
Figures and Tables
References
1. Hsia CY, Wu CW, Lui WY. Heterotopic pancreas: a difficult diagnosis. J Clin Gastroenterol. 1999. 28:144–147.
2. Lai EC, Tompkins RK. Heterotopic pancreas: review of a 26 year experience. Am J Surg. 1986. 151:697–700.
3. Neupert G, Appel P, Braun S, Tonus C. Heterotopic pancreas in the gallbladder: diagnosis, therapy, and course of a rare developmental anomaly of the pancreas. Chirurg. 2007. 78:261–264.
4. Foucault A, Veilleux H, Martel G, Lapointe R, Vandenbroucke-Menu F. Heterotopic pancreas presenting as suspicious mass in the gallbladder. JOP. 2012. 13:700–701.
5. Weppner JL, Wilson MR, Ricca R, Lucha PA Jr. Heterotopic pancreatic tissue obstructing the gallbladder neck: a case report. JOP. 2009. 10:532–534.
6. Artavanis-Tsakonas S, Rand MD, Lake RJ. Notch signaling: cell fate control and signal integration in development. Science. 1999. 284:770–776.
7. Klimis T, Roukounakis N, Kafetzis I, Mouziouras V, Karantonis I, Andromanakos N. Heterotopic pancreas of the gallbladder associated with chronic cholecystitis and high levels of amylasuria. JOP. 2011. 12:458–460.
8. Hara M, Tsutsumi Y. Immunohistochemical studies of endocrine cells in heterotopic pancreas. Virchows Arch A Pathol Anat Histopathol. 1986. 408:385–394.
9. Sato A, Hashimoto M, Sasaki K, Matsuda M, Watanabe G. Elevation of pancreatic enzymes in gallbladder bile associated with heterotopic pancreas: a case report and review of the literature. JOP. 2012. 13:235–238.
10. Jeng KS, Yang KC, Kuo SH. Malignant degeneration of heterotopic pancreas. Gastrointest Endosc. 1991. 37:196–198.




 ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download