Abstract
Purpose
The aim of this study is to evaluate the results of aspiration thrombectomy (AT) in the endovascular treatment for iliofemoral deep vein thrombosis (DVT) through the comparison of catheter directed thrombolysis (CDT) alone group and CDT with AT group.
Methods
From November 2001 to April 2011, 100 patients received endovascular treatment with CDT alone or CDT with AT for iliofemoral DVT at Yeungnam University Medical Center. We compared procedure, clinical outcomes and complications between the two groups.
Results
The mean age of patients was 60.48 ± 14.57 years. The patients consisted of 41 men and 59 women. CDT alone and CDT with AT were performed in 29 and 71 patients, respectively. The mean procedural time of the CDT-alone group was longer than the CDT with AT group (P < 0.001) and dose of urokinase used during the procedure significantly decreased in the CDT with AT group (P < 0.001). There were no statistically significant differences in clinical outcomes between the two groups. Cases of pulmonary embolism was not noted in each group in our series, but entrapped thrombus during procedure was noted in 6 of 37 in the CDT with AT group and 0 of 9 in the CDT-alone group among 46 patients with prophylactic inferior vena cava (IVC) filter insertion.
Venous thromboembolism (VTE), which contains deep vein thrombosis (DVT) and pulmonary embolism (PE), is not an uncommon medical problem [1]. The reported age standardized incidence of first time VTE was 1.92 per 1,000 person-years in the United States [2]. In Korea, the incidence of DVT was 5.31 per 100,000 in 2008 and is increasing with time [3]. VTE is a significant cause for morbidity and mortality in the general population, the socioeconomic burden due to VTE is substantial [4]. Especially, iliofemoral DVT accounts for 20-25% of lower limb DVT and has the highest risk for post thrombotic syndrome (PTS) and post phlebitic syndrome [5]. Thus, patients with iliofemoral DVT are more prone to lifelong complications. Systemic anticoagulation therapy is a classic treatment modality for VTE. However, it does not actively dissolve thrombus and has no effect on PTS prevention [6]. Therefore, the various methods for effective thrombus removal that reduce complications such as post thrombotic morbidity have been introduced [5,7].
Catheter directed thrombolysis (CDT) for iliofemoral DVT was presented in the early 1990s as an alternative to anticoagulation, systemic thrombolysis, or surgical thrombectomy [8-11]. CDT is an image-guided technique involving infusion of thrombolytic agents through a multiside hole infusion catheter or wire placed directly into a venous thrombus through a remote puncture site [12]. The main purpose of CDT is to restore the venous lumen and preserve the function of venous valves [13]. CDT improved long-term outcome after iliofemoral DVT by reducing PTS compared with conventional treatment with anticoagulation [14]. But the results of published studies demonstrated that the patients who underwent CDT needed long hospitalization and intensive care monitoring. And CDT therapy has a risk of hemorrhage, particularly in elderly patients [15]. Thus, CDT therapy may be used for patients with extensive acute proximal DVT (iliofemoral DVT, symptoms for ≤14 days, good functional status, life expectancy >1 year) who have a low risk of bleeding (grade 2B) according to the latest American College of Chest Physicians guidelines [16].
Manual aspiration thrombectomy (AT) was first reported in 1984 [17]. AT restores venous patency and relieves acute symptoms quickly as well as reduces the risk of hemorrhagic complication [18]. But AT also has several defects such as incomplete thrombus removal, the potential for vein or valve injury and embolization risks [19].
This study was conducted to evaluate the results of AT in the endovascular treatment for iliofemoral DVT through a comparison of CDT-alone group and CDT with AT group, including the amount of thrombolytic agent, procedure duration, completion of thrombus removal, symptom resolve, patency rate, etc.
From November 2001 to April 2011, 100 patients received endovascular treatment with CDT for iliofemoral DVT at Yeungnam University Medical Center. Demographic characteristics and clinical outcomes were analyzed retrospectively. The diagnosis of DVT was established using color Doppler ultrasonography (duplex scan) and 3-dimentional venous computed tomography (3D venous CT). DVT was confirmed by venography performed during endovascular treatment in all patients. We have performed CDT alone in early period (~2004) and CDT with AT in late period (~2011). For complete clot dissolution, we used urokinase in all patients. We analyzed total patients divided into two groups: 71 patients treated by CDT with AT and 29 patients treated by CDT alone. Exclusion criteria were iliofemoral DVT more than 14 days from symptom onset, patients who could not use urokinase and anticoagulation, terminally ill patients, and the presence of PE. End-points of study were recurrent symptomatic venous thrombosis, development of PE, major hemorrhage needing transfusion, and death. All patients were followed up every 6 months and duplex scans or 3D venous CT were checked.
In prone position on the angiographic table, the venography was done and the topography of the thrombus was established. After local anesthesia, an infusion catheter was introduced under ultrasonographic guidance, preferentially into the popliteal vein. A multiside hole catheter was located across the thrombosed venous segment and attached to a low dose infusion of a thrombolytic drug. Urokinase was used as the thrombolytic agent in all cases. Urokinase was given in a loading dose of 120,000-250,000 IU/hr for 2 hours followed by infusion of 30,000-60,000 IU/hr for 22 hours through the main route of catheter; the rate used depended on the patient's condition, amount of thrombus, and the patient's weight. Heparin was administered by infusion of 5,000 IU for 24 hours through the side route of catheter. Lysis progress was monitored at venography. The starting and ending times of thrombolysis, as well as the concentration and total amount of urokinase administered, were recorded. After infusion of the lytic agent, a 9 Fr VISTA guide catheter (Cordis, Miami Lakes, FL, USA) was inserted. Using a simple plastic syringe, aspiration of remnant thrombus was done gently. Aspirations were performed from the caudal to cranial ends. While pulling the catheter back, negative pressure was applied. Advancing the catheter to the more proximal site, the procedures were repeated several times. The most cranial part was aspirated last to prevent embolization of a thrombus fragment. When thromboemboli were not seen at venography, aspiration was stopped. Fluoroscopic images were used to help find residual thrombus. Percutaneous transluminal angioplasty (PTA) and stent placement were used to treat underlying severe stenoses or to treat complications. If there was significant compression of the left common iliac vein with intraluminal webs consistent with iliac vein compression syndrome (May-Thurner syndrome), or if there was more than 50% stenosis due to residual thrombi that could not be removed with CDT with/without AT in the iliac veins or the IVC, self-expanding stents were placed and dilated with a balloon catheter; Wall (Boston Scientific, Natick, MA, USA) in 10 cases, Nitis (Taewoong Medical, Seoul, Korea) in 13 cases, Zilver (Cook Ireland Ltd., Limerick, Ireland) in 4 cases, Hercules (S&G Biotech Inc., Seoul, Korea) in 5 cases and Smart (Cordis). A prophylactic retrievable IVC filter was inserted before or after the lytic infusion in 46 patients having a free floating thrombus at the IVC or common iliac vein. After recanalization of the major venous systems, including from common iliac vein to IVC junction, was achieved, a final IVC venogram was performed to search for trapped thrombus in the IVC filter. Anticoagulation therapy with warfarin sodium was initiated and continued for a minimum of 6 months. Low-molecular-weight heparin was overlapped with warfarin sodium until the international normalized radio (INR) was in the therapeutic range. Therapy was adjusted to attain an INR in the range of 2-3.
Statistical analysis was performed using the IBM SPSS ver. 18.0 (IBM Co., Armonk, NY, USA). Continuous data are reported as mean ± standard deviation. Nominal data are reported as number of subjects. The Student's t-test was used to compare the mean differences between the two groups. We compared the frequency of complete thrombus removal using chi-square. Symptom resolution was estimated by using the Fisher's exact test. Stent patency was estimated by using the Kaplan-Meier method and comparisons of patency were made with the log rank test. A P-value < 0.05 was considered to be statistically significant.
Demographic information of the patients is presented in Table 1. The mean age of patients was 60.48 ± 14.57 years (range, 27 to 83 years). The patients consisted of 41 men and 59 women. The lesion was on the right side in 17 patients and on the left side in 83 patients. CDT alone and CDT with AT were performed in 29 and 71 patients, respectively. The mean symptom duration was 5.05 ± 3.70 days (range, 1 to 15 days). 55 patients were diagnosed with May-Thurner syndrome by 3D venous CT.
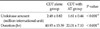
As shown in Table 2, the mean procedural time of the CDT-alone group was longer than the CDT with AT group (P < 0.001) and dose of urokinase used during the procedure significantly decreased in the CDT with AT group compared to CDT-alone group (P < 0.001).
Complete thrombus removal (≥99% elimination of thrombus) based on angiographic evidence was achieved in 48 of 71 patients (67.6%) in the CDT with AT group. In contrast, complete thrombus removal occurred in 15 of 29 patients (51.7%) in the CDT alone (P = 0.136) (Table 3). Complete symptom resolution as judged by the elimination of edema on the affected extremity within 24 hours after intervention, occurred in 61 cases (85.9%) of CDT with AT group and in 24 cases (82.8%) of CDT-alone group. There was no significant difference in symptom improvement (P = 0.456) (Table 3). PTA with stent insertion was performed in 61 patients with severe stenosis or complications. Stenting in the CDT with AT group and CDT-alone group was necessary in 45 (63.4%) and 17 cases (58.6%), respectively. There was no technical failure in stent insertion. The patency rate of iliac vein in the groups with stent (28.95%) was better than in the groups without stent (11.29%) (P = 0.026). PTS was defined as signs and symptoms including pain, heaviness, tingling sensation and swelling. There was no significant difference in the frequency of PTS between the groups with stent (10.53%) and the groups without stent (16.13%) (P = 0.433).
There were three patients with minor wound hematoma in all groups. No surgical interventions were required for these hemorrhagic complications. There was no complication related to AT or thrombolytic catheter itself. PE was not noted in all groups at arterial phase of 3D venous CT. There was no major morbidity or mortality. Follow-up was possible on all patients for an average of 37.62 ± 25.21 months (range, 1 to 82 months). No patient died as a direct result of the DVT. Follow-up information regarding lower extremity venous valvular function was collected in 72 patients by venous reflux test (20 in CDT-alone group, 52 in CDT with AT group). In venous reflux test, reflux was noted 3 in CDT-alone group (15%) and 7 in CDT with AT group (13.7%). Forty-six patients underwent prophylactic temporary IVC filter for the prevention of floating thrombus. Tulip (Cook Ireland Ltd.) was used in 35 cases and OptEase (Cordis) was used in 11 cases. Temporary IVC filter was removed within 2 weeks except patients having a free floating thrombus at the IVC after CDT with/without AT. There was no removal failure. The entrapped thrombi were founded 6 patients in only CDT with AT group. Thrombus recurrence was founded 7 patients in CDT-alone group (24.1%) and 11 patients in CDT with AT group (15.5%). The PTS was appeared 9 cases (12.68%) in CDT with AT group and 5 cases (17.24%) in CDT-alone group. There was no significant difference in PTS between the two groups (P = 0.550).
Over all patency rates of iliac vein by Kaplan-Meier method were 88.4%, 83.5%, 81.9%, 78.6% at 12, 24, 36, 48 months, respectively. Patency rates of CDT-alone group were 75.9%, 75.9%, 75.9%, 75.9% and patency rates of CDT with AT group were 90.4%, 86.6%, 83.9%, 78.2% at 12, 24, 36, 48 months, respectively (Fig. 1). There was no difference in long-term patency rate between the two groups (P = 0.546).
CDT has been accepted to be more effective and safer than systemic infusion but its many disadvantages have limited its widespread acceptance. Bleeding complications have been reported to occur in 0-25% of patients in a single-center series, and in 11% of patients in a multicenter venous registry study [10-12,20]. By adding AT during CDT procedure, shorter treatment time and more reduced thrombolytic agents contribute the decrease of bleeding complication. We found that combining CDT with AT significantly reduced the mean treatment duration compared with CDT alone (P < 0.001). And, we identified a significant reduction in mean amount of drug associated with therapy in the group treated with CDT with AT compared with CDT alone (P < 0.001). Vedantham et al. [20] investigated the effect of adjunctive mechanical thrombectomy with pharmacologic catheter-directed lower extremity venous thrombolysis. In a retrospective study of 20 patients in CDT with AT group, they demonstrated a procedural success rate of 82% and reduced doses of thrombolytic agents and infusion time compared with a previously published series of patients treated with CDT alone. The fact that the required treatment time and doses of thrombolytic agents decreased in CDT with AT group compared to CDT-alone group coincided with our data. In addition, CDT with AT was associated with a reduction in the cost of interventional material and the number of venographic assessments in the interventional suites [21]. AT is also associated with shorter intensive care unit and hospital stays as well as reduced hospital costs without difference of thrombus removal rate between CDT with AT and CDT alone [20]. We did not check the hospital costs. Because the procedure time and the amount of thrombolytic agents were decreased, medical costs might be reduced.
There were no statistically significant differences in clinical outcomes judged by complete thrombus removal and elimination of symptom between the two groups. But, the frequency of complete thrombus removal was higher in CDT with AT group (67.6%) than CDT-only group (51.7%). The frequency of symptom resolution was also higher in CDT with AT group (85.9%) than CDT-only group (82.8%).
With mechanical clot dissolution, clot migration or embolization is of clinical concern. The incidence of symptomatic PE and fatal PE during CDT was reported as 1% and 0% to 0.2%, respectively [12,22]. Kinney et al. [23] reported that CDT with AT had a higher rate of PE complications when used for hemodialysis graft declotting but not when used for DVT treatment. Cases of PE were not noted in each group in our series, but entrapped thrombus during procedure was noted in 6 of 37 cases in the CDT with AT group and 0 of 9 cases in the CDT-alone group among 46 patients previously inserted with prophylactic IVC filter. Noguchi et al. [24] reported that temporary IVC filters are useful and safe for the management of an acute proximal DVT, especially in patients who require aggressive thrombus removal. When we viewed the above results, prophylactic IVC filter insertion should be considered for the prevention of PE by floating thrombus in AT treatment.
In conclusion, our study suggested that the use of AT offers more effective thrombus removal in less time and doses of thrombolytic agents required. CDT with AT is safe and effective for the treatment of an acute iliofemoral DVT. In AT treatment, prophylactic IVC filter insertion should be considered for the prevention of PE by floating thrombus.
Figures and Tables
 | Fig. 1The patency rate of iliac vein by thrombus dissolution (P = 0.546). CDT, catheter directed thrombolysis; AT, aspiration thrombectomy. |
References
1. White RH. The epidemiology of venous thromboembolism. Circulation. 2003. 107:23 Suppl 1. I4–I8.
2. Cushman M, Tsai AW, White RH, Heckbert SR, Rosamond WD, Enright P, et al. Deep vein thrombosis and pulmonary embolism in two cohorts: the longitudinal investigation of thromboembolism etiology. Am J Med. 2004. 117:19–25.
3. Jang MJ, Bang SM, Oh D. Incidence of venous thromboembolism in Korea: from the Health Insurance Review and Assessment Service database. J Thromb Haemost. 2011. 9:85–91.
4. Cohen AT, Agnelli G, Anderson FA, Arcelus JI, Bergqvist D, Brecht JG, et al. Venous thromboembolism (VTE) in Europe. The number of VTE events and associated morbidity and mortality. Thromb Haemost. 2007. 98:756–764.
5. Nyamekye I, Merker L. Management of proximal deep vein thrombosis. Phlebology. 2012. 27:Suppl 2. 61–72.
6. Sharafuddin MJ, Sun S, Hoballah JJ, Youness FM, Sharp WJ, Roh BS. Endovascular management of venous thrombotic and occlusive diseases of the lower extremities. J Vasc Interv Radiol. 2003. 14:405–423.
7. Meissner MH, Gloviczki P, Comerota AJ, Dalsing MC, Eklof BG, Gillespie DL, et al. Early thrombus removal strategies for acute deep venous thrombosis: clinical practice guidelines of the Society for Vascular Surgery and the American Venous Forum. J Vasc Surg. 2012. 55:1449–1462.
8. Okrent D, Messersmith R, Buckman J. Transcatheter fibrinolytic therapy and angioplasty for left iliofemoral venous thrombosis. J Vasc Interv Radiol. 1991. 2:195–197.
9. Palombo D, Porta C, Brustia P, Peinetti F, Udini M, Antico A, et al. Loco-regional thrombolysis in deep venous thrombosis. Phlebologie. 1993. 46:293–302.
10. Semba CP, Dake MD. Iliofemoral deep venous thrombosis: aggressive therapy with catheter-directed thrombolysis. Radiology. 1994. 191:487–494.
11. Bjarnason H, Kruse JR, Asinger DA, Nazarian GK, Dietz CA Jr, Caldwell MD, et al. Iliofemoral deep venous thrombosis: safety and efficacy outcome during 5 years of catheter-directed thrombolytic therapy. J Vasc Interv Radiol. 1997. 8:405–418.
12. Mewissen MW, Seabrook GR, Meissner MH, Cynamon J, Labropoulos N, Haughton SH. Catheter-directed thrombolysis for lower extremity deep venous thrombosis: report of a national multicenter registry. Radiology. 1999. 211:39–49.
13. Cho JS, Martelli E, Mozes G, Miller VM, Gloviczki P. Effects of thrombolysis and venous thrombectomy on valvular competence, thrombogenicity, venous wall morphology, and function. J Vasc Surg. 1998. 28:787–799.
14. Enden T, Haig Y, Klow NE, Slagsvold CE, Sandvik L, Ghanima W, et al. Long-term outcome after additional catheter-directed thrombolysis versus standard treatment for acute iliofemoral deep vein thrombosis (the CaVenT study): a randomised controlled trial. Lancet. 2012. 379:31–38.
15. Murphy KD. Mechanical thrombectomy for DVT. Tech Vasc Interv Radiol. 2004. 7:79–85.
16. Kearon C, Kahn SR, Agnelli G, Goldhaber S, Raskob GE, Comerota AJ, et al. Antithrombotic therapy for venous thromboembolic disease: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008. 133:6 Suppl. 454S–545S.
17. Sniderman KW, Bodner L, Saddekni S, Srur M, Sos TA. Percutaneous embolectomy by transcatheter aspiration. Work in progress. Radiology. 1984. 150:357–361.
18. Kwon SH, Oh JH, Seo TS, Ahn HJ, Park HC. Percutaneous aspiration thrombectomy for the treatment of acute lower extremity deep vein thrombosis: is thrombolysis needed? Clin Radiol. 2009. 64:484–490.
19. O'Sullivan GJ. The role of interventional radiology in the management of deep venous thrombosis: advanced therapy. Cardiovasc Intervent Radiol. 2011. 34:445–461.
20. Vedantham S, Vesely TM, Parti N, Darcy M, Hovsepian DM, Picus D. Lower extremity venous thrombolysis with adjunctive mechanical thrombectomy. J Vasc Interv Radiol. 2002. 13:1001–1008.
21. Kim HS, Patra A, Paxton BE, Khan J, Streiff MB. Adjunctive percutaneous mechanical thrombectomy for lower-extremity deep vein thrombosis: clinical and economic outcomes. J Vasc Interv Radiol. 2006. 17:1099–1104.
22. Enden T, Klow NE, Sandvik L, Slagsvold CE, Ghanima W, Hafsahl G, et al. Catheter-directed thrombolysis vs. anticoagulant therapy alone in deep vein thrombosis: results of an open randomized, controlled trial reporting on short-term patency. J Thromb Haemost. 2009. 7:1268–1275.
23. Kinney TB, Valji K, Rose SC, Yeung DD, Oglevie SB, Roberts AC, et al. Pulmonary embolism from pulse-spray pharmacomechanical thrombolysis of clotted hemodialysis grafts: urokinase versus heparinized saline. J Vasc Interv Radiol. 2000. 11:1143–1152.
24. Noguchi M, Eishi K, Sakamoto I, Nakamura S, Yamachika S, Hazama S, et al. Thrombus removal with a temporary vena caval filter in patients with acute proximal deep vein thrombosis. Heart Vessels. 2003. 18:197–201.




 ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download