Abstract
The location of the sigmoid colon varies within the abdominal cavity, but its mesocolon is fixed to the left side. Right side fixation of the sigmoid colon is a very rare congenital positional anomaly. In addition, it has been reported that hepatocolic fistula is also a very rare disease that may present lower gastrointestinal bleeding. Here, the authors describe a case of a 71-year-old man who underwent surgery for hepato-sigmoidocolic fistula complicated by hepatocellular carcinoma and the right side fixation of the sigmoid colon.
From the embryonic period, most of the sigmoid colon is located in the left lower abdomen and some in the right. Regardless of its location, mesocolon of the sigmoid is always fixed to the peritoneum in the left side. Right side fixation of the sigmoid colon is a rare congenital malposition probably associated with midgut malrotation or extra-long sigmoid colon [1,2].
Hepatocolic fistula with lower gastrointestinal (GI) bleeding is a rare condition that is reported to occur by hydatid cyst or hepatocellular carcinoma [3-5]. Anatomically, if liver disease invades the colon to develop hepatocolic fistula, it may affect the ascending colon or hepatic flexure of the colon. However, in this case, right side fixation of the sigmoid colon developed a hepato-sigmoidocolic fistula. To our knowledge, this is the first successfully treated case of hepato-sigmoidocolic fistula complicated by hepatocellular carcinoma and concomitant cirrhosis.
The case was a 71-year-old male with a history of alcoholic liver cirrhosis. After being diagnosed with hepatocellular carcinoma 6 years ago, he was treated with transarterial chemoembolization (TACE) 7 times at other hospital. He visited our emergency room with lower GI bleeding. At the time of admission, the level of hemoglobin (Hb) was 7.5 g/dL, aspartate aminotransferase/alanine aminotransferase 27.8/13.8 U/L, alkaline phosphatase 41 U/L, albumin 2.8 g/dL, a-fetoprotein 26 ng/mL, and bilirubin 1.6 mg/dL. After he stabilized with transfusion of packed red blood cell (PRC), emergency colonoscopy was performed. A solitary diverticular-like lesion or ulceration with a brownish base in the sigmoid colon, 25 cm from the anal verge, was detected on colonoscopy, but the evidence of active bleeding was not shown (Fig. 1). Endoscopic clips were applied at the lesionto prevent recurrent bleeding. After bleeding was controlled, an abdominopelvic computerized scan was checked for evaluation of liver mass and other abnormalities (Fig. 2). The symptom improved and he was discharged 3 days later with plans to follow up using colonoscopy 2 months after. However, lower GI bleeding recurred after 7 weeks and the patient was admitted again. At the time of admission, Hb was 7.8 g/dL and PRC transfusion was given to stabilize the patient. The patient was diagnosed with recurrent sigmoid diverticular bleeding and was scheduled for laparoscopic segmental resection of the involved lesion of sigmoid colon. His preoperative Child-Pugh classification was grade A with serum albumin 3.3 g/dL, serum bilirubin 0.94 mg/dL, prothrombin time 12.3 seconds, no ascites, and no encephalopathy. The operation showed that the sigmoid colon was absent in the left lower abdomen, and it was not connected to the left peritoneum. The upper rectum was attached to the peritoneum of the right pelvis and extended to the upper right area, and thus the entire sigmoid mesocolon was fixed to the right parietal peritoneum and continued to the lower margin of the liver. Besides this, the cecum and the appendix were located in the central area of the abdominal cavity with no fixation and floated freely in the cavity. The finding was consistent with midgut malrotation (Fig. 3).
Under laparoscopic operative condition, the operator had to move the position from the right side to the left side of the patient, and the right side fixation of the sigmoid colon was dissected. Laparoscopic surgery was limited due to serious adhesion of proximal sigmoid colon to the liver and thus converted to laparotomy with upper midline incision. The upper fixation area of the sigmoid colon could be mobilized with concomitant en bloc nonanatomical excision of the liver (segment 6) containing hepatocellular carcinoma. After complete mobilization of the sigmoid colon with a part of the liver, segmental resection of the sigmoid colon was performed with about 10 cm resection margins proximally and distally, respectively. After surgery, the patient was treated for ascites and hydrothorax for about 20 days, which were free of malignant cells, and recovered without additional complications. Gross findings of the specimen showed a perforation hole between the sigmoid colon and liver, and hepatocellular carcinoma tissue. The microscopic findings revealed a 4.5 cm × 5 cm sized metastatic hepatocellular carcinoma invading the sigmoid colon. The central part of the tumor presented with necrosis with the peripheral part constituting intact cancer cells, suggesting marginal recurrence at the previous tumor site after TACE (Fig. 4).
In this case, besides the fixation anomaly of the sigmoid colon, midgut malrotation was considered a congenital anomaly. So far, only a couple of cases of right side fixation of the sigmoid colon have been reported [6-9]. Four or 5 cases were detected during autopsy, and another case was detected during X-ray examination. To our knowledge, our case is the first detected during the actual surgery. In most cases, it was considered to occur congenitally, since the sigmoid colon was excessively long. In one case that was detected during X-ray examination, it was reported to have occurred due to midgut malrotation [8]. It may be inferred from such evidence when midgut malrotation is developed, the cecum and the ascending colon float freely within the abdominal cavity, similar to the small bowel. Consequently, the empty space in the right side is occupied by the redundant sigmoid colon, and the fixation between the mesocolon of the sigmoid colon and peritoneum of the right side may occur during the later period of the fetus; and thus, such congenital malposition is developed. Therefore, summarizing the cases reported until now demonstrates that the cause of right side fixation of the sigmoid colon may be as a result of extra-long redundancy of sigmoid colon and/or midgut malrotation.
In the era of laparoscopic colorectal surgery, if the right side fixation of sigmoid colon is encountered during surgery, it may prove problematic, such that the operator position would need to be changed to the left side of the patient or an additional trochar may be inserted in the left side of abdomen.
The colon is located quite close to the liver within the abdominal cavity, particularly the ascending colon or the hepatic flexure of the colon. Despite this anatomical proximity, hepatocolic fistula is extremely rare. Until now, only 3 cases of hepatocolic fistula have been reported. Two of which were caused by hydatid disease [4,5], the other by an invasion of hepatocellular carcinoma [3], which corresponds to this case. In that case, the patient with a history of alcohol abuse showed lower GI bleeding and was confirmed with hepato-ascending-colic fistula as a result of invasion of hepatocellular carcinoma on the computed tomographic scan, water-soluble enema, colonoscopy and biopsy. The patients died a few weeks later without surgery, but, in our case, even though we didn't suspect, preoperatively, the hepato-colic fistula in the patient with lower GI bleeding, the cirrhotic patient with hepatocellular carcinoma was treated with operation. The preoperative diagnosis was considered as a solitary diverticulum or Dieulafoy's lesion of the sigmoid colon. In another case, extensive hepatocelluar carcinoma infiltrated to the hepatic flexure and induced a massive lower gastrointestinal bleeding, which caused the death of the patient [10]. It has been reported that, in hepatocellular carcinoma patients, gastrointestinal bleeding occurs as the hepatocellular carcinoma metastasize or directly infiltrate to the stomach, the duodenum, or rarely to the colon.
In summary, we report a combination case of congenital right side fixation of the sigmoid colon and hepato-sigmoidocolic fistula in a patient with hepatocellular carcinoma and cirrhosis, which was treated with surgery successfully. And when a patient with hepatocellular carcinoma develops lower GI bleeding, the possibility of hepatocolic fistula should be considered.
Figures and Tables
Fig. 1
Colonoscopic findings of the bleeding lesion of the colon. There was no active bleeding but 2 cm sized, solitary ulcerative lesion with dark-brown and dirty base at the sigmoid colon, about 30 cm from the anal verge, in which endoclips were applied (left side).
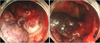
Fig. 2
Abdominopelvic computed tomographic scan showing a exophytic growth of the tumor from the right hepatic lobe. Endoclips applied in the bleeding lesion of the sigmoid colon during previous colonoscopy were visible very close to the hepatic tumor, but that finding was not noticed preoperatively.

Fig. 3
Schematic drawing of the operation finding. Sigmoid colon and upper rectum were fixed to the right side of parietal peritoneum. Proximal part of the sigmoid colon was strongly adhered to the low surface of liver. And cecum and ascending colon was placed inner part of abdominal cavity and not fixed, consistent with midgut malrotation.

Fig. 4
Gross specimen and microscopic findings; (A) outer side of the gross specimen showing segmentally resected sigmoid colon together with hepatic tissue; (B) inner view of the gross specimen, showing the fistula opening; (C) microscopically in lower power field, tumor is seen in inked serosa margin (H&E, ×40); (D) in high power field, metastatic hepatocellular carcinoma is expanding from serosa to mucosa (H&E, ×100).

References
1. Malas MA, Aslankoc R, Ungor B, Sulak O, Candir O. The development of large intestine during the fetal period. Early Hum Dev. 2004. 78:1–13.
2. Fiorella DJ, Donnelly LF. Frequency of right lower quadrant position of the sigmoid colon in infants and young children. Radiology. 2001. 219:91–94.
3. Berkelhammer C, Janarthan B, Bhagavan M, Schreiber S. Hepatocolic fistula and lower GI bleeding in hepatoma. Am J Gastroenterol. 1996. 91:2625–2626.
4. Ortiz H, Carmona JA, Perez-Cabanas I. Colohepatic fistula due to hydatid disease. Report of a case. Dis Colon Rectum. 1988. 31:546–547.
5. Morris DL, Smith WD, Alexander-Williams J. Colohepatic fistula due to hydatid disease. World J Surg. 1983. 7:797–798.
6. Bhattachayya B. Three cases of right-sided sigmoid colon. J Anat. 1926. 60(Pt 2):229–232.
7. Wondrak E. Right-side fixation of the sigmoid colon. Rozhl Chir. 1957. 36:158–160.
8. Schulz E, Bettenhaeuser K. On the roentgenologic differentiation of anomalies of the intestinal location (case of a fixed right location of an elongated sigmoid due to malrotation I). Fortschr Geb Rontgenstr Nuklearmed. 1963. 99:801–804.
9. Komiyama M, Shimada Y. A case of a right-sided sigmoid colon. Kaibogaku Zasshi. 1991. 66:537–540.
10. Singh Kalra TM, Mangla JC, Schwartz S, Lee JC. Hepatoma presenting as lower gastrointestinal bleeding. Am J Gastroenterol. 1977. 67:485–488.




 ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download