Abstract
Gastrojejunocolic fistula is a rare condition after gastrojejunostomy. It is severe complications of gastrojejunostomy, which results an inadequate resection or incomplete vagotomy during peptic ulcer surgery. The symptoms are diarrhea, upper abdominal pain, bleeding, vomiting and weight loss. A 55-year-old man with chronic diarrhea and weight loss for 6 months visited Dankook University Hospital. The patient had received a truncal vagotomy and gastrojejunostomy for duodenal ulcer obstruction 15 years previously. The patient underwent gastroscopy and upper gastrointestinal series evaluations, which detected the gastrojejunocolic fistula. After improving of malnutrition, an exploratory laparotomy was undertaken, which revealed that the gastrojejunostomy site and the T-colon formed adhesion and fistula. En block resection of the distal stomach and T-colon included the gastrojejunocolic fistula, and Roux-en-Y gastrojejunostomy was performed. Recovery was uneventful and the patient remained well at the follow-up. We report a gastrojejunocolic fistula, which is a rare case after gastrojejunostomy.
Gastrojejunocolic fistula (GJF) is a rare and late complication of gastrojejunostomy applied for recurrent peptic ulcer disease. It was thought to be induced by a stomal ulcer, due to inadequate gastrectomy or incomplete vagotomy [1,2]. The symptoms in these situations include upper abdominal pain, weight loss, diarrhea, gastrointestinal bleeding, and fecal vomiting [3]. These patients are cachectic and dehydrated, with labs showing malnutrition. Barium upper gastrointestinal series (UGIS), gastroscopy, and colonoscopy are used for diagnosis [1]. Although the occurrence of GJF has decreased remarkably as a result of better treatment, the modern management of this condition and the generally accepted surgical treatment strategies must be discussed.
A 55-year-old man was admitted to the medical center at Dankook University Hospital in December 2011. The patient had complaints of chronic watery diarrhea that occurred immediately after meals for 6 months, general weakness, and a weight loss of 15 kg during a 3-month period. Past medical history revealed primary repair for duodenal ulcer perforation in 1982 and truncal vagotomy and gastrojejunostomy in 1996 due to gastric outlet obstruction. The patient was cachectic and dehydrated. Laboratory parameters revealed malnutrition with albumin level of 2.6 g/dL (range, 3.4 to 4.8), protein level of 4.3 g/dL (range, 6.4 to 8.3), and cholesterol of 72 mg/dL (range, 120 to 239). Simple abdomen X-ray film was unremarkable.
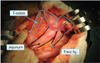
The infusion of contrast into the colon was identified near the gastrojejunostomy, according to a thin barium UGIS double study (Fig. 1). Copious fecal fluid was evident in the stomach through a gastroscopy, and a canal was identified in the previous gastrojejunostomy site and low body posterior wall connected directly to the colon (Fig. 2). A colonscopy revealed an anastomosis site was seen in the transverse colon stricture and T-colon connected to the stomach.
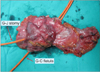
After improving the patient's state of malnutrition and his weight through total parenteral nutrition (TPN), the patient was taken into the operation room and an exploratory laparotomy was undertaken. In surgery, the gastrojejunostomy site and the midportion of the T-colon formed adhesion and fistula (Figs. 3-5). Distal gastrectomy, Roux-en-Y anastomosis, T-colon segmental resection and anastomosis were performed. Recovery was uneventful and the patient remained well at the follow-up. Histology of the resected specimen revealed chronic peptic ulcer with fibrosis and chronic inflammation. Three month after discharge, there was no ulcer, inflammation or passage disturbance at anastomosis site on endoscopic examination and the patient improved his symptoms. We planned to monitor the patient with endoscopy, annually.
Along with the development of medical treatment, such as H2 receptor blocker, proton pump inhibitors, and eradication of Helicobacter pylori, the need for an operative treatment for peptic ulcer disease decreased, dramatically [1]. For such a reason, the incidence rate of these fistulas has been remarkably decreased [4]. The symptoms of GJF are diarrhea with food containing stools, upper abdominal pain or discomfort, gastrointestinal bleeding, fecal vomiting, weight loss, and general weakness. Anemia, hypoalbuminemia, and electrolyte disturbances are common laboratory findings [5]. The most commonly used diagnostic tool includes barium enema or UGIS, and endoscopy. Computed tomography is used to determine this complex fistula and to exclude extra-abdominal diseases that may define underlying etiology [6]. Gastroscopy and colonoscopy is a diagnostic tool that can identify the orifice of the fistula, find intraluminal diseases, and rule out malignancy thorough an endoscopic biopsy [7]. The conventional treatment for GJF includes improving the nutritional status and two-to-three-phased operations with colostomy to minimize mortality [8]. Today, however, due to improved parenteral and enteral support treatment, single-stage procedures can be applied and these have been favored to minimize mortality [1,8,9]. In our case, truncal vagotomy was performed in previous operation on medical record, therefore we didn't perform truncal vagotomy. If truncal vagotomy has not previously been completed, it is advisable to perform it nonetheless.
In conclusion, the development of the peptic ulcer agents including those capable of eradicating H. pylori, GJF incidence has decreased dramatically. But, since the fistula formation needs a 20 to 30 years latent period after surgery, this complication can occur. Today, one-stage resection is preferred over the staged operation if the general status of the patient is suitable [5]. TPN is a crucial factor for recovering the patient's malnutrition status and so should precede surgery.
Figures and Tables
Fig. 1
Upper gastrointestinal series assessment confirming the passage between the corpus of the stomach and the transverse colon (arrow).

Fig. 3
At surgery, gastrojejuno-colic fistula was identified and gatrojejunostomy was performed by retrocolic fashion, as in the previous surgery.
References
1. Kece C, Dalgic T, Nadir I, Baydar B, Nessar G, Ozdil B, et al. Current diagnosis and management of gastrojejunocolic fistula. Case Rep Gastroenterol. 2010. 4:173–177.
2. Takemura M, Hamano G, Nishioka T, Takii M, Mayumi K, Ikebe T. One-stage laparoscopic-assisted resection of gastrojejunocolic fistula after gastrojejunostomy for duodenal ulcer: a case report. J Med Case Rep. 2011. 5:543.
3. Chung DP, Li RS, Leong HT. Diagnosis and current management of gastrojejunocolic fistula. Hong Kong Med J. 2001. 7:439–441.
4. D'Amata G, Rahili A, Karimdjee-Soilihi B, Gelsi E, Avallone S, Benchimol D. Gastrojejunocolic fistula after gastric surgery for duodenal ulcer: case report. G Chir. 2006. 27:360–362.
5. Cody JH, DiVincenti FC, Cowick DR, Mahanes JR. Gastrocolic and gastrojejunocolic fistulae: report of twelve cases and review of the literature. Ann Surg. 1975. 181:376–380.
6. Matsuo S, Eto T, Ohara O, Miyazaki J, Tsunoda T, Kanematsu T. Gastrocolic fistula originating from transverse colon cancer: report of a case and review of the Japanese literature. Surg Today. 1994. 24:1085–1089.
7. Choi SW, Yang JM, Kim SS, Kang SH, Ro HJ, Song KS, et al. A case of combined gastrojejunal and gastrocolic fistula secondary to gastric cancer. J Korean Med Sci. 1996. 11:437–439.
8. Pfeiffer DB. The surgical treatment of gastrojejunocolic fistula. Surg Gynecol Obstet. 1941. 72:282–289.
9. Subramaniasivam N, Ananthakrishnan N, Kate V, Smile SR, Jagdish S, Srinivasan K. Gastrojejunocolic fistula following surgery for peptic ulcer. Trop Gastroenterol. 1997. 18:183–187.




 ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download