Abstract
Purpose
There is controversy concerning the effect of a positive T-lymphocytotoxic crossmatch (TLC) on clinical outcomes in adult living donor liver transplantation (LDLT). The aim of this study was to investigate the effect of TLC on clinical outcomes in LDLT and to determine how long a pretransplant positive TLC continues after liver transplantation (LT).
Methods
Between January 2005 and June 2010, 219 patients underwent adult LDLT at National Cancer Center. The TLC test was routinely performed before LDLT. TLC test results were positive in 8 patients (3.7%). Patients were divided into 2 groups according to the result of TLC: positive TLC (n = 8) and negative TLC (n = 211) groups. All patients with a pretransplant positive TLC (n = 6) underwent a TLC test every week until negative conversion of TLC, except 2 patients who refused to receive the TLC test.
The clinical effect of a pretransplant positive T-lymphocytotoxic crossmatch (TLC) in the prediction of liver transplantation (LT) outcome is controversial [1]. LT is often performed before the results of crossmatch testing between the donor and recipient can be obtained. In many cases, a pretransplant positive TLC between a recipient and donor is shown subsequent to LT because of time constraints. Nevertheless, hyperacute rejection rarely occurs in patients with a pretransplant positive TLC [2].
There are several studies of clinical outcomes in patients with positive crossmatch grafts. Some studies have reported that the presence of pretransplant lymphocytotoxic antidonor antibodies is not a prognostic factor in deceased donor liver transplantation (DDLT) [3,4]. However, more recent studies have contradicted these findings, showing higher acute or chronic rejection rates and worsening graft survival in patients who have a positive TLC [5-10]. The detrimental effects of a pretransplant positive TLC on patient and graft survival have also been emphasized in other studies of DDLT [1,2,6,11-15].
Recently, adult living donor liver transplantation (LDLT) has been widely performed because of the shortage of deceased donors. Similar to DDLT, there is controversy concerning the effect of a pretransplant positive TLC on clinical outcomes in LDLT. Even though there have been many studies on the effect of a pretransplant positive TLC, there have been few studies on the effect of a positive TLC after LT. Moreover, to the best of our knowledge, there has been no study on how long pretransplant positive TLC continues after LT.
The aim of this study was to investigate the effect of TLC on clinical outcome in LDLT and to determine how long pretransplant positive TLC continues after LT.
LT was performed on a total of 230 patients at the National Cancer Center, Korea, between January 2005 and June 2010. Of these patients, 11 were excluded from this study due to DDLT. The remaining 219 patients were enrolled in the study (171 males, 48 females; median age, 53 years; range, 25 to 70 years). The donors were 134 men and 85 women with a median age of 35 years (range, 17 to 66 years). All donors had ABO blood types compatible or identical with the recipients. One hundred ninety-nine donors were related to the recipients and 20 donors were unrelated to the recipients. One hundred ninety-nine donors were selected among relatives within the third degree of consanguinity or were spouses. The relations of the donors to the patients were 127 children, 19 siblings, 1 parent, 32 spouses, 8 nephews and others (2 brothers-in-law, 2 sisters-in-law, 8 cousins, and 20 unrelated donors). The types of surgery for donors were 198 right hemihepatectomies, 11 extended right hemihepatectomies, 1 extended left hemihepatectomy, 1 left hemihepatectomy. Only 1 patient received auxiliary partial orthotopic LT. In accordance with the Declaration of Helsinki recommendations, approval was obtained from the institutional review board at the National Cancer Center, and informed consent was provided to all recipients and donors.
Before June 2008 or after April 2010, a double (prednisolone and tacrolimus) or a triple (prednisolone, tacrolimus and mycophenolate mofetil) combination regimen was used. Prednisolone was tapered and stopped within 6 months of LT. Between June 2008 and March 2010, early steroid withdrawal regimen was used. Combined with basiliximab induction, prednisolone was tapered rapidly within 6 days after LT. Tacrolimus with or without mycophenolate mofetil was maintained thereafter. Mycophenolate mofetil was discontinued within 6 months.
Acute cellular rejection (ACR) was defined as a biopsy-proven episode [16] and was graded according to the Banff schema [17]. The indication for liver biopsy was a significant increase in the levels of total bilirubin, aspartate and alanine aminotransferase. The defining limit was 6 weeks [18]. An acute rejection episode was treated with bolus intravenous methylprednisolone, regardless of the severity at a starting dose of 20 mg/kg/day. The dose was reduced by half per day, and the therapy was continued for 5 days. High-dose methylprednisolone therapy was given 1 or 3 times. There was no case of steroid resistant cellular rejection.
Complement-dependent-cytotoxicity and flow cytometry were performed preoperatively in all cases. The lymphocytotoxic crossmatch test was performed according to the National Institute of Health standard T-cell crossmatch test (T-NIH), antiglobulin T-cell crossmatch test (T-AHG), B-cell crossmatch, and T-cell flow cytometry (FACS Calibur Analyzer, Becton-Dickinson, San Jose, CA, USA). A positive TLC was defined as 1) a positive T-NIH result, 2) a positive T-AHG result or 3) greater than 20% cell death as measured by T-cell flow cytometry. B-Cell crossmatch was positive in 1 patient and regarded as a negative crossmatch. When a pretransplant TLC test was positive, the test was performed once a week post until negative conversion of TLC was found.
Continuous variables are expressed as median and range (minimum to maximum). Group comparisons were made with the Wilcoxon-Mann-Whitney test. Categorical variables are expressed as counts and percentage. Group comparisons were made with the Fisher exact test. Survival was assessed with the Kaplan-Meier nonparametric survivorship function, and group comparisons were made with the log-rank test. A P-value < 0.05 was considered significant.
TLCs were performed on 219 patients. The TLC test was positive in 8 patients and negative in 211 patients. There was no difference between the two groups in the indications stratified by the test results. Viral related liver cirrhosis with/without hepatocellular carcinoma was the most common indication for LDLT in the positive (75.0%) and negative (89.0%) TLC groups. In adult LDLT recipients at our institution, the rate of pretransplant positive TLC was 3.7% (8/219).
The demographic and intraoperative data of both groups are shown in Table 1. The pretransplant model for end-stage liver disease (MELD) score (P = 0.003), Child-Pugh classification (P = 0.031) and history of pretransplant blood transfusion (P = 0.021) were significantly higher in the positive TLC group. There were no significant differences between both groups in recipient age and sex, donor age and sex, etiology of liver disease, graft recipient weight ratio, relation to the recipient, immunosuppression, operation time, cold ischemic time, and intraoperative packed red blood cells transfusion.
ACR was not significantly different between both groups. The incidence of ACR within 6 weeks was 0% (0/8) in the positive TLC group and 6.6% (14/211) in the negative TLC group. The median time to ACR was 13 days (range, 5 to 45 days) in the negative TLC group. The severity of the episode was mostly mild (76%). None of the patients experienced episodes of severe or refractory rejection.
Table 2 shows the incidence of surgical complications after LDLT in each group. There was no significant difference between both groups in the incidence of hepatic artery thrombosis, hepatic vein stenosis and portal vein stenosis. Biliary tract complications, including biliary leakage and anastomotic stricture, were not significantly different between both groups. There was no significant difference between both groups in the incidence of reoperations.
Fig. 1 shows LDLT patient survival rates at our center. Based on the Kaplan-Meier analysis, 1- and 3-year patient survival rates were 85.7% and 85.7%, respectively, in the positive TLC group, while they were 94.6% and 85.6%, respectively, in the negative TLC group; the differences between both groups were not statistically significant (P = 0.68). One- and 3-year graft survival rates were 85.7% and 85.7%, respectively, in the positive group, and 93.9% and 83.7%, respectively, in the negative group (P = 0.73) (Fig. 2).
Table 3 shows the perioperative TLC findings and clinical outcomes of 8 patients. All 6 patients with a positive pretransplant TLC (2 patients were excluded because of refusal to receive the test after LT) had a negative TLC following LT without any treatment. The median time to a negative conversion of TLC was 1.5 weeks (range, 1 to 3 weeks). Three of 6 patients (50%) with a pretransplant positive TLC had a negative TLC in the first postoperative week. In the other 3 patients (cases 3, 7, and 8), titers of antidonor antibodies decreased as measured by the complement-dependent cytotoxicity test or the percentages of cell death decreased as assessed by flow cytometry. TLC test results were negative in cases 3 and 8 in the second postoperative week and in case 7 in the third postoperative week.
Our frequency of a positive TLC test results (3.7%) is similar to those of other centers [19,20]. Patients with a pretransplant positive TLC had high MELD score, poor Child-Pugh classifications and higher percentage of pretransplant blood transfusion. The reason for the differences may be that most patients with a pretransplant positive TLC had a prolonged prothrombin time and received some blood transfusions prior to LT, such as fresh frozen plasma or platelet, which may have contained some foreign leukocytes with antihuman leukocyte antigen causing the production of antidonor specific antibodies in recipient sera. Saito et al. [21] have demonstrated, in a study of pediatric LDLT, that the positivity rate of the pretransplant lymphocytotoxic crossmatch tests is higher in pediatric patients than in adult patients. They also mentioned that the reason for this discrepancy may be that most cases in their study had biliary atersia and received some blood transfusions prior to LT. This suggestion concurs with our study. Koneru et al. [22] have reported the effect of blood transfusion on the prognoses of liver recipients. They also stated that transfusion recipients have significantly higher panel reactive antibody levels (P < 0.02). Even though this did not reach statistical significance, there was tendency toward higher incidence of a positive crossmatch result. Judging from these facts, there may be a relationship between the presence of history of pretransplant blood transfusion and the positivity of TLC results.
Some authors have reported that a positive TLC before LDLT is closely related to a higher ACR [5,20,23] and lower graft or patient survival [5,23,24]. They recommend that a pretransplant positive crossmatch be regarded as a factor predicting lower liver allograft survival and be used as an indicator for the use of more aggressive and individualized immunosuppressive regimens [5,19,23,25,26]. However, some previous studies have demonstrated that a pretransplant positive TLC does not negatively affect graft or patient survival in LDLT and does not increase ACR in pediatric LDLT [21]. In our study, we confirmed that ACR and graft or patient survival did not increase in the positive TLC group compared to the negative group in adult-to-adult LDLT.
There are several reports about the relationship between the pretransplant lymphocytotoxic crossmatch and patient or allograft survival in LDLT [5,19,20,23,24,27,28]. Attention should be paid to the evaluation of the cause of mortality after solid organ transplantation. Infection or multiorgan failure is often described as the major cause of mortality in many studies, which should be considered comprehensively. In our opinion, when discussing the effect of crossmatch results on the outcomes of LDLT, immunologic cause should be precisely investigated. In our study, none died of an immunologic disease. The most common cause of death in our study was recurrence of malignancy in the negative (n = 10) and positive (n = 1) TLC groups. Also, the most common cause of death during initial hospitalization was infection (n = 6) in the negative TLC group. Since we minimized confounding bias, such as nonimmunologic reasons for death and aggressive tailored immunosuppression, our study precisely examined the effect of a pretransplant positive TLC on patient or graft survival.
Takaya et al. [5] have documented that the incidence of bile duct complications increased with crossmatch positivity. However, Suehiro et al. [25] have reported that there is no significant difference between the positive and negative crossmatch groups. There have been few reports about the relationship of the incidence of surgical complications and crossmatch in adult LDLT. Our study demonstrates that pretransplant crossmatch results are not related to the incidence of posttransplant complications in patients undergoing adult LDLT.
Suh et al. [24] have shown that pretransplant positive TLC is an independent risk factor causing early death after adult-to-adult LDLT using small-for-size grafts. They stated that all 4 patients died of multiorgan failure after early acute rejection episodes. It was difficult to determine whether the causes of graft loss were truly related with the acute rejection episodes. They also mentioned that a small-for-size graft is related to detrimental outcomes. Three of the 4 patients had nonimmunologic disorder complications, such as hepatic venous stenosis, bleeding and sigmoid volvulus in the early postoperative period. Surgical repair was required for the complications before liver failure developed. In our study, 4 of the 8 patients underwent LDLT using a small liver graft (graft recipient weight ratio <1%) (Table 3). There were no mortalities in the early postoperative period in all 4 patients. LDLT using small-for-size graft can be safely performed on patients with a pretransplant positive TLC without considering any immunologic treatment.
It is well known that patients with higher MELD scores before LT can detrimentally affect early posttransplant stages. Nevertheless, although the positive TLC group had higher MELD scores, the overall survival or graft survival rate did not show any difference between the 2 groups. These results can strongly support our conclusion that pretransplant positive TLC does not affect clinical outcomes of LDLT.
In our study, we found that cross-reactivity of T-lymphocyte disappeared after LT within 3 weeks (range, 1 to 3 weeks) without any immunologic treatment. We cannot give a precise explanation for the rapid disappearance of cross-reactivity after LT. A plausible explanation may be that liver allografts have a great capacity for secretion of soluble class I histocompatibility antigen into circulation and absorption of antidonor antibodies by Kupffer's cells [11].
All patients undergoing posttransplant TLC test (n = 6) lost cross-reactivity rapidly within 3 weeks. None had an ACR episode. Based on these findings, it is conceivable that ACR within 6 weeks might be not related to a pretransplant positive crossmatch but posttransplant positive crossmatch. Further studies with a larger sample size are required to investigate the association between ACR and maintenance of a posttransplant positive TLC.
Previous studies of crossmatch in LT have used the ACR definition [9,20,21,27,28]. In our study, we adopted this definition. However, donor specific antibodies can attribute to antibody-mediated rejection by which acute humoral rejection is mainly associated. Unfortunately, we did not perform C4d staining in all biopsy samples. Therefore, we could not provide the real incidence of acute humoral rejection. This is a limitation of this study.
In conclusion, this study demonstrates that, in LDLT, pretransplant TLC results may not be related to the posttransplant incidence of surgical complications and rejection episodes or graft and patient survival. Therefore, pretransplant TLC may not be useful for donor selection. Some aggressive and tailored immunosuppressive regimens should not be considered in patients with a pretransplant positive TLC after LDLT. In addition, this study demonstrates that cross-reactivity of T-lymphocyte disappeared after LT within 3 weeks (range, 1 to 3 weeks) without any immunologic treatment.
Figures and Tables
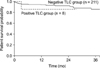 | Fig. 1Kaplan-Meier patient survival curves of 219 patients underwent adult-to-adult living donor liver transplantation according to their pretransplant T-lymphocytotoxic crossmatch (TLC) results. The 1- and 3-year patient survival rates were 85.7% and 85.7%, respectively, in the positive crossmatch group (n = 211, solid line), while they were 94.6% and 85.6%, respectively, in the negative crossmatch group (n = 8, dashed line); the difference between the groups was not statistically significant (P = 0.68). |
 | Fig. 2Kaplan-Meier graft survival curves of 219 patients underwent adult-to-adult living donor liver transplantation according to their pretransplant T-lymphocytotoxic crossmatch (TLC) results. The 1- and 3-year patient survival rates were 85.7% and 85.7%, respectively, in the positive crossmatch group (n = 211, solid line), while they were 93.9% and 83.7%, respectively, in the negative crossmatch group (n = 8, dashed line); the difference between the groups was not statistically significant (P = 0.73). |
Table 1
Comparison of demographic and intraoperative data between the positive and negative T-lymphocytotoxic crossmatch groups

References
1. Castillo-Rama M, Castro MJ, Bernardo I, Meneu-Diaz JC, Elola-Olaso AM, Calleja-Antolin SM, et al. Preformed antibodies detected by cytotoxic assay or multibead array decrease liver allograft survival: role of human leukocyte antigen compatibility. Liver Transpl. 2008. 14:554–562.
2. Muro M, Marin L, Miras M, Moya-Quiles R, Minguela A, Sanchez-Bueno F, et al. Liver recipients harbouring anti-donor preformed lymphocytotoxic antibodies exhibit a poor allograft survival at the first year after transplantation: experience of one centre. Transpl Immunol. 2005. 14:91–97.
3. Iwatsuki S, Rabin BS, Shaw BW Jr, Starzl TE. Liver transplantation against T cell-positive warm crossmatches. Transplant Proc. 1984. 16:1427–1429.
4. Iwatsuki S, Iwaki Y, Kano T, Klintmalm G, Koep LJ, Weil R, et al. Successful liver transplantation from crossmatch-positive donors. Transplant Proc. 1981. 13(1 Pt 1):286–288.
5. Takaya S, Bronsther O, Iwaki Y, Nakamura K, Abu-Elmagd K, Yagihashi A, et al. The adverse impact on liver trans-plantation of using positive cytotoxic crossmatch donors. Transplantation. 1992. 53:400–406.
6. Charco R, Vargas V, Balsells J, Lazaro JL, Murio E, Jaurrieta E, et al. Influence of anti-HLA antibodies and positive T-lymphocytotoxic crossmatch on survival and graft rejection in human liver transplantation. J Hepatol. 1996. 24:452–459.
7. Goggins WC, Fisher RA, Kimball PM, Wolfe L, Hill BE, Pietruszka TD, et al. The impact of a positive crossmatch upon outcome after liver transplantation. Transplantation. 1996. 62:1794–1798.
8. Dawson S 3rd, Imagawa DK, Johnson C, Cecka M, Terasaki PI, Shackleton CR, et al. UCLA liver transplantation: analysis of immunological factors affecting outcome. Artif Organs. 1996. 20:1063–1072.
9. Bathgate AJ, McColl M, Garden OJ, Forsythe JL, Madhavan KK, Hayes PC. The effect of a positive T-lymphocytotoxic crossmatch on hepatic allograft survival and rejection. Liver Transpl Surg. 1998. 4:280–284.
10. Gordon RD, Fung JJ, Markus B, Fox I, Iwatsuki S, Esquivel CO, et al. The antibody crossmatch in liver transplantation. Surgery. 1986. 100:705–715.
11. Demetris AJ, Murase N, Nakamura K, Iwaki Y, Yagihashi A, Valdivia L, et al. Immunopathology of antibodies as effectors of orthotopic liver allograft rejection. Semin Liver Dis. 1992. 12:51–59.
12. Doran TJ, Geczy AF, Painter D, McCaughan G, Sheil AG, Susal C, et al. A large, single center investigation of the immunogenetic factors affecting liver transplantation. Transplantation. 2000. 69:1491–1498.
13. Doyle HR, Marino IR, Morelli F, Doria C, Aldrighetti L, McMichael J, et al. Assessing risk in liver transplantation. Special reference to the significance of a positive cytotoxic crossmatch. Ann Surg. 1996. 224:168–177.
14. Hathaway M, Gunson BK, Keogh AC, Briggs D, McMaster P, Neuberger JM. A positive crossmatch in liver transplantation: no effect or inappropriate analysis? A prospective study. Transplantation. 1997. 64:54–59.
15. Nikaein A, Backman L, Jennings L, Levy MF, Goldstein R, Gonwa T, et al. HLA compatibility and liver transplant outcome. Improved patient survival by HLA and cross-matching. Transplantation. 1994. 58:786–792.
16. International Working Party. Terminology for hepatic allograft rejection. Hepatology. 1995. 22:648–654.
17. Demetris A, Adams D, Bellamy C, Blakolmer K, Clouston A, Dhillon AP, et al. An International Panel. Update of the International Banff Schema for Liver Allograft Rejection: working recommendations for the histopathologic staging and reporting of chronic rejection. Hepatology. 2000. 31:792–799.
18. Wiesner RH, Demetris AJ, Belle SH, Seaberg EC, Lake JR, Zetterman RK, et al. Acute hepatic allograft rejection: incidence, risk factors, and impact on outcome. Hepatology. 1998. 28:638–645.
19. Ashihara E, Tsuji H, Sakashita H, Haga H, Yurugi K, Kimura S, et al. Antidonor antibody in patients receiving ABO-identical and HLA-mismatched living donor liver transplants: effect on survival. Transplantation. 2007. 83:506–509.
20. Sugawara Y, Tamura S, Kaneko J, Togashi J, Makuuchi M, Kokudo N. Positive lymphocytotoxic crossmatch does not adversely affect survival in living donor liver transplantation. Dig Surg. 2009. 26:482–486.
21. Saito T, Mizuta K, Hishikawa S, Kawano Y, Sanada Y, Fujiwara T, et al. Lymphocytotoxic crossmatch in pediatric living donor liver transplantation. Pediatr Transplant. 2009. 13:194–199.
22. Koneru B, Harrison D, Rizwan M, Holland BK, Ippolito T, Holman MJ, et al. Blood transfusions in liver recipients: a conundrum or a clear benefit in the cyclosporine/tacrolimus era? Transplantation. 1997. 63:1587–1590.
23. Hori T, Uemoto S, Takada Y, Oike F, Ogura Y, Ogawa K, et al. Does a positive lymphocyte cross-match contraindicate living-donor liver transplantation? Surgery. 2010. 147:840–844.
24. Suh KS, Kim SB, Chang SH, Kim SH, Minn KW, Park MH, et al. Significance of positive cytotoxic cross-match in adult-to-adult living donor liver transplantation using small graft volume. Liver Transpl. 2002. 8:1109–1113.
25. Suehiro T, Shimada M, Kishikawa K, Shimura T, Soejima Y, Yoshizumi T, et al. Influence of HLA compatibility and lymphocyte cross-matching on acute cellular rejection following living donor adult liver transplantation. Liver Int. 2005. 25:1182–1188.
26. Takakura K, Kiuchi T, Kasahara M, Uryuhara K, Uemoto S, Inomata Y, et al. Clinical implications of flow cytometry crossmatch with T or B cells in living donor liver transplantation. Clin Transplant. 2001. 15:309–316.
27. Sugawara Y, Makuuchi M, Kaneko J, Kishi Y, Hata S, Kokudo N. Positive T lympho cytotoxic cross-match in living donor liver transplantation. Liver Transpl. 2003. 9:1062–1066.
28. Sugawara Y, Makuuchi M, Kaneko J, Saiura A, Imamura H, Kokudo N. Risk factors for acute rejection in living donor liver transplantation. Clin Transplant. 2003. 17:347–352.




 ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download