This article has been corrected. See "Erratum: Significance of defecographic parameters in diagnosing pelvic floor dyssynergia" in Volume 84 on page 377.
Abstract
Purpose
Defecography is known to be a sensitive and specific measurement of pelvic floor dyssynergia (PFD). However, its standardized parameter for diagnostic analysis is still incomplete. We attempted to determine which defecographic findings are most significant for PFD, and how closely they match other physiologic tests and clinical symptoms of functional pelvic outlet obstruction.
Methods
Ninety-six patients with constipation who completed work-up of their symptoms with defecography, anorectal manometry and electromyography (EMG) were included in the study. Internal consistency of defecographic findings, and agreements between defecographic findings and results of other tests were statistically analyzed (Crohnbach's α, Cohen's κ, respectively).
Results
Of the 96 patients evaluated, obstructive symptoms of constipation were obvious in 35 (36.5%) by obstructive symptom score. As known defecographic findings for PFD, poor opening of the anal canal was found in 33 (34.4%), persistent posterior angulation of the rectum in 33 (34.4%), and poor emptying of the rectum in 61 (63.5%). Manometric defecation index, manometric evacuation index, and EMG findings compatible with PFD were in 81 (84.4%), 72 (75%), and 73 (76%), respectively. Internal consistency of three defecographic findings was good (α = 0.78). Agreements between each defecographic findings and each result of other tests were all poor.
Conclusion
Among known defecographic findings for PFD, one specific finding cannot be considered more important than the others for its diagnosis. It is hard to expect consistent results of various diagnostic tests and to predict the presence of defecographic PFD by use of anorectal manometry, EMG, or even by clinical symptoms.
Chronic constipation is a symptom-based disorder of unsatisfactory defecation. Patients complain of mainly infrequent stools and/or difficult stool passage. There are two principal etiologies for such symptoms: delayed transit through the colon and impaired evacuation of the rectum. Impaired rectal evacuation can result from mechanical or structural obstruction, but the more common cause are functional pelvic outlet obstructions, which include paradoxical contraction or inadequate relaxation of pelvic floor muscle during defecation (pelvic floor dyssynergia, PFD) and failure to increase intrarectal pressure during evacuation [1,2].
Dynamic defecography is a fluoroscopic procedure used to observe rectal evacuation of contrast paste, in order to assess changing anatomic relationships of the pelvic floor and associated organs. Thus, it is particularly relevant in those patients who complain of difficult stool passage and usually performed to diagnose functional pelvic outlet obstruction. This test is generally known to be sensitive and specific for PFD, and recommended in situations when other anorectal physiologic test results differ from clinical impression [2-4]. However, even in defecography, standardized parameters for diagnostic analysis is still incomplete, and there are some controversies about what kind of defecographic finding is necessary for diagnosing PFD [5-7].
In this study, we tried to determine which defecographic findings are most significant for PFD, and how closely they match other physiologic tests such as anorectal manometry and electromyography (EMG), and how accurately they reflect clinical symptoms of constipation.
Among patients with chronic constipation who visited our colorectal clinic from March 2009 to April 2012, patients who completed work-up of their symptoms with dynamic defecography, anorectal manometry and EMG testing were included to the study. Chronic constipation was defined according to the Rome III criteria [8]. Patients with drug-induced or organic lesion-associated constipation were excluded. Ninety-six (mean age, 54 years; range, 17 to 83 years; female 72, male 24) constituted final study population.
Patients' data including dynamic video files of defecography were reviewed retrospectively. Patients' symptoms were evaluated by reviewing our own questionnaire sheet, which was routinely checked during initial interview. The questionnaire form was made with reference to the Wexner constipation scoring system [9], and the obstructed defecation syndrome score questionnaire [10]. Among the more than 10 items of our form, 5 items which were empirically believed related to obstructed defecation were selected and scored from 0 to 4 for stratifying the symptoms of pelvic outlet obstruction. The sum of all those points was termed as obstructive symptom score (OSS) with a maximum possible of 20 points (Table 1). When it was 16 or more, the patient was considered to have obvious obstructive symptoms of constipation.
Defecographic examination was done by radiologic technician. With patient in left lateral position, liquid barium of 50 mL was inserted first into the rectum using a catheter syringe. For female patients, the vaginal wall was coated with an appropriate amount of water-soluble contrast. Then, the barium paste, which was made with our own recipe (barium powder 180 mL, potato starch 90 mL, hot water 180 mL), was then inserted to the point where patients felt rectal filling and desire to defecate. Then the patient was asked to sit down on a specially designed commode and pose as usual for defecation. Dynamic image of fluoroscopy was then obtained while the patient was trying to evacuate the rectum. Defecographic findings of interest were those already known to be suggestive of PFD. They were: poor opening of the anal canal (PO), persistent posterior angulation of the rectum (PA), poor emptying of the rectum (PE). Anatomical changes such as rectocele (RE) and intussusception (IN) were also checked. PO was defined when the anal canal was not widened enough until 20 seconds after effective push action began. PA was defined when posterior wall of the rectum was not or poorly straightened with rectal tenesmus. PE was defined when zone of evacuation (a portion of the rectum below distal transverse fold) was not or poorly emptied until 40 seconds after the anal canal opened. Rectal tenesmus was defined effective when perineal descent and concave change of upper border of the rectum were noted. Anatomical changes were defined when there was obvious anterior bulging (RE), or funnel-shaped deformity (IN) of the rectum with rectal tenesmus. All these findings were observed only in dynamic image, not in static image.
Anorectal manometry was performed by nurse practitioner using a water-perfused catheter with eight channels attached to a hydraulic capillary infusion system (Medtronics, Minneapolis, MN, USA). The catheter was 4.5 mm in diameter with side-holes of 0.8 mm in diameter. Side-holes of each channel were spirally aligned with 7 mm-intervals along the longitudinal axis. Examination was performed in left lateral position without preparation. After calibration of systems, the catheter was inserted into the anal canal until the most distal side-hole was located at the anal verge. While the catheter was in position, simultaneous pressure measurements of the rectum and anal canal were done at squeeze and push with intervening resting stage. Rectal channels and anal channels were distinguished by pressure change during squeeze. Channels recording obvious pressure increase by squeeze were considered to be anal channels, and those proximal to them were considered rectal channels. Manometric defecation index (MDI) [11] was given by dividing maximum rectal pressure into minimum anal pressure during push. MDI was considered compatible for PFD when 1.2 or smaller. Manometric evacuation index (MEI) [12] was given by dividing evacuation pressure into pressure increase during squeeze. Evacuation pressure was herein defined as the pressure difference between the baseline resting pressure and the maximal relaxation or contraction during a given push effort with pressure variables measured at high-pressure zone of the anal canal. MEI was considered compatible with PFD when greater than 0.25.
EMG testing was done by nurse practitioner with patient in sitting position. An anal electrode of plug type was inserted into the anal canal and another electrode of surface type was attached to the abdominal wall. After patient's accommodation to the sensation of having a plug in the anal canal, EMG was recorded by system (HMT2000, HMT Inc., Seoul, Korea) at rest, squeeze, and push. EMG finding was considered compatible with PFD when reproducible increase of electrical activity was present while patient was attempting to push the plug out.
Statistical analysis was completed with SPSS ver. 17.0 (SPSS Inc., Chicago, IL, USA). Crohnbach's α test was used to define internal consistency of defecographic findings. Cohen's κ test was used to define agreements between each defecographic finding and each result of other tests, and agreements between results of other tests.
Obstructive symptoms of constipation were considered obvious by OSS in 35 patients (36.5%). For defecographic findings, PO was found in 33 (34.4%), PA was in 33 (34.4%), and PE was in 61 cases (63.5%). Patients with at least one of three findings totaled 64 (66.7%), and those with all three findings totaled 26 (27.1%). RE and IN were present in 61 (63.5%) and 37 patients (38.5%), respectively. As for findings of other physiologic tests, MDI, MEI and EMG pattern compatible with PFD were in 81 (84.4%), 72 (75%), and 73 cases (76%), respectively.
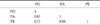
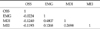
Internal consistency of three defecographic findings was generally good (α = 0.78), although consistency between PO and PA was highest (Table 2). Agreements between each defecographic finding and each result of other tests (OSS, MDI, MEI, EMG) were all poor, and agreements between simultaneous occurrence of all three defecographic findings and each result of other tests were also poor (Table 3). Agreements within results of other tests were moderate between MDI and EMG, but fair or poor between others (Table 4).
Chronic constipation is a symptom-based disorder of unsatisfactory defecation. Patients complain of mainly infrequent stools, difficult stool passage, or both. Except organic ones, etiologies of such symptoms are known to be colonic slow transit, pelvic outlet obstruction and irritable bowel syndrome (IBS) [1,2]. But IBS was classified separately in Rome criteria of functional constipation, and thus colonic slow transit and pelvic outlet obstruction could be deemed two major etiologies of chronic constipation.
Pelvic outlet obstruction can be either structural or functional [1]. Functional outlet obstruction is newly termed in Rome III criteria as functional defecation disorders, which include dyssynergic defecation and inadequate defecatory propulsion. Dyssynergic defecation is defined as inappropriate contraction of the pelvic floor or insufficient relaxation of the anal sphincter with adequate propulsive forces during attempted defecation. Inadequate defecatory propulsion is defined as inadequate propulsive forces with or without inappropriate contraction or insufficient relaxation of the anal sphincter during attempted defecation [8,13]. PFD was used previously as equivalent terminology to functional defecation disorders, without including the concept of inadequate defecatory propulsion. Strictly, it is equivalent to dyssynergic defecation in Rome III criteria.
Rome III criteria for diagnosing functional defecation disorders are as follows; 1) The patient must satisfy diagnostic criteria of functional constipation, and 2) During repeated attempts to defecate must have at least 2 of the following: (1) evidence of impaired evacuation, based on balloon expulsion or imaging, (2) inappropriate contraction of the pelvic floor muscles or less than 20% relaxation of basal resting sphincter pressure by manometry, imaging, or EMG, (3) inadequate propulsive forces assessed by manometry or imaging [8,13].
As shown above, usual tools for diagnosis of functional defecation disorders have been imaging, manometry and EMG, with recent addition of balloon expulsion test. Among them, defecography as imaging test has been considered to be a sensitive and specific measurement of PFD when it documents nonrelaxation of the puborectalis and the anal sphincter [3,4]. While balloon expulsion test, EMG, or anorectal manometry is usually chosen as a first-line test in diagnostic steps for PFD, defecography may be useful as a second-line test, especially when those tests are discrepant or differ from the clinical impression [2-4].
But defecography also has its own limitations. Contrast paste used in defecography is so different from typical condensed feces in patients with pelvic outlet obstruction that it may mislead to a different physiology of defecation. Particularly, such paste cannot always be a standardized commercial product, depending on the medico-social environment. Then, its consistency can vary enough to lead to a different physiology of defecation in certain cases. It is also well known that the reproducibility of measurement value is lacking, the concept of normal value is ambiguous, and standardized parameters for defecographic analysis are still incomplete. Besides, patient's feeling of embarrassment about being observed while defecating may lead to false positive findings.
Usual diagnostic findings of defecographic PFD are poor opening of the anal canal, persistent posterior angulation of the rectum, and/or poor emptying of the rectum. Traditionally, efforts to diagnose PFD have been focused on a patient's inappropriate puborectalis contaction during rectal evacuation. As the puborectalis cradles the anorectal junction, it has been suggested that a prominent muscular impression during evacuation, reflected by persistent posterior angulation of the rectum, is indicative of PFD. However, several studies have suggested that poor rectal emptying is more important in many of these patients and that this impairment may be more reliable in prediction of PFD than abnormal puborectalis configuration. They insisted that although the anorectal angle may sometimes reflect puborectalis tone, it is more often a secondary sign [6,7].
In our study, internal consistency of defecographic variables was calculated as good. Then, it is not pertinent to treat PO, PA, and PE separately in defecographic analysis. In other words, it is hard to say one of the above findings of defecography is more important than the others for the diagnosis of PFD. Moreover, individual agreements between each defecographic finding and each result of other tests were all poor. None of the defecographic findings were correlated to PFD-compatible findings in MDI, MEI or EMG. None of them agreed with clinical obstructive symptoms assessed by OSS. Even simultaneous occurrence of all three defecographic findings did not show better agreement with the results of other tests. Thus, it is hard to expect consistent results of various diagnostic tests for PFD.
Although defecography has often been considered as sensitive and specific for PFD, it is better to believe no single test is specific enough to confirm it, because other physiologic tests could also have their own measuring accuracy. In this sense, PFD should not depend on the results of a single test, but depend on the consistent results of 2 or more tests for its diagnosis. However, in another sense, those diagnostic tests for PFD including defecography may not be testing the same pathophysiologic condition, or the pathophysiology of PFD is much more complicated than generally accepted.
Based on this kind of interpretation, it was suggested that careful differentiation of testing results suggestive of PFD may actually lend itself to different forms of treatment [5]. Although theoretical, patients with poor rectal emptying on defecography, yet with normal EMG may have a rectal propulsion problem, rather than a relaxation problem, and thus may benefit from a laxative treatment. But patients with PFD-compatible EMG, irrespective of defecographic findings, could have more chance of improvement with biofeedback therapy. Further studies will elucidate issues about whether patients with PFD should be treated according to their individual patterns of testing abnormalities.
There are some problems or limitations in our study. First, the number of patients with abnormal findings in MDI, MEI, or EMG was high enough to suppose some errors in measuring technique, or interpreting method. But it does not seem possible, because agreement between MDI and EMG was moderate and it is very unusual for such errors to occur simultaneously in two different tests. In addition, the defecographic contrast paste used in our study was made using our own recipe at each time of examination. Although we tried to keep constancy in the making process, there could have been some errors in maintaining equable consistency of the paste. These can lead to different results under similar conditions.
In conclusion, internal consistency of defecographic variables was so good that it is not pertinent to treat PE, PO, and PA separately in defecographic analysis. Then, among known defecographic findings for PFD, one specific finding cannot be deemed more important than the others for its diagnosis. Individual agreements between each defecographic finding and each result of other tests were all poor. Thus, it is hard to expect consistent results of various diagnostic tests and to predict the presence of defecographic PFD by use of anorectal manometry, EMG, or even by clinical symptoms. Further studies will elucidate issues about whether patients with PFD should be treated according to their individual patterns of testing abnormalities.
Figures and Tables
Table 3
Agreement between defecography findings and results of other tests (Cohen's κ value)
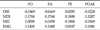
PO, poor opening of the anal canal; PA, persistent posterior angulation of the rectum; PE, poor emptying of the rectum; POAE, simultaneous occurrence of PO, PA, and PE; OSS, obstructive symptom score; MDI, manometric defecation index; MEI, manometric evacuation index.
Good, κ > 0.8; substantial, 0.8 ≥ κ > 0.6; moderate, 0.6 ≥ κ > 0.4; fair, 0.4 ≥ κ > 0.2; poor, 0.2 ≥ κ.
References
1. Birnbaum EH. Work-up of the constipated patient. Clin Colon Rectal Surg. 2008. 21:313–317.
2. Whitehead WE, Bharucha AE. Diagnosis and treatment of pelvic floor disorders: what's new and what to do. Gastroenterology. 2010. 138:1231–1235. 1235.e1–1235.e4.
3. Bove A, Pucciani F, Bellini M, Battaglia E, Bocchini R, Altomare DF, et al. Consensus statement AIGO/SICCR: diagnosis and treatment of chronic constipation and obstructed defecation (part I: diagnosis). World J Gastroenterol. 2012. 18:1555–1564.
4. Ternent CA, Bastawrous AL, Morin NA, Ellis CN, Hyman NH, Buie WD, et al. Practice parameters for the evaluation and management of constipation. Dis Colon Rectum. 2007. 50:2013–2022.
5. Bordeianou L, Savitt L, Dursun A. Measurements of pelvic floor dyssynergia: which test result matters? Dis Colon Rectum. 2011. 54:60–65.
6. Halligan S, Bartram CI, Park HJ, Kamm MA. Proctographic features of anismus. Radiology. 1995. 197:679–682.
7. Halligan S, Malouf A, Bartram CI, Marshall M, Hollings N, Kamm MA. Predictive value of impaired evacuation at proctography in diagnosing anismus. AJR Am J Roentgenol. 2001. 177:633–636.
8. Rome Foundation. Rome III disorders and criteria [Internet]. c2012. cited 2012 Sep 10. McLean: Rome Foundation;Available from: http://www.romecriteria.org/criteria.
9. Agachan F, Chen T, Pfeifer J, Reissman P, Wexner SD. A constipation scoring system to simplify evaluation and management of constipated patients. Dis Colon Rectum. 1996. 39:681–685.
10. Altomare DF, Spazzafumo L, Rinaldi M, Dodi G, Ghiselli R, Piloni V. Set-up and statistical validation of a new scoring system for obstructed defaecation syndrome. Colorectal Dis. 2008. 10:84–88.
11. Rao SS. Dyssynergic defecation. Gastroenterol Clin North Am. 2001. 30:97–114.
12. Ger GC, Wexner SD, Jorge JM, Salanga VD. Anorectal manometry in the diagnosis of paradoxical puborectalis syndrome. Dis Colon Rectum. 1993. 36:816–825.
13. Bharucha AE, Wald A, Enck P, Rao S. Functional anorectal disorders. Gastroenterology. 2006. 130:1510–1518.




 ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download