Abstract
Purpose
The aim of our study is to evaluate the factors affecting surgical margin positivity among patients with invasive ductal breast cancer who underwent breast-conserving surgery (BCS) after preoperative diagnostic core biopsy.
Methods
Two hundred sixteen patients with stage I, II invasive ductal breast carcinoma who had histological diagnosis with preoperative tru-cut biopsy and underwent BCS were included in the present study. Potential factors that affect the positive surgical margin were analyzed. In univariate analysis, the comparisons of the factors affecting the surgical margin positivity were made by chi-square test. Logistic regression test was used to detect the independent factors affecting the surgical margin positivity.
Results
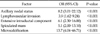
Positive axillary lymph node (odds ratio [OR], 8.2; 95% confidence interval [CI], 3.01 to 22.12), lymphovascular invasion (LVI; OR, 3.9; 95% CI, 1.62 to 9.24), extensive intraductal component (EIC; OR, 6.1; 95% CI, 2.30 to 16.00), presence of spiculation (OR, 5.1; 95% CI, 2.00 to 13.10) or presence of microcalcification in the mammography (OR, 13.7; 95% CI, 4.04 to 46.71) have been found to be the independent and adverse factors affecting surgical margin positivity.
The National Institute of Health (NIH) Consensus Conference in 1990 concluded that breast conservation surgery (BCS) was an appropriate method of treatment for women with early-stage breast cancers (stages I and II). BCS has been increasingly performed for patients with early breast cancer since the NIH Consensus Conference [1]. The objective of BCS is to completely remove the breast cancer and achieve negative surgical margins while maintaining the best possible breast cosmesis. Surgical margin positivity is the most important factor for local recurrence after BCS [2-4]. BCS after tru-cut biopsy is known to be more efficient in providing negative surgical margin compared with excisional biopsy [5-7]. We used tru-cut biopsy, except in special cases, as the primary histological diagnostic method in our clinic. The data on the factors associated with surgical margin positivity and BCS for invasive ductal cancer in the setting of preoperative tru-cut biopsy are limited [8]. The purpose of the present study is to evaluate the factors affecting surgical margin positivity among patients with invasive ductal breast cancer who underwent BCS after preoperative tru-cut biopsy.
Two hundred sixteen patients with stage I, II invasive ductal breast carcinoma who had histological diagnosis with preoperative tru-cut biopsy and underwent BCS at the Department of General Surgery in Ondokuz Mayis University School of Medicine between January 2004 and September 2012 were the subject of this retrospective study. All patients underwent sentinel lymph node biopsy with isosulphane blue and patients with metastatic sentinel lymph node biopsy underwent level I, II axillary node dissection. Injectable sterile solutions of 1% isosulphane blue (monosodium salt of 2,5-disulphonated triphenyl methane) was prepared by the Department of Pharmaceutical Technology at Istanbul University Faculty of Pharmacy using a stock solution obtained from Sigma company (5 g isosulphan blue, Sigma catalog No: P1888, Sigma-Aldrich chemical Co., Deisenhofen, Germany). The findings of mammography, and breast ultrasonography, and pathological examination have been recorded. Information regarding surgical margin positivity (negative, positive), age (≤40, >40), tumor size (≤2 cm, >2 cm), tumor grade (1, 2, 3), presence of lymphovascular invasion (LVI), presence of extensive intraductal component (EIC), axillary lymph node status (negative, positive), estrogen receptor (ER) status, progesterone receptor (PR) status, human endothelial growth factor receptor 2 (Her-2) status, molecular subtypes (luminal A, luminal B, Her-2 (+), triple negative), multifocality (present, absent), tumor location in breast quadrants (upper outer, upper inner, lower outer, lower inner, central), mammographic lation or the presence of microcalcification in the mammography have been recorded and analyzed (Table 1). Positive ER and PR status was defined as ≥5% of tumor cell nuclei showing specific staining. Specific membrane staining for c-erbB2 (Her-2/neu) was reported as positive, with the intensity of the staining observed on a scale of 0-3. Intensity of 0 to 1+ was considered negative, whereas 3+ staining was considered positive. An intermediate score of 2+ was confirmed by fluorescence in situ hybridization amplification [9]. Tumors with ER and/or PR positive and Her-2 negative were classified as luminal A, tumors with ER and/or PR positive and Her-2 positive as luminal B, tumors with ER and PR negative and Her-2 positive as Her-2 (+), and tumors with ER and PR negative and Her-2 negative as triple negative molecular subtype. We staged the patients using the tumor-node-metastasis stage according to the 7th American Joint Committee on Cancer system [10].
We generally used curvilinear incisions, though radial incisions were sometimes used for tumors located at the three or nine o'clock positions. To achieve a clear surgical margin, we attempted to obtain a margin of 1 cm of grossly normal breast tissue around the tumor. A skin island overlying the tumor was also excised for very superficial tumors. All the breast tissue under subcutaneous fat tissue was removed for tumors located close to the breast skin. Underlying breast tissue down to the pectoralis major muscle including the fascia of the muscle was excised for tumors located deep in the breast. Nipple-areola complex (NAC) was removed for tumors located at the central quadrant in case the tumor was close to or invaded the NAC. Preoperative localization of 16 nonpalpable tumors was performed by wire localization, and specimen radiography was performed for these tumors. Breast magnetic resonance imaging was not used as routinely, but was used for the evaluation of the suspected lesions found on mammography or ultrasonography in 7 patients. Intraoperative margin excision and frozen section analysis were performed for intraoperative margin assessment in 13 patients for whom the breast surgeon suspected margin positivity during the surgery. The presence of tumor cells at or closer than 1 mm to the inked margins was accepted as positive surgical margin. Variables to be analyzed have been recorded into the computer by using the SPSS ver. 15.0 (SPSS Inc., Chicago, IL, USA). The categorical data have been identified numerically and by percentage. In univariate analysis, the comparisons of the factors affecting surgical margin positivity were made by chi-square test. Logistic regression test was used to detect independent factors affecting surgical margin positivity, and the odds ratios (ORs), and 95% confidence interval (CI) were calculated. P < 0.05 has been accepted as significance level.
General characteristics of the patients have been given in Table 1. The median age of the patients was 50 (range, 27 to 82). Ninety-six patients were stage IA (45%), 2 were stage IB (1%), 67 (31%) were stage IIA, 37 (17%) were stage IIB, 11 were stage IIIA (5%), and 3 were stage IIIC (1%). Positive surgical margin was detected in 58 patients (27%). Ten patients with positive surgical margin had mastectomy (17%), and 48 (83%) had re-excisions as the second surgery. At the end of the second surgeries, of the 4 patients that had persistent positive surgical margin, two had re-excision and the other two had mastectomy.
In the univariate analysis (Table 1), tumor size (P = 0.002), positive axillary lymph node (P < 0.001), LVI (P < 0.001), EIC (P < 0.001), presence of spiculation in the mammography (P < 0.001) and presence of microcalcification in the mammography (P < 0.001) were found to be significantly associated with positive surgical margin. In multivariate analysis (Table 2), positive axillary lymph node (OR, 8.2; 95% CI, 3.01 to 22.12), LVI (OR, 3.9; 95% CI, 1.62 to 9.24), EIC (OR, 6.1; 95% CI, 2.30 to 16.00), presence of spiculation in the mammography (OR, 5.1; 95% CI, 2.00 to 13.10), and presence of microcalcification in the mammography (OR, 13.7; 95% CI, 4.04 to 46.71) were found to be the independent and adverse factors affecting surgical margin positivity.
The objective with patients having BCS is to provide a clean surgical margin with acceptable breast cosmetics. There is still no consensus regarding the definition of clean surgical margin. Eleven percent of the surgeons attending a study presented by Azu et al. [11] has defined clear surgical margin as the inexistence of tumor cells in the painted margin, 42% defined it as 1-2 mm, 28% as ≥5 mm, and 19% as ≥10 mm. We have accepted clear surgical margin as the inexistence of tumor cells at or closer than 1 mm to the inked margin.
The findings of our study revealed that metastatic axillary lymph nodes, LVI, EIC, spiculated mass or microcalcifications in mammography were associated with positive surgical margin after BCS. Young age [12-14], high grade [15], and high density of the breast [16] have been reported as factors affecting positive surgical margin after BCS. Contrary to these studies, in some studies it has been shown that young age [17,18] and grade [6,19] do not have any influence on surgical margin positivity. These factors have also been found not significant in the present study. In studies where the tumor size was analyzed, it has been reported that it affected surgical margin positivity [20,21]. In the present study; while the tumor size was important in univariate analysis, in multivariate analysis it lost significance. EIC [22-24] and LVI [3,22] were reported as significant factors associated with positive surgical margin in parallel with our study. Park et al. [25] have detected that patients who had 4 or more metastatic axillary lymph nodes had more positive surgical margins. In our study, we have found that metastatic axillary lymph node affected positive surgical margin significantly.
There are just a few studies analyzing the affect of the molecular subtypes of breast cancer on surgical margin positivity among patients who underwent BCS. Our findings do not agree with the study by Sioshansi et al. [9] who reported that triple negative breast cancer is associated with an increased risk of residual invasive carcinoma after lumpectomy. Atalay and Irkkan [26] have demonstrated that the presence of tumor in re-excision following BCS is significantly higher in patients with Her-2 (+) subgroup. However, Sioshani et al. [9] and Atalay et al. [26] analyzed the association of molecular subtypes with residual carcinoma, and with re-excision after lumpectomy, respectively, whereas we analyzed the association of subtypes with positive surgical margins.
Preoperative mammography could also have been used for decision making for the extent of excision in patients who are candidates for BCS. We agree with many studies that showed that the presence of microcalcification in mammography was an adverse factor affecting positive margin [27-29]. In our study, we have found that surgical margin positivity was significantly higher in patients who had a spicular appearance in mammography. However, a spiculated mass, which had been analyzed in only two studies, was not found to affect positive surgical margin [20,30].
Our findings support the findings of the study by Sioshansi et al. [9] who showed that multifocality is not significantly associated with an increased risk of residual invasive breast carcinoma, but contrast with the studies reporting that multifocality was as an adverse factor affecting positive surgical margin [21,27,29]. However, the number of patients with multifocality is very low in our series (3%); therefore, although surgical margin positivity is higher in patients with multifocal disease compared with those without multifocality (44% vs. 26%), this is not significant. Our study could lack the ability to show a difference at this level. Tumor location in breast quadrants was not found to be predictive of positive margins in our series as suggested by previous studies [6,30].
A limited study, found in the literature, analysed the factors affecting positive surgical margin among invasive breast cancer patients who had preoperative core or fine-needle biopsy was performed by Smitt and Horst [8]. In that study they reported that only lobular histology and LVI were significantly related with positive surgical margin among 67 invasive breast cancer patients who underwent preoperative diagnostic biopsy [8].
Consequently, metastatic axillary lymph nodes, EIC, LVI, presence of spiculation or presence of microcalcification in mammography have been found as the independent and adverse factors affecting positive surgical margin.
By using the factors affecting positive surgical margin, while communicating with the patient, we can describe more realistically the risks of the margin positivity thereby helping the patient understand better. We could also benefit from these factors for defining the extent of the excision size, and we could provide a clear surgical margin with fewer surgeries and reduce the treatment costs and morbidity.
References
1. National Institutes of Health Consensus Development Panel. Consensus statement: treatment of early-stage breast cancer. J Natl Cancer Inst Monogr. 1992. (11):1–5.
2. Klimberg VS, Harms S, Korourian S. Assessing margin status. Surg Oncol. 1999. 8:77–84.
3. Singletary SE. Surgical margins in patients with early-stage breast cancer treated with breast conservation therapy. Am J Surg. 2002. 184:383–393.
4. Peterson ME, Schultz DJ, Reynolds C, Solin LJ. Outcomes in breast cancer patients relative to margin status after treatment with breast-conserving surgery and radiation therapy: the University of Pennsylvania experience. Int J Radiat Oncol Biol Phys. 1999. 43:1029–1035.
5. White RR, Halperin TJ, Olson JA Jr, Soo MS, Bentley RC, Seigler HF. Impact of core-needle breast biopsy on the surgical management of mammographic abnormalities. Ann Surg. 2001. 233:769–777.
6. Waljee JF, Hu ES, Newman LA, Alderman AK. Predictors of re-excision among women undergoing breast-conserving surgery for cancer. Ann Surg Oncol. 2008. 15:1297–1303.
7. Staradub VL, Rademaker AW, Morrow M. Factors influencing outcomes for breast conservation therapy of mammographically detected malignancies. J Am Coll Surg. 2003. 196:518–524.
8. Smitt MC, Horst K. Association of clinical and pathologic variables with lumpectomy surgical margin status after preoperative diagnosis or excisional biopsy of invasive breast cancer. Ann Surg Oncol. 2007. 14:1040–1044.
9. Sioshansi S, Ehdaivand S, Cramer C, Lomme MM, Price LL, Wazer DE. Triple negative breast cancer is associated with an increased risk of residual invasive carcinoma after lumpectomy. Cancer. 2012. 118:3893–3898.
10. Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A. AJCC cancer staging manual. 2010. 7th ed. New York: Springer.
11. Azu M, Abrahamse P, Katz SJ, Jagsi R, Morrow M. What is an adequate margin for breast-conserving surgery? Surgeon attitudes and correlates. Ann Surg Oncol. 2010. 17:558–563.
12. Lovrics PJ, Cornacchi SD, Farrokhyar F, Garnett A, Chen V, Franic S, et al. Technical factors, surgeon case volume and positive margin rates after breast conservation surgery for early-stage breast cancer. Can J Surg. 2010. 53:305–312.
13. DiBiase SJ, Komarnicky LT, Schwartz GF, Xie Y, Mansfield CM. The number of positive margins influences the outcome of women treated with breast preservation for early stage breast carcinoma. Cancer. 1998. 82:2212–2220.
14. Mirza NQ, Vlastos G, Meric F, Buchholz TA, Esnaola N, Singletary SE, et al. Predictors of locoregional recurrence among patients with early-stage breast cancer treated with breast-conserving therapy. Ann Surg Oncol. 2002. 9:256–265.
15. Cellini C, Hollenbeck ST, Christos P, Martins D, Carson J, Kemper S, et al. Factors associated with residual breast cancer after re-excision for close or positive margins. Ann Surg Oncol. 2004. 11:915–920.
16. Bani MR, Lux MP, Heusinger K, Wenkel E, Magener A, Schulz-Wendtland R, et al. Factors correlating with reexcision after breast-conserving therapy. Eur J Surg Oncol. 2009. 35:32–37.
17. Keskek M, Kothari M, Ardehali B, Betambeau N, Nasiri N, Gui GP. Factors predisposing to cavity margin positivity following conservation surgery for breast cancer. Eur J Surg Oncol. 2004. 30:1058–1064.
18. Chagpar AB, Martin RC 2nd, Hagendoorn LJ, Chao C, McMasters KM. Lumpectomy margins are affected by tumor size and histologic subtype but not by biopsy technique. Am J Surg. 2004. 188:399–402.
19. Sabel MS, Rogers K, Griffith K, Jagsi R, Kleer CG, Diehl KA, et al. Residual disease after re-excision lumpectomy for close margins. J Surg Oncol. 2009. 99:99–103.
20. Dillon MF, Hill AD, Fleming FJ, O'Doherty A, Quinn CM, McDermott EW, et al. Identifying patients at risk of compromised margins following breast conservation for lobular carcinoma. Am J Surg. 2006. 191:201–205.
21. Cabioglu N, Hunt KK, Sahin AA, Kuerer HM, Babiera GV, Singletary SE, et al. Role for intraoperative margin assessment in patients undergoing breast-conserving surgery. Ann Surg Oncol. 2007. 14:1458–1471.
22. American College of Radiology. Practice guideline for the breast conservation therapy in the management of invasive breast carcinoma. J Am Coll Surg. 2007. 205:362–376.
23. Newman LA, Washington TA. New trends in breast conservation therapy. Surg Clin North Am. 2003. 83:841–883.
24. Smitt MC, Nowels K, Carlson RW, Jeffrey SS. Predictors of reexcision findings and recurrence after breast conservation. Int J Radiat Oncol Biol Phys. 2003. 57:979–985.
25. Park S, Park HS, Kim SI, Koo JS, Park BW, Lee KS. The impact of a focally positive resection margin on the local control in patients treated with breast-conserving therapy. Jpn J Clin Oncol. 2011. 41:600–608.
26. Atalay C, Irkkan C. Predictive factors for residual disease in re-excision specimens after breast-conserving surgery. Breast J. 2012. 18:339–344.
27. Ramanah R, Pivot X, Sautiere JL, Maillet R, Riethmuller D. Predictors of re-excision for positive or close margins in breast-conservation therapy for pT1 tumors. Am J Surg. 2008. 195:770–774.
28. Walls J, Knox F, Baildam AD, Asbury DL, Mansel RE, Bundred NJ. Can preoperative factors predict for residual malignancy after breast biopsy for invasive cancer? Ann R Coll Surg Engl. 1995. 77:248–251.
29. Kurniawan ED, Wong MH, Windle I, Rose A, Mou A, Buchanan M, et al. Predictors of surgical margin status in breast-conserving surgery within a breast screening program. Ann Surg Oncol. 2008. 15:2542–2549.
30. Moore MM, Borossa G, Imbrie JZ, Fechner RE, Harvey JA, Slingluff CL Jr, et al. Association of infiltrating lobular carcinoma with positive surgical margins after breast-conservation therapy. Ann Surg. 2000. 231:877–882.




 ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download