Abstract
Purpose
The preoperative prediction of malignant potential in patients with gastric submucosal tumors (SMTs) plays an important role in decisions regarding their surgical management.
Methods
We evaluated the predictors of malignant gastric SMTs in 314 patients with gastric SMTs who underwent surgery in Chonnam National University Hospital.
Results
The malignant SMTs were significantly associated with age (odds ratio [OR], 1.067; 95% confidence interval [CI], 1.042 to 1.091; P < 0.0001), presence of central ulceration (OR, 2.690; 95% CI, 1.224 to 5.909; P = 0.014), and tumor size (OR, 1.791; 95% CI, 1.483 to 2.164; P < 0.0001). Receiver operating characteristic curve analysis showed that tumor size was a good predictor of malignant potential. The most relevant predictor of malignant gastric SMT was tumor size with cut-offs of 4.05 and 6.40 cm.
Conclusion
Our findings indicated that age, central ulceration, and tumor size were significant preoperative predictors of malignant SMTs. We suggest that 4 cm be selected as a threshold value for malignant gastric SMTs. In patients with a gastric SMT larger than 4 cm with ulceration, wide resection of the full thickness of the gastric wall or gastrectomy with adequate margins should be performed because of its malignant potential.
Gastric submucosal tumors (SMTs) account for less than 2% of all neoplasms of the stomach and stromal tumors are the most common tumors of the gastric submucosa [1,2]. Most SMTs are asymptomatic and benign, but 15 to 30% are malignant [3,4]. Endoscopic ultrasonography (EUS) is widely used following endoscopy for the evaluation of SMTs, but EUS is not yet reliable enough to differentiate between benign and malignant SMTs. Brand et al. [5] reported a sensitivity of 95% and a specificity of 72% for diagnosing gastrointestinal stromal tumors, while Oguz et al. [6] reported a sensitivity of 50% and specificity of 72% for diagnosing gastrointestinal SMTs. More than 30% of the patients with malignant tumors develop local recurrence and distant metastases [7]. Therefore, the preoperative prediction of malignant potential in patients with gastric SMTs plays an important role in the decision regarding surgical management. This study examined the preoperative predictors of malignant gastric SMTs.
From January 2004 to December 2009, 314 patients (151 males, 163 females) with suspected SMT of the stomach underwent surgery in Chonnam National University Hospital, Gwangju, Korea. Patient information was gathered from the hospital records retrospectively. Eleven variables were evaluated for each patient: patient age and gender, the use of EUS, pre- and postoperative diagnosis, tumor growth pattern, exploration method, type of operation, presence of central ulceration, and tumor location and size. To establish the diagnosis and determine the extent of the disease, all patients underwent a preoperative work-up including esophagogastroduodenoscopy, EUS, and computed tomography (CT). We classified the patients into malignant potential and benign groups. The aggressive risk was defined according to the size and mitotic rate of the tumors, as proposed by Fletcher et al. [8]. We evaluated the accuracy of the preoperative diagnosis and the sensitivity and specificity of the preoperative diagnosis in all cases. Furthermore, we compared the sensitivity and specificity of diagnosis with and without performing EUS.
The operative indications included a SMT > 20 mm in size and definitely visible by endoscopy, irrespective of symptoms. Tumors < 20 mm in size measured on EUS or CT were observed or a gastrectomy was performed when the patient requested surgery because of concern. Laparoscopic resection and local excision were performed using three methods: extragastric wedge resection was performed for SMTs with an exophytic growth pattern; transgastric resection was performed for endophytic SMTs; and intragastric resection was performed for SMTs located at the esophagogastric junction. Intraoperative gastroscopy was used to identify and mark small tumors and to ensure that the tumor was excised with an adequate margin. Conventional open surgery was performed via an upper midline laparotomy.
To identify significant independent correlates of overall and malignant risk, a stepwise procedure was applied for selected factors with P < 0.05 in order to identify independent potent risk factors. A multiple logistic model was applied to evaluate the odds ratios of the major risk factors. Statistical analyses were conducted using PASW ver. 18.0 (IBM Co., Armonk, NY, USA).
Table 1 shows the clinicopathological features of the patients with gastric SMTs. In total, 314 patients with a SMT in the stomach underwent surgery. Of the patients, 151 (48.1%) were male and 163 (51.9%) were female. The mean age was 53.3 years and the mean tumor size was 3.6 ± 2.5 cm in maximum diameter (range, 0.6 to 20.0 cm). The growth pattern was endophytic in 207 cases (65.9%) and exophytic in 107 cases (34.1%). The lesions were located in the upper one third in 173 (55.1%) patients including the esophagogastric junction, in the middle third in 61 (19.4%) patients, and in the lower one third in 80 (25.5%) patients. Fifty-six tumors (17.8%) were ulcerated. Wedge resection was the procedure carried out most frequently in patients with gastric SMTs. The preferred procedure was laparoscopic surgery.
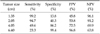
The sensitivity, specificity, and negative and positive predictive values of diagnosis without EUS for malignant SMT were 93.8, 35.1, 71.7, and 76.4%, respectively. The cases diagnosed with EUS had respective values of 88.0, 46.7, 39.3, and 90.9% for potential malignancy (Table 2).
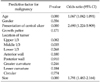
Multivariate analysis of the predictors of malignant SMTs is summarized in Table 3. The malignant SMTs were significantly associated with age (odds ratio [OR], 1.067; 95% confidence interval [CI], 1.042 to 1.091; P < 0.0001), the presence of central ulceration (OR, 2.690; 95% CI, 1.224 to 5.909; P = 0.014), and tumor size (OR, 1.791; 95% CI, 1.483 to 2.164 for a 1-cm increase; P < 0.0001). No relationship between the other factors (gender, growth pattern, tumor location) and malignant potential was found.
The receiver operating characteristic (ROC) curve analysis showed that tumor size was a good predictor of malignant potential (Fig. 1). The area under the ROC curve was 0.772 ± 0.026 (95% CI, 0.721 to 0.823). The diagnostic performance of malignant potential was further analyzed using two cut-off values: a lower value to improve sensitivity and a higher value to improve specificity. Table 4 shows the different threshold values, and the most relevant ones for malignant SMT prediction were 4.05 and 6.40 cm. A cut-off value of 4.05 cm gave a sensitivity of 49.6%, specificity of 86.2%, positive predictive value of 72.5%, and negative predictive value of 69.9%. When the cut-off value was increased to 6.40 cm, the specificity reached 99.4% and the positive predictive value 96.8%.
The surgical principles for managing SMTs include laparoscopic resection for small tumors and avoidance of tumor rupture, wedge resection, and complete resection of gross disease and adherent organs [9-12]. A wide resection of the full thickness of the gastric wall with adequate margins is a satisfactory procedure for malignant gastric SMTs, while mass enucleation may be sufficient for benign gastric SMTs [12,13]. The preoperative prediction of malignant potential in patients with gastric SMTs plays an important role in deciding on the operative method. However, it is difficult to diagnose whether a tumor is malignant preoperatively; the definitive diagnosis of gastric SMTs is possible only with pathological confirmation.
EUS is used widely in the evaluation of gastric SMTs. Unfortunately, EUS is not yet reliable enough for differentiating between benign and malignant SMTs. Palazzo et al. [14] reported that the three most predictive EUS features for malignancy were irregular margins, cystic spaces, and lymph nodes with a malignant pattern. They found that the presence of at least one of these criteria had a sensitivity of 91%, specificity of 88%, positive predictive value of 83%, and negative predictive value of 94% for potential malignancy. We found that EUS has a high diagnostic sensitivity for the malignant potential of SMT, in agreement with previous studies [8,9,14]. However, EUS had a low specificity and positive predictive value for the diagnosis of malignant SMTs in our study. Therefore, we need better preoperative predictors for malignant SMTs to establish the surgical plan.
In this study, three factors predicted malignant SMTs in the multivariate analysis. The first was age. Rabin et al. [15] found a significant correlation between age and malignant potential and reported that the younger the patient, the higher the incidence of malignancy. Contrary to their results, the mean age was higher in the malignant group in our series. No similar data regarding age as a predictor of malignant SMTs were found when reviewing other reports.
Second, mucosal ulceration is a common feature of gastric SMTs. Miettinen et al. [16] reported that the presence of ulceration has no predictive value or prognostic significance, although it may be related to tumor size. In another study, Miettinen et al. [17] demonstrated that ulceration was common in all histologic subtypes but, nevertheless, was an adverse prognostic factor, probably because of its consistent presence in malignant SMTs. In contrast to their result, we found that tumor ulceration predicted malignant SMTs.
Third, tumor size was another predictor of malignant SMTs in our series. Tumor size is an easily applicable morphologic criterion for predicting tumor behavior. In some studies, tumor size > 6 cm has been suggested as a threshold value for malignancy [18,19]. Miettinen et al. [17] suggested that 5 cm was a threshold value for malignant SMTs, despite an unpredictable, but low, frequency of unexpected progressive disease among patients with relatively small tumors and low mitotic activity, although this frequency does not exceed 2 to 3%. Hsu et al. [20] also reported that tumor size ≥ 10 cm carried both a higher risk of recurrence and worse survival in SMTs. We used ROC curves to determine the optimal cut-off value for size to distinguish malignant and benign tumors. Examining different threshold values, the most relevant for malignant SMTs prediction were 4.05 and 6.40 cm. A cut-off value of 4.05 cm had a sensitivity of 49.6%, specificity of 86.2%, positive predictive value of 72.5%, and negative predictive value of 69.9%. When the cut-off value was increased to 6.40 cm, the specificity reached 99.4% and the positive predictive value was 96.8%. We propose 4 cm as the threshold value.
In conclusion, malignant SMTs were significantly associated with age, the presence of central ulceration, and tumor size. We suggest that a tumor size of 4 cm be selected as the threshold value for malignant SMTs. If an ulcerated SMT is bigger than 4 cm, we recommend a wide wedge resection of the full thickness of the gastric wall, or gastrectomy with adequate margins, because it has high potential for malignancy.
Figures and Tables
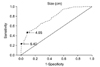 | Fig. 1The receiver operating characteristic curve of tumor size for predicting malignant gastric submucosal tumors. |
Table 2
Sensitivity, specificity, PPV, and NPV of the diagnosis of malignant submucosal tumor (exclusion criterion: preoperative diagnosis not described, n = 63)

References
1. Campbell F, Bogomoletz WV, Williams GT. Fletcher CD, editor. Tumours of the oesophagus and stomach. Diagnostic histopathology of tumours. 1995. London: Churchill Livingstone;193–242.
2. Kempson RL, Hendrickson MR. Whitehead R, editor. Gastrointestinal stromal (smooth muscle) tumours. Gastrointestinal and oesophageal pathology. 1995. 2nd ed. Edinburgh: Churchill Livingstone;727–739.
3. Chak A. EUS in submucosal tumors. Gastrointest Endosc. 2002. 56:4 Suppl. S43–S48.
4. Connolly EM, Gaffney E, Reynolds JV. Gastrointestinal stromal tumours. Br J Surg. 2003. 90:1178–1186.
5. Brand B, Oesterhelweg L, Binmoeller KF, Sriram PV, Bohnacker S, Seewald S, et al. Impact of endoscopic ultrasound for evaluation of submucosal lesions in gastrointestinal tract. Dig Liver Dis. 2002. 34:290–297.
6. Oguz D, Filik L, Parlak E, Disibeyaz S, Cicek B, Kacar S, et al. Accuracy of endoscopic ultrasonography in upper gastrointestinal submucosal lesions. Turk J Gastroenterol. 2004. 15:82–85.
7. Krajinovic K, Germer CT, Agaimy A, Wunsch PH, Isbert C. Outcome after resection of one hundred gastrointestinal stromal tumors. Dig Surg. 2010. 27:313–319.
8. Fletcher CD, Berman JJ, Corless C, Gorstein F, Lasota J, Longley BJ, et al. Diagnosis of gastrointestinal stromal tumors: a consensus approach. Hum Pathol. 2002. 33:459–465.
9. Samelis GF, Ekmektzoglou KA, Zografos GC. Gastrointestinal stromal tumours: clinical overview, surgery and recent advances in imatinib mesylate therapy. Eur J Surg Oncol. 2007. 33:942–950.
10. Sasaki A, Koeda K, Nakajima J, Obuchi T, Baba S, Wakabayashi G. Single-incision laparoscopic gastric resection for submucosal tumors: report of three cases. Surg Today. 2011. 41:133–136.
11. Eisenberg BL, Judson I. Surgery and imatinib in the management of GIST: emerging approaches to adjuvant and neoadjuvant therapy. Ann Surg Oncol. 2004. 11:465–475.
12. Singaporewalla RM, Baladas GH, Lee TD. Laparoendoscopic removal of a benign gastric stromal tumor at the cardia. JSLS. 2006. 10:117–121.
13. Silberhumer GR, Hufschmid M, Wrba F, Gyoeri G, Schoppmann S, Tribl B, et al. Surgery for gastrointestinal stromal tumors of the stomach. J Gastrointest Surg. 2009. 13:1213–1219.
14. Palazzo L, Landi B, Cellier C, Cuillerier E, Roseau G, Barbier JP. Endosonographic features predictive of benign and malignant gastrointestinal stromal cell tumours. Gut. 2000. 46:88–92.
15. Rabin I, Chikman B, Lavy R, Sandbank J, Maklakovsky M, Gold-Deutch R, et al. Gastrointestinal stromal tumors: a 19 year experience. Isr Med Assoc J. 2009. 11:98–102.
16. Miettinen M, El-Rifai W, Sobin HL, Lasota J. Evaluation of malignancy and prognosis of gastrointestinal stromal tumors: a review. Hum Pathol. 2002. 33:478–483.
17. Miettinen M, Sobin LH, Lasota J. Gastrointestinal stromal tumors of the stomach: a clinicopathologic, immunohistochemical, and molecular genetic study of 1765 cases with long-term follow-up. Am J Surg Pathol. 2005. 29:52–68.
18. Appleman HD, Helwig EB. Gastric epithelioid leiomyoma and leiomyosarcoma (leiomyoblastoma). Cancer. 1976. 38:708–728.
19. Wong NA, Young R, Malcomson RD, Nayar AG, Jamieson LA, Save VE, et al. Prognostic indicators for gastrointestinal stromal tumours: a clinicopathological and immunohistochemical study of 108 resected cases of the stomach. Histopathology. 2003. 43:118–126.
20. Hsu KH, Yang TM, Shan YS, Lin PW. Tumor size is a major determinant of recurrence in patients with resectable gastrointestinal stromal tumor. Am J Surg. 2007. 194:148–152.




 ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download