Abstract
Purpose
Treatment for esophageal atresia has advanced over several decades due to improvements in surgical techniques and neonatal intensive care. Subsequent to increased survival, postoperative morbidity has become an important issue in this disease. The aim of our study was to analyze our experience regarding the treatment of esophageal atresia.
Methods
We reviewed and analyzed the clinical data of patients who underwent surgery for esophageal atresia at Severance Children's Hospital from 1995 to 2010 regarding demographics, surgical procedures, and postoperative outcomes.
Results
Seventy-two patients had surgery for esophageal atresia. The most common gross type was C (81.9%), followed by type A (15.3%). Primary repair was performed in 52 patients. Staged operation was performed in 17 patients. Postoperative esophageal strictures developed in 43.1% of patients. Anastomotic leakages occurred in 23.6% of patients, and recurrence of tracheoesophageal fistula was reported in 8.3% of patients. Esophageal stricture was significantly associated with long-gap (≥3 cm or three vertebral bodies) atresia (P = 0.042). The overall mortality rate was 15.3%. The mortality in patients weighing less than 2.5 kg was higher than in patients weighing at least 2.5 kg (P = 0.001). During the later period of this study, anastomotic leakage and mortality both significantly decreased compared to the earlier study period (P = 0.009 and 0.023, respectively).
Esophageal atresia is one of the most significant congenital diseases in pediatric surgery, requiring prompt surgical treatment for optimal outcome in that its outcomes are mainly dependent on the surgery. Since the first successful repair in 1941 [1], treatments for esophageal atresia have gradually evolved due to not only better preoperative and postoperative neonatal intensive care but also the application of meticulous and precise surgical techniques [2]. Recently, the mortality rate associated with esophageal atresia was reported to be less than 10%, and high-risk neonates now have a better prognosis [3].
However, esophageal atresia is still a difficult disease for the pediatric surgeon who may not have sufficient experience. Postoperative complications such as anastomotic leakage and stricture are common, and occasionally, recurrence of tracheoesophageal fistula (TEF) occurs. Additionally, gastroesophageal reflux (GER) and esophageal dysmotility are often observed during long-term follow-up. These issues are currently under investigation [3].
In this study, we reviewed our experience regarding the treatment of esophageal atresia with or without TEF. As one of the large studies of esophageal atresia in Korea, our results may well contribute to improvements in treatment outcomes for esophageal atresia.
We performed a retrospective review of the clinical data of patients who were treated for esophageal atresia at Severance Children's Hospital from January 1995 to December 2010. Cases prior to 1995 could not be included because of the incompleteness of the data. Overall, 107 patients were treated during the study period. Among them, 29 patients were excluded from the study because they did not undergo primary surgery at Severance Children's Hospital; instead, they were transferred from other hospitals after complication from the primary surgery. We also excluded six patients from the study because four patients were discharged against medical advice before surgery and two, who had severe multiple congenital anomalies, died immediately after birth.
We analyzed the data of 72 patients. The following data were collected: patient demographics including combined anomalies and types of esophageal atresia, diagnostic tools, methods of surgical procedures, and treatment outcomes.
Statistical analyses were performed using IBM SPSS ver. 18.0 (IBM Co., Armonk, NY, USA). Two-sample t-tests and chi-square tests were used to analyze the data, with P-values less than 0.05 considered significant.
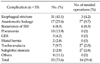
Patient characteristics are shown in Table 1. Fifty patients (69.4%) had combined anomalies, and VACTERL association with two or more anomalies was identified in 14 patients (19.4%). Among the combined anomalies, cardiac anomalies were most common (43 patients, 59.7%), and 12 patients (16.7%) had major cardiac anomalies that required surgery.
The most common gross type of esophageal atresia was C (59 patients, 81.9%), followed by types A (11 patients, 15.3%) and E (H-type, 2 patients, 2.8%). The other types were not found in our data.
All patients with types A and C esophageal atresia were diagnosed by the identification of a coiled gavage tube by chest radiography. Two cases of H-type TEF were diagnosed by contrast esophagography. In 17 cases (23.6%), chest computed tomography (CT) was performed to evaluate the anatomy of the TEF and to measure the distance between the proximal and distal esophagus.
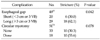
The surgical methods are summarized in Table 2. Most patients with type C esophageal atresia underwent repair by primary surgery (mean age, 3.9 ± 2.2 days), but seven underwent staged operations due to severe combined anomalies (4 patients) and long-gap atresia (3 patients). One of four patients with severe combined anomalies did not undergo definite surgery after gastrostomy because the parents declined further treatment early in the study. Three of four patients with severe combined anomalies were performed only gastrostomy in the first operation. Three patients with long-gap atresia underwent fistula ligation, gastrostomy, and cervical esophagostomy in the first operation.
All patients with type A esophageal atresia underwent staged operations, which included esophago-esophagostomy after elongation of the proximal and distal esophagus by several bouginations, adopted by the authors in 2004 [4].
In 53 patients (73.6%), postoperative complications developed (Table 3). The most common complication was esophageal strictures that were mostly treated by esophageal balloon dilatation or bougination. However, in three cases, segmental resection of esophageal stricture and end-to-end anastomosis were performed. We were able to obtain data on the esophageal gap (distance between the proximal and distal esophageal end) in 49 patients and on circular myotomy in 51 patients (Table 4). Postoperative esophageal strictures developed more often in the long-gap than in short-gap atresia (P = 0.042). However, circular myotomy was not significantly associated with esophageal stricture (P = 0.078).
Anastomotic leakage was the second most common complication in our study. Only one case of anastomotic leakage required surgery, as the other cases were resolved by conservative management. However, among these cases, six patients (8.3%) were found to have delayed TEF recurrence. The mean date of TEF recurrence was 6.7 months (range, 0.6 to 23 months) after primary operations. One case of H-type esophageal atresia and two cases of long-gap type C atresia were included. All underwent another surgery.
Overall, the mortality rate was 15.3% (11 patients). Eight patients died due to surgery-related complications, and two patients died after cardiac surgery. One patient with Down's syndrome died due to an unknown cause 1 year after surgery. The reasons for death due to surgery-related complications were leakage or recurrent TEF-induced respiratory failure (4 patients), postoperative sepsis with acute renal failure (3 patients), and hypoxic brain damage due to tracheomalacia (1 patient). If we include two patients who died immediately after birth, the mortality rate would increase to 17.6 % (13/74).
When comparing the mortality rate with the birth weight, the mortality rate of patients weighing less than 2.5 kg (34.6%, 9/26) was significantly higher than the rate of patients weighing at least 2.5 kg (4.3%, 2/46, P = 0.001).
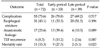
We grouped the patients into the early study period (from 1995 to 2003) and the late study period (from 2004 to 2010) based on an evenly balanced number of patients and the study duration.
In comparing the late period with the early period, patients in the late period had significantly lower rates of anastomotic leakage (P = 0.009) and mortality (P = 0.023) than those in the early period. However, the total complication rate, including esophageal stricture and recurrence of TEF was not significantly different between the two periods (Table 5).
Esophageal atresia is a complex congenital anomaly with a complicated prognosis. Although survival of patients with esophageal atresia has markedly improved due to advances in surgical techniques and neonatal intensive care, complications often occur, and morbidities after treatment are still regarded as an important issue [5,6].
The reasons for the high morbidity associated with esophageal atresia are well known [2,5,7,8]. Associated anomalies, low birth weight or prematurity, and likelihood of pneumonia are common findings with esophageal atresia and affect treatment outcome. In addition, variations in the type of atresia, anatomical differences, anastomotic tension induced by long-gap esophageal atresia, and lack of surgical experience are also considered as potential risk factors [6,7,9]. In this study, our results have shown that some of these factors are correlated with the postoperative prognosis. The incidence of complications is so high that 73.6% of patients have at least one complication. Postoperative esophageal strictures, which are the most common complication, were significantly correlated with the length of esophageal gap. Associated congenital anomalies are also common findings of esophageal atresia. Among them, major congenital heart disease, which is regarded as a prognostic factor, was one of the causes of death in this study.
Birth weight, another prognostic factor, is a valid factor in this study as well. Using the Waterston classification, a birth weight of 2.5 kg was used as one of the criteria to divide the patients into three groups [10]. Our data showed that patients weighing less than 2.5 kg at birth had a significantly higher mortality rate compared with patients weighing at least 2.5 kg at birth. Although these data were not analyzed by a multivariate analysis, they suggest that low birth weight is associated with poor prognosis, such as high incidence of associated anomalies, poor general physical status, and difficulty during the surgical procedure. However, these results are based on the data from the early period of the study. In the late period, we had only two cases of mortality with birth weights of 1.04 kg and 2.57 kg. Consequently, survival of patients in the late study period was not statistically associated with birth weight.
When we analyzed the data in early and late periods, significant improvements were found in the survival of patients in the late study period. Previous studies also showed that survival of esophageal atresia has gradually improved over past decades. Spitz et al. [11] emphasized that early diagnosis with improvements in neonatal intensive care and a number of surgical advances contribute to reductions in mortality; they revised the criteria for risk classification to be more tolerant of high-risk patients previously assigned using the Waterston classification. In addition, Poenaru et al. [12] proposed a new classification, the Montreal classification, which depends on the use of a ventilator and major combined anomalies. These new classifications attempted to define new risk factors and their association with the improved outcome. Although the timing of the early and late periods in this study is later than either the Spitz or the Montreal classification schemes, our results are supportive of improvements in outcome.
One interesting result of our study was the incidence of gross type A esophageal atresia. Usually, the incidence of type A atresia is less than 10%, but our data showed a relatively high incidence of type A (15.3%) [3,5,13]. Therefore, we used various surgical methods such as esophago-cologastrostomy (ECG), transhiatal gastric pull-up (THGP), and transthoracic esophago-esophagostomy after elongation (TEEE). Whether the esophagus should be preserved or replaced using either the stomach or colon, are still controversial [3,4,14,15]. Our outcomes after the different surgical methods were not analyzed statistically because of the few cases performed using each type of surgery. However, two of the three patients who received ECG died due to postoperative complications. The patients who received the other staged operations, THGP and TEEE, are still alive. Therefore, we suggest that staged operation using TEEE or THGP is better than ECG as a treatment for long-gap esophageal atresia, including type A. However, further research regarding the best choice of surgical method for either long-gap or type A esophageal atresia should be undertaken.
The other noticeable finding of this study is the use of chest CT for preoperative diagnosis. Traditionally, a diagnosis of esophageal atresia is not difficult. Simple insertion of a nasogastric tube and its coiling in the proximal esophageal pouch is a sufficient diagnostic method. However, recent studies report that a chest CT image with three-dimensional (3D) reconstruction provides preoperative information about the anatomy around the esophageal atresia, even the esophageal gap length. Therefore, CT imaging can help to determine the optimal surgical method [16-18]. We used a chest CT for the same reasons in 17 cases (23.6%). Our results could not confirm the effectiveness of the 3D reconstructed image in terms of the anatomy around the esophageal atresia and the esophageal gap. However, because the number of our CT performances was small, further research regarding the more established applications of chest CT imaging is needed.
In Korea, clinical studies of esophageal atresia are not common: only five reports with a large patient population were previously published [19-23]. When we analyzed those studies, our results were comparable regarding the high incidence of combined anomalies and the complication rates; however, one intriguing result was the incidence of GER (Table 6).
GER is a significant complication of the treatment of esophageal atresia: Seo et al. [20] reported the incidence of GER as 39.0%, and Kim et al. [21] reported it as 19.2%. According to the literature, GER occurs in approximately 40% of cases of esophageal atresia with approximately one-half requiring surgery [3,24,25]. In our study, GER developed in 4.2% of patients, and all were treated by conservative management. We could not exclude, however, underestimation of the incidence of GER because of the limitations of a retrospective study and an insufficient follow-up period.
In summary, our data suggest that the survival of patients with esophageal atresia has improved over the years and the rate of anastomotic leakage was significantly reduced. However, overall morbidities related surgical treatment of esophageal atresia still exists with high incidence. Further studies to reduce the surgical complications should be required.
Figures and Tables
References
1. Haight C, Towsley HA. Congenital atresia of the esophagus with tracheoesophageal fistula and end-to-end anastomosis of esophageal segments. Surg Gynecol Obstet. 1943. 76:672–688.
2. Lopez PJ, Keys C, Pierro A, Drake DP, Kiely EM, Curry JI, et al. Oesophageal atresia: improved outcome in high-risk groups? J Pediatr Surg. 2006. 41:331–334.
3. Spitz L. Oesophageal atresia. Orphanet J Rare Dis. 2007. 2:24.
4. Kim SM, Choi SH, Kim SH, Kwon IK, Han SJ, Oh JT. Esophageal atresia without tracheoesophageal fistula: report of 6 cases. J Korean Assoc Pediatr Surg. 2005. 11:157–164.
5. Castilloux J, Noble AJ, Faure C. Risk factors for short- and long-term morbidity in children with esophageal atresia. J Pediatr. 2010. 156:755–760.
6. Hicks LM, Mansfield PB. Esophageal atresia and tracheoesophageal fistula. Review of thirteen years' experience. J Thorac Cardiovasc Surg. 1981. 81:358–363.
7. Engum SA, Grosfeld JL, West KW, Rescorla FJ, Scherer LR 3rd. Analysis of morbidity and mortality in 227 cases of esophageal atresia and/or tracheoesophageal fistula over two decades. Arch Surg. 1995. 130:502–508.
8. Choudhury SR, Ashcraft KW, Sharp RJ, Murphy JP, Snyder CL, Sigalet DL. Survival of patients with esophageal atresia: influence of birth weight, cardiac anomaly, and late respiratory complications. J Pediatr Surg. 1999. 34:70–73.
9. Sharma AK, Shekhawat NS, Agrawal LD, Chaturvedi V, Kothari SK, Goel D. Esophageal atresia and tracheoesophageal fistula: a review of 25 years' experience. Pediatr Surg Int. 2000. 16:478–482.
10. Waterston DJ, Carter RE, Aberdeen E. Oesophageal atresia: tracheo-oesophageal fistula. A study of survival in 218 infants. Lancet. 1962. 1:819–822.
11. Spitz L, Kiely EM, Morecroft JA, Drake DP. Oesophageal atresia: at-risk groups for the 1990s. J Pediatr Surg. 1994. 29:723–725.
12. Poenaru D, Laberge JM, Neilson IR, Guttman FM. A new prognostic classification for esophageal atresia. Surgery. 1993. 113:426–432.
13. Tsai JY, Berkery L, Wesson DE, Redo SF, Spigland NA. Esophageal atresia and tracheoesophageal fistula: surgical experience over two decades. Ann Thorac Surg. 1997. 64:778–783.
14. Spitz L. Esophageal atresia. Lessons I have learned in a 40-year experience. J Pediatr Surg. 2006. 41:1635–1640.
15. Khan AR, Stiff G, Mohammed AR, Alwafi A, Ress BI, Lari J. Esophageal replacement with colon in children. Pediatr Surg Int. 1998. 13:79–83.
16. Ratan SK, Varshney A, Mullick S, Saxena NC, Kakkar S, Sodhi PK. Evaluation of neonates with esophageal atresia using chest CT scan. Pediatr Surg Int. 2004. 20:757–761.
17. Zhang Z, Huang Y, Su P, Wang D, Wang L. Experience in treating congenital esophageal atresia in China. J Pediatr Surg. 2010. 45:2009–2014.
18. Fitoz S, Atasoy C, Yagmurlu A, Akyar S, Erden A, Dindar H. Three-dimensional CT of congenital esophageal atresia and distal tracheoesophageal fistula in neonates: preliminary results. AJR Am J Roentgenol. 2000. 175:1403–1407.
19. Han JH, Chung JH, Song YT. Esophageal atresia with tracheoesophageal fistula: a 20 year experience of 51 cases. J Korean Assoc Pediatr Surg. 2008. 14:1–11.
20. Seo J, Kim DY, Kim AR, Kim DY, Kim SC, Kim IK, et al. An 18-year experience of tracheoesophageal fistula and esophageal atresia. Korean J Pediatr. 2010. 53:705–710.
21. Kim SS, Rhim SY, Jung PM. A clinical review of esophageal atresia: one surgeon's experience. J Korean Assoc Pediatr Surg. 2008. 14:14–20.
22. Jeong JH, Kim HE, Lee SK, Seo JM. The long-term outcome of esophageal atresia. J Korean Assoc Pediatr Surg. 2008. 14:117–124.
23. Chun YS, Jung SE, Lee SC, Park KW, Kim WK. Seventeen years' experience with ninety-six esophageal atresias. J Korean Assoc Pediatr Surg. 1995. 1:140–148.
24. Parker AF, Christie DL, Cahill JL. Incidence and significance of gastroesophageal reflux following repair of esophageal atresia and tracheoesophageal fistula and the need for anti-reflux procedures. J Pediatr Surg. 1979. 14:5–8.
25. Wheatley MJ, Coran AG, Wesley JR. Efficacy of the Nissen fundoplication in the management of gastroesophageal reflux following esophageal atresia repair. J Pediatr Surg. 1993. 28:53–55.




 ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download