Abstract
Purpose
The aim of our study was to compare single incision laparoscopic cholecystectomy (SILC) and conventional laparoscopic cholecystectomy (CLC) with respect to clinical outcomes.
Methods
Patients with less than a 28 body mass index (BMI) and a benign gall bladder disease were enrolled in this study. From January 2011 to February 2012, 30 consecutive patients who underwent SILC were compared with 30 patients who underwent CLC during the same period. In this study, all operations were performed by one surgeon. In each group, patient characteristics and perioperative data were collected.
Results
There was no significant difference in the preoperative characteristics. There was no significant difference in the postoperative laboratory result (alanine aminotransferase, aspartate aminotransferase, and alanine aminotransferase), number of conversion and complication cases, and length of hospital stay. The operation time was significantly longer in the SILC group (78.5 ± 17.8 minutes in SILC group vs. 34.9 ± 5.75 minutes in CLC group, P < 0.0001). The total nonsteroidal antiinflammatory drug usage during perioperative period showed significantly higher in SILC groups (162 ± 51 mg in the SILC group vs. 138 ± 30 mg in the CLC group), but there was no statistically significant difference in opioid usage between two groups. The postoperative pain score was significantly higher in the SILC group at second, third, and tenth postoperative day. Satisfaction of postoperative wound showed superiority in SILC group.
After the first reports of laparoscopic cholecystectomy by Erich Muhe in 1985 [1], within several years the technique gained enormous popularity due to its significant advantages of reduced postoperative pain, shortened hospital stay, faster recuperation, and earlier return to normal function, so it became the gold standard procedure in cholecystectomy. During past two decades with a phenomenal change of laparoscopic technique, many laparoscopic surgeons worked to lessen wound size and number of incisions. These several years have seen numerous reports on single incisional laparoscopic surgery (SILS) in the surgical literature. Since Navarra et al. [2] reported that laparoscopic cholecystectomy through single umbilical incision may be technically feasible and could prove advantageous in selected patients, single incision laparoscopic cholecystectomy (SILC) gained popularity and several reports examined its feasibility and safety. Hong et al. [3], Kim et al. [4], and Choi et al. [5] also reported that SILC is feasible and safe as conventional laparoscopic cholecystectomy (CLC) with its cosmetic merit in Korea. Until now, SILC studies were simple presentation and/or retrospective studies of clinical outcomes after SILC. Prospective comparative studies between and SILC and conventional multi-port laparoscopic cholecystectomy are lacking. Therefore, the aim of our study was to compare SILC with CLC respect to clinical and cosmetic outcome through well designed prospective comparative study.
Before we began this study, 10 cases of SILC were performed. All of 10 cases were performed by one expert laparoscopic surgery in the hepatobiliary division. Serious complications did not occur in these 10 cases. However, SILC operation showed a higher pain score in visual analogue pain scale and long operation time, when compared to CLC. Following these initial clinical studies, we planned a prospective controlled study to evaluate advantage, disadvantage and feasibility of SILC operation, when compared to CLC. The study protocol was approved by the Institutional Review Board of the Wonkwang University School of Medicine and Hospital in Feb. 2011. Each patient's decision to participate in the study was voluntary and informed consent was obtained from each patients. All patients, from age 18 to 90 years, with preoperative diagnosis of benign gall bladder disease scheduled for elective cholecystectomy at the Department of Surgery, Wonkwang University School of Medicine and Hospital in Korea, were offered the opportunity to participate in this trial. The exclusion criteria included the following: 1) patients with acute cholecystitis in physical exam and imaging study-ultrasonography, computed tomography or hepatobiliary scan, 2) patients with body mass index [BMI] > 28, 3) patients with previous upper abdominal surgery, 4) patients with suspected presence of common bile duct stones or intrahepatic bile stones, 5) patients with suspected gall bladder malignancy, 6) American Society of Anesthesiologist (ASA) class IV and V. Eligible patients were allocated in 1 of 2 groups (SILC group or CLC group). We performed a prospectively matched comparable analysis between 30 consecutive patients who underwent SILC and prospective cohort of 30 patients who underwent CLC from January 2011 to February 2012. Conversion or failure of SILC or CLC was defined as insertion of additional 5 mm port or laparotomy. Operation time was defined as from transumbilical incision time until skin reapproximation time.
All surgery in this study was performed by one experienced laparoscopic surgeon. Before proceeding of this study, we decided to preclude the use of hybrid techniques for easily traction of gallbladder-such as using stay suture, wire or 2 mm sized instrument. All surgeries were performed under general anesthesia in the supine and lithotomy position. The operating surgeon was placed between the patient's legs. In SILC operation, the 1.5 to 2.0 cm sized transumbilical incision was made by open method, and fascia and peritoneum was dissected by electrocautary. And then transumbilical port was inserted. A transumbilical port was used and a SILS port (Covidien Inc., Norwalk, CT, USA) in initial 3 cases and OCTO-port (Dalim Co., Seoul, Korea) was used in the remaining cases. The abdominal cavity was insufflated to a pneumoperitoneum of 12 mmHg, and 30° laparoscope then inserted. The patients were placed in a reverse Trendelenburg position, with right side elevated. 5 mm standard length articulating grasper instrument and 5 mm standard length straight dissecting instrument (dissector) then were inserted SILC operation. Articulating grasper was used at the infundibulum or Hartmann's pouch for lateral dissection without traction by stay suture or 2 mm instruments for cephalad retraction of gall bladder body (Fig. 1). The gall bladder hilum was then dissected with dissector to expose the cystic duct and cystic artery which were clipped with 5 mm hemo-lock (Weck Closure Systems, Triangle Park, NC, USA) and a 5 mm Endoclip (Covidien Inc.), respectively and then divided with scissors. The gall bladder was dissected from the gallbladder fossa with hook electrocautery device. To allow removal of the gallbladder, the retrieval bag Endocatchbag (Covidien Inc.) was placed beneath the gallbladder fossa through the 10 mm port. The transumbilical wound was reapproximated with usual suture method. The operating process of conventional 3 port laparoscopic cholecystectomy was not significantly different from published operating method. Conversion of SILC or CLC was defined as open cholecystectomy or insertion of additional port.
To control postoperative pain on the day of surgery, Kotoloc (Keromin, 30 mg/mL/ample, Ketorolac tromethamin, Hana Pham Co., Seoul, Korea) was injected one ampule two times a day, intravenously. If patients complained of increased pain within 1 hour after injection of analgesic, narcotic pain reliever (Demerol, meperidine hydrochloride, 1 mg/mL/ample) was injected, half ampule, intravenously. From postoperative 1 day to discharge of hospital, oral analgesic (somalgen, Talniflumate, 370 mg/tablet, Kunwha Phamaceutical Co., Seoul, Korea) was administered three times a day. Postoperative pain was measured using the visual analogue scale (VAS) every 12 hours (AM 9 and PM 9) in hospitalization. VAS was graded from 0 to 10. Patients were eligible for discharge when they tolerated a regular diet and VAS pain score was less than 4.
Collected date included patient demographics (age, gender, BMI, ASA grade), postoperative laboratory finding (leukocyte count, liver function test, alanine aminotransferase, gamma-glutamyltransferase), clinicopathologic characteristics (diagnosis), and perioperative clinical finding (operation time, conversion rate, VAS pain score, total dose of analgesics, complication rate, length of hospital stay). We evaluated satisfaction of cosmetic outcome through telephone interviews to all patients in this study at 3 months after operation. Satisfaction of cosmetic outcome was defined by each patient on 1 to 3 scale with 1 being satisfaction, 2 being unconcern about wound and 3 being dissatisfaction.
Results are expressed as median values with the interquartile range or mean values ± standard deviation. Continuous variables were compared using Student's t-test, the Mann-Whitney U test or repeated measures analysis of variance. The relationship of postoperative pain and operation time according cases was analyzed by correlation analysis and linear regression method, respectively. Discrete variables were analyzed with the chi-square test or Fisher's exact test. We performed correlation analysis between several parameters and VAS pain score of postoperative 1, 2, and 3 day. Statistical analysis was performed using SPSS ver.14.0 (SPSS Inc., Chicago, IL, USA). A probability of 0.05 or less was considered statistically significant.
From January 2011 to February 2012, there were 60 eligible patients with benign gallbladder disease verified by ultrasonography or computed tomography, who were randomized to SILC (n = 30) and CLC (n = 30). No one who participated in this study was eliminated.
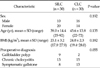
There were no significant differences between the SILC group and CLC group with regards to indication of surgery or medical or demographic variables (age, gender distribution) (Table 1).
Operation time between SILS group and CLC group were 78.5 ± 17.8 and 34.9 ± 5.75, respectively. The SILC group took twice as long as the CLC group (P < 0.001). Operation success rate between the two groups were 93.3% and 100%, respectively. The conversion rates were 6.7% (n = 2) and 0%, respectively (P = 0.492). The causes of two conversion case in of SILC group were ambiguous cystic duct anatomy and long operation time due to adhesion. There was no open cholecystectomy between groups. The two cases that needed an additional port occurred in the SILC group (Table 2).
At postoperative 1 day, laboratory findings were similar for both the SILC group and CLC group. The complication rate between SILC and CLC groups were 10% (n = 3) and 0.0%, respectively and there was no significant difference (P = 0.237). The 3 cases of complication in SILC were all wound problems, seroma. There was no case of bile leak or common bile duct injury in either group. The mean length of hospital stay for the SILC was 4.0 ± 0.9, for the CLC group 3.7 ± 0.9. There was not statistically difference between both groups (P = 0.175). Mean perioperative cost between SILC and CLC were 710.000 Korean Won (KRW, the currency of South Korea) and 700.000 KRW, respectively. There was no difference statistically (Table 3).
In correlation analysis, there was no significant relationship between operation time of all patients and VAS pain score. The relationship between operative time of each operation type and VAS pain score also did not show a significant association. Also, there was no association between BMI and VAS pain score. However, in VAS the pain score according to operation type, the SILC group showed a significantly higher pain score than the CLC from postoperative day 1 to day 3 (P = 0.005) (Fig. 2). The total dose of analgesic also was significantly higher in SILC group (P = 0.037) (Table 3).
We evaluated satisfaction of cosmetic outcome through telephone interviews to all patients in this study. Satisfaction of cosmetic outcome was defined on a 1 to 3 scale with 1 being satisfaction, 2 being unconcern about wound and 3 being dissatisfaction. There was statistically significant difference between groups on cosmetic satisfaction (P < 0.0001) (Fig. 3).
Laparoscopic cholecystectomy has become one of the most frequently performed procedures in visceral surgery. Current efforts focus on minimizing trauma and improving cosmesis by reduction of inserted trocars. The appearance of single-port technology in the recent years continues this trend. SILC can predict better cosmetic outcome, reduced postoperative pain due to less operative trauma, fewer complications, and quickly recovery. However, the superiority of the SILC compared to the CLC, is still controversial. Since SILC was first introduced, within 2 to 3 years, operative indication and the benefits with regards to operation time reduction, postoperative pain, and cosmetic outcome have been actively studied. However, with the advent of any new surgical technique, patient safety must be the primary concern before more subjective outcomes such as cosmesis or pain. Many authors have been report that SILC was feasible and safe in selected patients with uncomplicated gallstone disease or gallbladder polyp [6]. However, SILC is difficult to recommend in patients who have a high BMI or acute cholecystitis because relatively high conversion rate to CLC, increasing complication rate (bile leak by gall bladder rupture, wound infection), and prolonged operative time [7].
The operative time of SILC in several studies reported no statistically significant difference compared to CLC [8,9]. However, Wang et al. [10] by a meta-analysis of SILC clinical trials recently reported that SILC carries a longer operative time. In our study, mean operative time was 79 minutes, comparable with reports by Roberts et al. (80 minutes) [11] and Solomon et al. (78 minutes) [12]. In our study, time consuming points that were occurred during SILC were as follows: 1) time from transumbilical incision to multiport insert; 2) traction of gall bladder for good operative field; 3) intracorporeal interruption between scope and instruments. To reduce operative time of SILC, introduction of instrument that can be more flexible, articulation, and more firm holding may be considered to reduce interruptions between laparoscope and instruments, and can provide better exposure of the operation field. Sasaki et al. [13] suggested using WLR (wire loop retractor), anchoring suture, and 2 mm sized reusable instrument to reduce operative time. Also, in order to adapt to a new surgical technique, experience of several cases is needed. Rivas et al. [14] and Feinberg et al. [15] proposed a conservative learning curve of 20 to 25 cases for safe adoption of SILC. So we underwent 10 cases of SILC by one experienced laparoscopic surgeon as learning curve, and mean operative time was 89 minutes.
The reduction of postoperative pain is one of the primary concerns on SILC. Recently published randomized studies have suggested that patients undergoing SILC had similar pain score and total amount of analgesic within 24 hours after operation when compared with standard laparoscopic cholecystectomy [6,16]. In our study, VAS pain score of the SILC group was significantly higher than that of the CLC group and the total dose of analgesic also was significantly higher in SILC group though with no benefit in terms of postoperative hospital stay. We hypothesized that increasing operative time will increase postoperative pain because of prolonged stretching and ischemia of umbilical wound by single multichannel port. However, the relationship between operative time according to operative type and VAS pain score did not show in this study. Another reason for high postoperative pain score of SILC group in this study may be considered that the effect of less port numbers on postoperative pain might be compromised by a large incision size [17]. Recently, we changed single multichannel port from SILS and Octo-port to handmade glove port that was made with Alexis wound retractor and hand glove in operation field. Since then, complains of postoperative pain have decreased. For this reason, we seemed to be analyzing degree of postoperative pain according to kind of single multichannel port.
SILC has been reported to have better cosmetic outcome compared with CLC. Our study also showed high level of satisfaction in SILC group. However, Ma et al. [17] and Garg et al. [18] reported that patients' perceptions regarding cosmetic outcome after SILC and CLC were similar in both groups. Hey et al. [19] reported that patients ranked the level of risk for complications and postoperative pain above cosmetic results in determining their choice of procedure, if sufficient contemporary data of SILC is provided to patients.
In summary, on the basis of our study, SILC have longer operative time and higher postoperative pain score. However, SILC showed a high level of satisfaction in term of cosmetic outcome. SILC for cholecystectomy may at least be equal to CLC in term of efficacy and patient safety. According to the literature, the superiority of SILC over CLC, seems to still be not accepted. Large, randomized, prospective studies will be required to investigate the potential benefits of the SILC technique such as reduced operative time, reduced postoperative pain, improved cosmesis, and improved patient satisfaction.
In conclusion, SILC may be recognized as an alternative for CLC in selected patients (with a low risk of adhesion or technical difficulty), despite longer operative time and higher postoperative pain. So, we propose as indication with the patient who want cosmetic satisfaction, and who have keloid skin characteristic, and who decide SILC with enough information about SILC.
Figures and Tables
Fig. 1
Articulating grasper is being used at infundibulum, or Hartmann's pouch, for lateral dissection without any stay suture for cephalad retraction of gall bladder body.

Fig. 2
Comparison of visual analogue scale (VAS) pain score (mean) during postoperative day between single incision laparoscopic cholecystectomy (SILC) and conventional laparoscopic cholecystectomy (CLC). Differences at postoperative day (POD)2 and POD3 are statistically significant in independent t-test. In repeat measure analysis, P-value was 0.005.
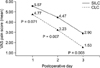
Fig. 3
Evaluation of cosmetic outcome according to operative type through telephone survey. There was statistical difference between groups on cosmetic satisfaction. In chi-square analysis, P-value is less than 0.001.

Table 3
Clinical outcomes of postoperative parameter

Values are presented as mean ± SD.
SILC, single incision laparoscopic cholecystectomy; CLC, conventional 3-port laparoscopic cholecystectomy; POD, postoperative day; NSAID, nonsteroidal anti-inflammatory drug; KRW, Korean Won.
a)Kotoloc (keromin, 30 mg/mL/ample, ketorolac tromethamin). b)Demerol (meperidine hydrochloride, 50 mg/ample).
Notes
References
1. Litynski GS. Erich Muhe and the rejection of laparoscopic cholecystectomy (1985): a surgeon ahead of his time. JSLS. 1998. 2:341–346.
2. Navarra G, Pozza E, Occhionorelli S, Carcoforo P, Donini I. One-wound laparoscopic cholecystectomy. Br J Surg. 1997. 84:695.
3. Hong TH, You YK, Lee KH. Transumbilical single-port laparoscopic cholecystectomy: scarless cholecystectomy. Surg Endosc. 2009. 23:1393–1397.
4. Kim BS, Kim KC, Choi YB. A comparison between single-incision and conventional laparoscopic cholecystectomy. J Laparoendosc Adv Surg Tech A. 2012. 22:443–447.
5. Choi SH, Hwang HK, Kang CM, Lee WJ. Single-fulcrum laparoscopic cholecystectomy: a single-incision and multi-port technique. ANZ J Surg. 2012. 82:529–534.
6. Markar SR, Karthikesalingam A, Thrumurthy S, Muirhead L, Kinross J, Paraskeva P. Single-incision laparoscopic surgery (SILS) vs. conventional multiport cholecystectomy: systematic review and meta-analysis. Surg Endosc. 2012. 26:1205–1213.
7. Han HJ, Choi SB, Kim WB, Choi SY. Single-incision multiport laparoscopic cholecystectomy: things to overcome. Arch Surg. 2011. 146:68–73.
8. Lai EC, Yang GP, Tang CN, Yih PC, Chan OC, Li MK. Prospective randomized comparative study of single incision laparoscopic cholecystectomy versus conventional four-port laparoscopic cholecystectomy. Am J Surg. 2011. 202:254–258.
9. Bucher P, Pugin F, Buchs NC, Ostermann S, Morel P. Randomized clinical trial of laparoendoscopic single-site versus conventional laparoscopic cholecystectomy. Br J Surg. 2011. 98:1695–1702.
10. Wang D, Wang Y, Ji ZL. Laparoendoscopic single-site cholecystectomy versus conventional laparoscopic cholecystectomy: a systematic review of randomized controlled trials. ANZ J Surg. 2012. 82:303–310.
11. Roberts KE, Solomon D, Duffy AJ, Bell RL. Single-incision laparoscopic cholecystectomy: a surgeon's initial experience with 56 consecutive cases and a review of the literature. J Gastrointest Surg. 2010. 14:506–510.
12. Solomon D, Bell RL, Duffy AJ, Roberts KE. Single-port cholecystectomy: small scar, short learning curve. Surg Endosc. 2010. 24:2954–2957.
13. Sasaki K, Watanabe G, Matsuda M, Hashimoto M. Original single-incision laparoscopic cholecystectomy for acute inflammation of the gallbladder. World J Gastroenterol. 2012. 18:944–951.
14. Rivas H, Varela E, Scott D. Single-incision laparoscopic cholecystectomy: initial evaluation of a large series of patients. Surg Endosc. 2010. 24:1403–1412.
15. Feinberg EJ, Agaba E, Feinberg ML, Camacho D, Vemulapalli P. Single-incision laparoscopic cholecystectomy learning curve experience seen in a single institution. Surg Laparosc Endosc Percutan Tech. 2012. 22:114–117.
16. Garg P, Thakur JD, Garg M, Menon GR. Single-incision laparoscopic cholecystectomy vs. conventional laparoscopic cholecystectomy: a meta-analysis of randomized controlled trials. J Gastrointest Surg. 2012. 16:1618–1628.
17. Ma J, Cassera MA, Spaun GO, Hammill CW, Hansen PD, Aliabadi-Wahle S. Randomized controlled trial comparing single-port laparoscopic cholecystectomy and four-port laparoscopic cholecystectomy. Ann Surg. 2011. 254:22–27.
18. Garg P, Thakur JD, Raina NC, Mittal G, Garg M, Gupta V. Comparison of cosmetic outcome between single-incision laparoscopic cholecystectomy and conventional laparoscopic cholecystectomy: an objective study. J Laparoendosc Adv Surg Tech A. 2012. 22:127–130.
19. Hey J, Roberts KJ, Morris-Stiff GJ, Toogood GJ. Patient views through the keyhole: new perspectives on single-incision vs. multiport laparoscopic cholecystectomy. HPB (Oxford). 2012. 14:242–246.




 ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download