Abstract
Purpose
In Korea, the results of bariatric surgery have not been compared with those of nonsurgical treatment. The purpose of this study was to evaluate the effectiveness and safety of bariatric surgery vs. conventional nonsurgical treatment in severely obese Koreans.
Methods
In this retrospective cohort study, we reviewed the medical charts of 261 consecutive subjects who underwent bariatric surgery and 224 subjects who were treated with weight control medication and lifestyle modification therapy between January 2008 and February 2011. Measures of clinical effectiveness, including change in weight (%) and comorbid diseases, and occurrence of complications, were investigated for 18 months after bariatric surgery.
Results
Body mass index (BMI) was higher in the surgery group than in the conventionally treated group (mean ± standard deviation, 39.0 ± 6.2 vs. 34.3 ± 3.8). Diabetes was more prevalent in the surgery group than in the conventionally treated group (39.1% vs. 12.9%). The change in weight (%) between baseline and 18 months posttreatment was significantly greater in the surgery group (22.6%) than in the conventional therapy group (6.7%). While 57%, 47%, and 84% of subjects recovered from diabetes, hypertension, and dyslipidemia, respectively, in the surgery group, 10%, 20%, and 24% of subjects recovered from these conditions in the conventional group. Fifty-one subjects (19.5%) in the surgery group reported 61 complications (23.4%).
Obesity is an epidemic healthcare problem worldwide. In the United States, the prevalence of obesity, defined as a body mass index (BMI) ≥ 30 kg/m2, has increased, and now includes >30% of the population [1]. Data from the Korean National Health and Nutritional Examination Survey indicate that the prevalence of obesity in Korea, defined as a BMI > 25 kg/m2, increased from 26% in 1998 to 31% in 2009 [2]. During the same period, the prevalence of severe obesity (BMI > 30 kg/m2) increased markedly from 2.4 to 4.7%. Although the prevalence of obesity in Korea has been increasing rapidly, it remains much lower than in Western countries. However, Asians are more predisposed to abdominal obesity than are Western individuals, and obesity comorbidities such as diabetes, high blood pressure, high plasma triglyceride (TG) level, and low high-density lipoprotein cholesterol level seem to occur at a BMI that is much lower than the World Health Organization recommended cutoff value for obesity in Asians [3]. Therefore, different criteria for obesity are applied depending on ethnicity and nationality. Whereas severe obesity is defined as a BMI ≥ 35 kg/m2 in Western populations, the cutoff value for severe obesity has been lowered to a BMI ≥ 30 kg/m2 in Asians [4-6].
In Western society, bariatric surgery is recommended for individuals with a BMI ≥ 35 kg/m2 with comorbidities or a BMI ≥ 40 kg/m2 without comorbidities. The Asian-Pacific Bariatric Surgery Group recommends bariatric surgery for obese Asians with a BMI ≥ 32 kg/m2 with comorbidities or a BMI ≥ 37 kg/m2 without comorbidities [7]. A survey of Korean bariatric surgeons found that the criteria for this recommendation in Korea are slightly lower than the Asian criteria (i.e., BMI ≥ 30 kg/m2 with comorbidities or BMI ≥ 35 kg/m2), which correspond to the cutoff values for severe obesity recommended by the Asian-Pacific Group.
The first bariatric surgery in Korea was performed in 2003 [8], and about 1,000 bariatric surgeries have been performed annually since 2011. Laparoscopic adjustable gastric banding (LAGB), laparoscopic Roux-en-Y gastric bypass (LRYGB), and laparoscopic sleeve gastrectomy (LSG) are the three most common bariatric procedures performed in Korea. However, the effect of bariatric surgery has not been compared with that of nonsurgical treatment in a Korean population.
Therefore, we conducted a comparative analysis of the results of bariatric surgery and conventional nonsurgical treatment in severely obese patients. The purpose of this study was to evaluate the effectiveness and safety of bariatric surgery vs. conventional nonsurgical treatment in severely obese Koreans.
We used a retrospective cohort design with a medical chart review to investigate the effectiveness of bariatric surgery compared with that of conventional therapy. The surgery group included adults who underwent consecutive bariatric surgeries at the Departments of Surgery of seven Korean tertiary medical centers between January 2008 and February 2011. The conventional group included adults who were treated with conventional therapies, such as weight control medication, lifestyle modification therapy, and educational program with dietician and exercise practitioner at the Departments of Family Medicine of two Korean tertiary medical centers during the same period. Patients who were ≤17 years old and/or had a BMI < 30 kg/m2 were not included in this study. The ethics review board of each hospital and the National Evidence-Based Healthcare Collaborating Agency involved in this study approved the study protocol.
Baseline height, weight, blood pressure, and laboratory data were collected by physical examination and laboratory assessments within a few days before bariatric surgery in the surgery group. These data were collected in the conventional therapy group at the first visit to start a weight loss program in the family medicine departments. Weight, blood pressure, and laboratory findings were collected over time when the subjects visited the hospital. Medical history information before bariatric surgery or the first visit for conventional therapy was investigated through a chart review. Descriptive information of the event, onset date, and hospitalization were collected to investigate complications related to bariatric surgery.
The clinical effectiveness of weight loss was investigated using two parameters. The first parameter was change in weight (%), calculated by dividing weight change from baseline by baseline weight. The second parameter was the percentage of excess weight loss (%EWL), calculated by dividing the weight change from baseline by excess weight, which was obtained by subtracting ideal body weight from actual baseline weight. Ideal body weight was calculated using height-adjusted weight, depending on sex, for a medium frame according to the 1983 Metropolitan Life Insurance Company tables [9].
Recovery from comorbidities such as diabetes, hypertension, and dyslipidemia was investigated over time. Diabetes was defined as the use of medication, fasting blood glucose level ≥ 126 mg/dL, or glycosylated hemoglobin (HbA1C) concentration ≥ 6.5%. Hypertension was defined as the use of medication, systolic blood pressure ≥ 140 mmHg, or diastolic blood pressure ≥ 90 mmHg. Dyslipidemia was defined as the use of medication, total cholesterol (TC) level ≥ 240 mg/dL, TG level ≥ 200 mg/dL, or low-density lipoprotein cholesterol (LDL-C) level ≥ 160 mg/dL. Patients who did not meet the criteria for a given comorbidity were considered to have recovered from that comorbidity after intervention.
We summarized the patient characteristics of the two groups, and compared the baseline characteristics between groups using a t-test for continuous variables and a chi-squared test for categorical variables. To investigate weight change, weight measurements obtained during routine visits were summarized at 3-month intervals. For example, if one patient's weight was measured twice during a 3-month period from baseline, the weight value at 3 months was the mean value of the two measurements. Study outcomes such as change in weight (%) and %EWL were summarized at 0 (baseline), 3, 6, 9, 12, 15, and 18 months, and 95% confidence intervals (CIs) were calculated. The t-test was used to compare study outcomes between the two groups at each time point. Matching and the generalized estimating equation (GEE) model were used to balance confounding factors at baseline between the two groups [10]. Three matching variables were considered: age (±5 years), BMI (±3 kg/m2), and sex. The dependent variable for the GEE model was change in weight (%), and measurement time, age, and sex were included as independent variables. Measurement time and age were inputted as continuous variables. Two independent researchers inputted data into the data collection forms. Then, data entry errors were checked using the SAS ver. 9.2 (SAS Institute Inc., Cary, NC, USA) and corrected. Data were analyzed using the SAS software.
We identified 261 subjects in the surgery group and 224 subjects in the conventional therapy group. Patient characteristics are shown in Table 1. The median follow-up periods were 9 months for the surgery group and 8 months for the conventional therapy group. BMI was higher in the surgery group than in the conventional therapy group (mean ± standard deviation, 39.0 ± 6.2 vs. 34.3 ± 3.8 kg/m2). Mean age was lower in the surgery group than in the conventional therapy group (36 ± 10.8 vs. 41 ± 13.3 years). In total, 75.5% of patients in the surgery group and 56.7% of patients in the conventional therapy group were female. Diabetes was more prevalent in the surgery group than in the conventional therapy group (39.1% vs. 12.9%). In the surgery group, 27.6% of procedures were LAGB, 28.0% were LRYGB, and 44.4% were LSG. Most subjects (95%) in the conventional group used antiobesity drugs. Phentermine (26.3%) was the most frequently prescribed medicine, followed by sibutramine (24.1%), fluoxetin (12.8%), mazindole (10.5%), bupropion (10.1%), and orilistat (4.9%). Sibutramine was withdrawn from the Korean market at the end of 2010.
Treatment outcomes such as change in weight (%) are shown in Fig. 1. The change in weight (%) from baseline to 18 months was significantly higher in the surgery group (22.6%; 95% CI, 19.1 to 26.0%) than in the conventional therapy group (6.7%; 95% CI, 4.4 to 9.1%). This pattern was consistent with %EWL. The %EWL of surgery group was 61.4% whereas the %EWL of conventional therapy group was 20.6% at 18 months after treatment. The surgery group showed significant weight loss (P < 0.001) at each time point throughout the 18-month follow-up period in the subgroup analysis in terms of BMI; 30 ≤ BMI < 35 and BMI ≥ 35 groups (Fig. 2).
There was no significant difference of change in weight (%) from baseline to 18 months according to operative procedures (20.8% for LAGB, 26.6% for LRYGB, and 22.3% for LSG).
After age, sex, and BMI were matched between the two groups, the pattern of change in weight (%) was similar to that before matching. Weight change was greater in the surgery group, with a similar significance before and after matching (P < 0.001).
Time and treatment effects for change in weight (%) from baseline using the GEE are described in Table 2. Change in weight (%) was 1.2% greater in the surgery group than in the conventional therapy group over a 1-month period. Thus, the difference in the percentage of weight change between the surgery and conventional therapy groups was 25.4% at 18 months. Age and sex did not significantly affect weight loss.
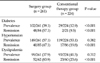
Recovery from concomitant diseases such as diabetes, hypertension, and dyslipidemia was more frequent in the surgery group than in the conventional therapy group (Table 3). While 57.1%, 47.1%, and 83.9% of subjects recovered from diabetes, hypertension, and dyslipidemia, respectively, in the surgery group, 9.5%, 19.8%, and 23.6% of subjects recovered from these comorbidities in the conventional group.
Fifty-one (19.5%) of 261 subjects in the surgery group reported 61 complications (23.4%). Complications occurred within 30 days after bariatric surgery in 26 patients (10%) and >30 days after bariatric surgery in 32 patients (12.3%). Wound complications were most frequent (3.4%) among complications that occurred within 30 days. Among complications occurring after 30 days, port/band revision/removal-related complications were most frequent (17/261, 6.5%). Thus, total complication rate was higher in LAGB than other two procedures. One patient (0.38%) died due to aspiration pneumonia within 30 days of bariatric surgery (Table 4).
In this retrospective study, we examined the records of patients who had undergone bariatric surgery to determine the effectiveness for weight reduction and improvement in comorbid diseases, as compared with that of conventional medical therapy. We showed that bariatric surgery was more effective than conventional therapy for weight loss and treatment of comorbid diseases in severely obese patients in Korea. Observed effects on weight loss were consistent after adjusting for major confounders such as BMI, age, and sex.
The effectiveness of bariatric surgery has been well established in Western countries, where the prevalence of obesity is high. Bariatric surgery is the most effective option for weight loss in severely obese patients [11-13]. However, the first bariatric surgery was performed in Korea relatively recently, in 2003. About 1,000 bariatric surgeries were performed last year. The most frequent bariatric procedure (about 70%) was LAGB performed in private clinics. Because the history of bariatric surgery in Korea is short, few long-term investigations or comparative analyses with conventional therapy have been reported. Additionally, whether the results of bariatric surgery in Korea are comparable with those in Western countries remains unknown. This study is the first report of the results of Korean multicenter consecutive bariatric surgeries.
Our weight loss findings are in agreement with those of retrospective studies [13,14]. Many studies have reported not only the weight reduction effect, but also the survival effect of bariatric surgery [13,14]. However, we could not demonstrate a favorable survival effect of bariatric surgery in Korean obese patients because the observation period was limited to 18 months after surgery. Nevertheless, the weight reduction pattern we observed was comparable to those reported in previous studies, including the early (18-month) results of the Swedish Obese Subjects (SOS) study [13], a large-scale multicenter cohort study. In contrast, the control group in our study showed 8% weight loss after 18 months, whereas the control group in the SOS study showed only 1% weight change. The reasons for this discrepancy may be that the mean BMI of the control group was lower in the present study than in the SOS study, and that conventional medical therapy in the present study was actively conducted in tertiary hospitals.
Recovery from comorbidities such as diabetes, hypertension, and dyslipidemia was better in the surgery group than in the conventional therapy group in the present study. The remission of diabetes was observed in 57.1% of subjects in the surgery group and 9.5% of subjects in the conventional therapy group. This result was consistent with those of previous studies [15-17].
Buchwald et al. [17] reported a large-scale meta-analysis of 22,094 patients. In that study, diabetes was completely resolved in 76.8% of patients. In two comparative cohort studies, the SOS study [13] and the Utah Obesity study [14], diabetes remission rates were 66% and 74%, respectively, in the surgery groups, but <1% in the control groups.
Two prospective randomized trials assessing the results of surgical treatment of obese patients with diabetes have been published in the New England Journal of Medicine. Schauer et al. [18] evaluated the efficacy of intensive medical therapy alone versus medical therapy plus LRYGB or LSG in 150 obese patients with uncontrolled type 2 diabetes. The target HbA1C concentration of 6.0% or less at 12 months was achieved in 12%, 42%, and 37% of patients in the medical therapy, LRYGB, and LSG groups, respectively. The remission rates, evaluated by achievement of the endpoint without the use of hypoglycemic agents, were 0%, 100%, and 37%, respectively. Mingrone et al. [19] assigned patients to undergo RYGB, biliopancreatic diversion, or standard medical therapy. After 2 years, complete remission rates of diabetes were 75% for patients who underwent RYGB and 95% for those who underwent biliopancreatic diversion, whereas no remission occurred in the medical therapy group. In contrast, diabetes remission was also observed in the conventional therapy group in the present study because these patients received intensive medical treatment at a tertiary medical center.
Obesity remains a major cause of illness and death, and bariatric surgery appears to be the only intervention that consistently results in substantial, sustained weight loss. The surgical safety of bariatric surgery is an important consideration; many physicians and the general population in Korea appreciate that bariatric surgery is a risky procedure. In our study, the postoperative mortality rate was 0.38% (one case) and the immediate postoperative complication rate was 10%. The mortality rate in our study was comparable with that of a previous report in which the 30-day death rate among patients who underwent RYGB or LAGB was 0.3% [20]. However, the reported frequencies of adverse outcomes have varied and a direct comparison was not possible. In our study, the early postoperative complication rate of 10% and the rate of 13% after 30 days were considered to be acceptable because they included minor wound complications in the early period and long-term band-related complications in the late period.
This study had several limitations. First, although about 70% of bariatric surgeries in Korea are LAGBs performed in private clinics, this study included only those performed in tertiary hospitals. However, weight loss outcomes did not differ among surgical groups. Thus, although we did not include data from private clinics, the results seem to be generalizable. Second, our study was not randomized or prospective, but was designed as a retrospective cohort study. Thus, baseline characteristics differed between groups. The surgery group was younger, female dominant, higher BMI, and more comorbidities. This is because younger female patient usually want to receive surgery, and surgeons recommend bariatric surgery for patients who have higher BMI and comorbidities. To overcome this limitation, we used various statistical methods such as matching and the GEE model to balance confounding factors at baseline between the two groups. The results of these analyses were robust. Third, long-term outcomes and complications could not be examined because of the short follow-up period.
In conclusion, bariatric surgery had a significant effect on weight loss when compared with conventional medical therapy in severely obese Korean patients. The recovery from comorbidities such as diabetes, hypertension, and dyslipidemia was better in the surgery group than in the conventional therapy group. Our results suggest that bariatric surgery may be a favorable option for treating severe obesity in Koreans. Further studies are needed to elucidate the weight loss mechanisms of bariatric surgery, improvement in comorbid diseases, and long-term outcomes of bariatric surgeries in Korea.
Figures and Tables
 | Fig. 2Percentage of weight change in surgery and conventional therapy groups in subgroup analysis in terms of body mass index (BMI) (30 ≤ BMI < 35 and BMI ≥ 35). |
Table 3
Recovery from diabetes, hypertension, and dyslipidemia in the surgery and conventional therapy groups
ACKNOWLEDGEMENTS
This study was completed as part of the health technology assessment report (project no. NA2011-003) funded by the National Evidence-based Healthcare Collaborating Agency (NECA) in Korea.
References
1. Freedman DS. Centers for Disease Control and Prevention (CDC). Obesity: United States, 1988-2008. MMWR Surveill Summ. 2011. 60:Suppl. 73–77.
2. Korea Centers for Disease Control and Prevention. Progress report on the national health and nutrition survey 2009 (health examination). 2010. Cheongwon: Korea Centers for Disease Control and Prevention.
3. Ramachandran A, Snehalatha C, Viswanathan V, Viswanathan M, Haffner SM. Risk of noninsulin dependent diabetes mellitus conferred by obesity and central adiposity in different ethnic groups: a comparative analysis between Asian Indians, Mexican Americans and Whites. Diabetes Res Clin Pract. 1997. 36:121–125.
4. Wen CP, David Cheng TY, Tsai SP, Chan HT, Hsu HL, Hsu CC, et al. Are Asians at greater mortality risks for being overweight than Caucasians? Redefining obesity for Asians. Public Health Nutr. 2009. 12:497–506.
5. Misra A. Redefining obesity in Asians: more definitive action is required from the WHO. Natl Med J India. 2004. 17:1–4.
6. Low S, Chin MC, Ma S, Heng D, Deurenberg-Yap M. Rationale for redefining obesity in Asians. Ann Acad Med Singapore. 2009. 38:66–69.
7. Lee WJ, Wang W. Bariatric surgery: Asia-Pacific perspective. Obes Surg. 2005. 15:751–757.
8. Han SM, Kim WW. The 3-year results of laparoscopic sleeve gastrectomy for the treatment of Korean morbid obesity. J Korean Surg Soc. 2007. 73:400–405.
9. 1983 metropolitan height and weight tables. Stat Bull Metrop Life Found. 1983. 64:3–9.
10. Hanley JA, Negassa A, Edwardes MD, Forrester JE. Statistical analysis of correlated data using generalized estimating equations: an orientation. Am J Epidemiol. 2003. 157:364–375.
11. Buddeberg-Fischer B, Klaghofer R, Krug L, Buddeberg C, Muller MK, Schoeb O, et al. Physical and psychosocial outcome in morbidly obese patients with and without bariatric surgery: a 4 1/2-year follow-up. Obes Surg. 2006. 16:321–330.
12. Dixon JB, Strauss BJ, Laurie C, O'Brien PE. Changes in body composition with weight loss: obese subjects randomized to surgical and medical programs. Obesity (Silver Spring). 2007. 15:1187–1198.
13. Sjostrom L, Narbro K, Sjostrom CD, Karason K, Larsson B, Wedel H, et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med. 2007. 357:741–752.
14. Adams TD, Gress RE, Smith SC, Halverson RC, Simper SC, Rosamond WD, et al. Long-term mortality after gastric bypass surgery. N Engl J Med. 2007. 357:753–761.
15. Picot J, Jones J, Colquitt JL, Gospodarevskaya E, Loveman E, Baxter L, et al. The clinical effectiveness and cost-effectiveness of bariatric (weight loss) surgery for obesity: a systematic review and economic evaluation. Health Technol Assess. 2009. 13:1–190. 215–357. iii–iv.
16. Colquitt JL, Picot J, Loveman E, Clegg AJ. Surgery for obesity. Cochrane Database Syst Rev. 2009. (2):CD003641.
17. Buchwald H, Avidor Y, Braunwald E, Jensen MD, Pories W, Fahrbach K, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004. 292:1724–1737.
18. Schauer PR, Kashyap SR, Wolski K, Brethauer SA, Kirwan JP, Pothier CE, et al. Bariatric surgery versus intensive medical therapy in obese patients with diabetes. N Engl J Med. 2012. 366:1567–1576.
19. Mingrone G, Panunzi S, De Gaetano A, Guidone C, Iaconelli A, Leccesi L, et al. Bariatric surgery versus conventional medical therapy for type 2 diabetes. N Engl J Med. 2012. 366:1577–1585.
20. Longitudinal Assessment of Bariatric Surgery (LABS) Consortium. Flum DR, Belle SH, King WC, Wahed AS, Berk P, et al. Perioperative safety in the longitudinal assessment of bariatric surgery. N Engl J Med. 2009. 361:445–454.




 ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download