Abstract
Purpose
The aim of this study was to compare the surgical completeness and outcome of total thyroidectomy in two patient groups: One treated by harmonic scalpel (HS) and one by conventional total thyroidectomy (CT).
Methods
Between March 2006 and December 2007, 104 patients had total thyroidectomy by HS and 108 patients underwent CT. We analyzed clinicopathological characteristics and stimulated serum thyroid-stimulating hormone (TSH), thyroglobulin (Tg), and anti-Tg antibodies at the time of ablation for both groups.
Results
Compared with the CT group, the HS group had shorter operating time and hospital stays and reduced postoperative drainage. At postsurgical ablation, mean serum TSH was 80.47 ± 21.77 mU/L in the HS group and 69.74 ± 21.17 mU/L in the CT group, with significant between-group differences (P < 0.001). Mean serum Tg levels after TSH stimulation were 1.57 ± 3.17 and 3.95 ± 10.14 ng/mL in the HS and CT groups, respectively, with significant between-group differences (P = 0.028).
The incidence of papillary thyroid carcinoma (PTC) is increasing worldwide, rising 2.9-fold between 1988 and 2002 in the United States [1]. It is now the most prevalent cancer in Korean women [2].
With the rising incidence of PTC, there is a need for new safe surgical techniques that require less operating time so that more patients can be treated in a timely manner.
Although the extent of thyroidectomy remains controversial, total thyroidectomy (TT) has been one of the most frequently performed operations for patients with PTC. Complete resection of the thyroid gland results in fewer loco-regional recurrences and facilitates detection of metastatic disease, both by serum thyroglobulin (Tg) evaluation and by postablation 131I whole body scan [3,4]. However, TT has more postoperative complications, such as permanent recurrent laryngeal nerve (RLN) palsy and hypoparathyroidism, than unilateral lobectomy [5]. Since development of the harmonic scalpel (HS) in the early 1990s, it has been used in thyroid surgery to ensure a dry surgical field and to satisfy the surgeon's need for surgical efficiency. The synchronous action of the HS for simultaneous cutting and coagulation of blood vessels is beneficial in reducing operating time, compared with conventional suture ligation techniques or other vessel sealing devices [6-9]. In addition, the capability of the HS to seal vessels and assure coagulation at low temperatures (between 50℃ and 100℃) results in less thermal damage to surrounding structures [10]. Previous studies have confirmed a reduction in postoperative complications after thyroidectomy with HS [11,12].
The HS was initially used in open thyroid surgery for treatment of benign or malignant thyroid disease [7]. Subsequently, it was shown to be advantageous in minimally invasive endoscopic thyroidectomy [13,14]. To date, a number of HS studies in thyroid surgery have been published. The majority of studies have shown HS to be safe and efficient in terms of perioperative complications and hemostasis and time-saving in comparison with conventional suture ligation techniques or other vessel sealing devices. However, we have assessed the impact of HS on surgical completeness in TT followed by 131I ablation of the thyroid remnant.
This study had two objectives: first, to evaluate and compare the surgical efficiency and safety of HS and conventional TT, and second, to determine if there is any distinction in surgical completeness between the two techniques. Toward that end, we measured the mean level of serum thyroid-stimulating hormone (TSH) at 131I ablation and the mean level of stimulated serum Tg. To the best of our knowledge, this is the first study that has compared the HS technique with the conventional technique with regard to surgical completeness in patients with thyroid cancer.
We retrospectively reviewed medical records of 701 consecutive patients who underwent surgery for treatment of PTC between March 2006 and December 2007 in the Department of Surgery, Yonsei University College of Medicine, by one experienced surgeon (KHN). Preoperative diagnoses of thyroid nodules were made by ultrasonographic-guided fine needle aspiration biopsy and neck computed tomography.
In October 2006, we began routine use of HS in thyroid surgery. Thus, of the 701 patients treated, 200 had conventional total thyroidectomy (CT group; from March to September 2006), and 501 had TT by use of HS (HS group; from October 2006 to December 2007).
We excluded patients who underwent less than TT, completion thyroidectomy, lateral neck node dissection, endoscopic thyroidectomy, or robotic-assisted endoscopic thyroidectomy.
In all, a total of 212 PTC patients were selected who met the following four inclusion criteria:
1) The TT was performed in our hospital.
2) 131I ablation was performed after surgery without a preliminary diagnostic 131I whole body scan.
3) Serum Tg levels in the absence of serum anti-Tg antibodies (TgAb) were determined at the time of 131I ablation when serum TSH should be above 30 mU/L, minimal criteria for optimal ablation based on American Thyroid Association (ATA) guidelines [15]. Thyroiditis patients with positive levels of TgAb were excluded from the study due to possible false reduction in measured serum Tg levels.
4) Patients had no preoperative or postoperative distant metastases.
According to ATA guidelines [15], TT is recommended in the following circumstances: 1) primary thyroid cancer >1 cm; 2) presence of contralateral thyroid nodules or regional or distant metastases; 3) history of radiation therapy to the head and neck; 4) patient has a first-degree relative with differentiated thyroid cancer; 5) age >45 years; 6) presence of extracapsular invasion or multifocality.
Of the 212 patients with PTC enrolled in this study, 104 were in the HS group and 108 in the CT group. All had prophylactic ipsilateral central compartment node dissection (CCND). In order to reduce interoperator confounding factors, all operations were performed by the same principal surgeon. The study was approved by the hospital's Institutional Review Board.
After surgery, all patients began treatment with a TSH-suppressing dose of LT4 (2 µg/kg). In the present study, radioactive iodine (RI) was given therapeutically without a diagnostic 131I whole-body scan in order to avoid a "stunning effect" (i.e., decreased uptake by a thyroid remnant of 131I after diagnostic administration of 131I) [16]. RI was administered 6 to 8 weeks after surgery when each patient was in hypothyroidism after LT4 had been withdrawn for 4 weeks. After 2 weeks on a low-iodine diet, all patients were treated with 30 mCi of RI. Patients received written instructions and were assisted by a dietician. The 131I whole body scan was done on the second day after RI treatment.
Stimulated serum Tg, serum TgAb, and serum TSH were measured at ablation. Serum TSH was measured by chemiluminescence immunoassay (Centaur; Bayer Health Care, Mannheim, Germany). Serum Tg was measured by immunoradiometric assay (Dynotest TgS, Brahms, Berlin, Germany), and, similarly, for TgAbs (Anti-Tgn RIA, Brahms). The Tg assay had a sensitivity of 0.2 ng/mL. TgAb status was considered negative when readings were <20 IU/mL.
TT is defined as total bilateral extracapsular thyroidectomy. Each patient was placed in a supine position and the neck was extended while the patient was under general anesthesia. A 5 to 6 cm transverse collar skin incision was made two fingerbreadths above the sternal notch, and the lower layer of the platysma was exposed under direct vision. Subplatysmal flap dissection was performed for achievement of adequate working space from the sternal notch to the hyoid bone level superiorly and both medial sides of the anterior border of the sternocleidomastoid muscle laterally. The midline of the strap muscle was divided vertically, and the thyroid gland was exposed. In patients assigned to the HS group, only Harmonic ACE Curved Shears (23-mm long; Johnson & Johnson Medical, Cincinnati, OH, USA) were used for vascular control of the thyroid gland. The named vessels of the superior, middle, and inferior thyroidal arteries and veins were controlled by using a low power level (70 µm vibration). Other small vessels and surrounding soft tissues were controlled by using a higher power level (100 µm vibration) for easy cutting. For patients in the conventional TT group, electrocautery was used for control of the small vessels of the gland and conventional hand-tied ligation was used for the named vessels and some arterial branches. The upper pole of the gland was divided carefully in order to avoid injury to the superior laryngeal nerves. The greatest attention was paid to identification of all of the superior and inferior parathyroid glands and to their preservation with the intact vascular pedicle. Parathyroid autotransplantation was performed as needed. Careful dissection was performed for identification of the inferior thyroid artery and the RLN in the usual anatomic relationship. The whole cervical course of the RLN was traced and the gland was then dissected from the trachea. When CCND (the prelaryngeal, pretracheal, and paratracheal area of the tumor side) was performed, while monitoring the RLN track, soft tissue and lymph nodes were removed within an area limited cranially by the hyoid bone and superior thyroid vessels, caudally by the thyro-thymic ligament area, and laterally by the medial border of the carotid artery. In the HS group, special care was taken to avoid damage to the RLN in the tracheoesophageal groove due to the collateral energy of the HS. A Jackson-Pratt closed suction drain (100 mL, 3.2 mm in diameter; Barovac Sewoon Medical, Seoul, Korea) was placed through a separate skin incision in all patients. This drain was removed when drainage decreased to less than 20 mL/day. Wounds were closed with absorbable suture material using a continuous subcutis suture method.
Based on clinical and pathologic records, a retrospective analysis was performed on numerous variables in both patient groups. These included demographic and pathological findings, operating time (from skin incision to closure), intraoperative bleeding, total amount of drainage, length of hospital stay, incidence of perioperative complications (hematoma, RLN palsy, hypoparathyroidism, seroma, other injuries), and measurement of stimulated serum Tg, serum TgAb, and serum TSH at the time of 131I ablation.
Laryngoscopy was performed preoperatively for evaluation of vocal cord mobility in all patients. Gauze pieces were weighed before and after use for estimation of the amount of intraoperative bleeding (1 g, 1 mL of blood). Postoperative calcium, phosphorus, and parathyroid hormone (PTH) levels were monitored in all patients. Hypocalcemia was defined as a serum calcium level <8.0 mg/dL, even in a single measurement. Hypocalcemic patients received supplementation therapy with oral calcium and vitamin D (calcitriol), even if asymptomatic. Supplementation therapy was gradually tapered on the basis of serum calcium and PTH measurements in the outpatient clinic. We defined transient hypocalcemia and RLN palsy based on recovery from symptoms and normalization of laboratory data within 6 months.
All data were expressed as mean ± standard deviation, proportions, or absolute numbers. We used SPSS ver. 13.0 (SPSS Inc., Chicago, IL, USA) for statistical analysis. Statistical differences between the two groups were assessed by the Student's t-test or the Mann-Whitney test for continuous variables, depending on distribution. Interarm comparisons of categorical variables were performed using the chi-square test. P < 0.05 was accepted as a significant difference.
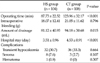
Clinicopathological findings of both groups are shown in Table 1. The groups were well matched for age and sex (P-value, not significant). There were no differences in clinicopathological findings, except for tumor size. Mean tumor size in the CT group was 1.00 ± 0.61 cm compared with 0.80 ± 0.47 cm in the HS group. Although statistically significant, the difference was clinically negligible considering that the actual difference of mean tumor size between the two groups was only about 0.2 cm and there was no difference in T stage.
Mean number of retrieved and pathologically proven metastatic central lymph nodes in the HS group were 4.41 ± 4.07 and 0.61 ± 1.68 compared with 4.27 ± 3.85 and 0.66 ± 1.56 in the CT group. The differences were not statistically significant.
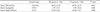
Postoperative outcomes and complications in the groups are summarized Table 2. Operating time in the two groups was statistically significant (P < 0.001): 87.73 ± 22.52 minutes in the HS group, 36.23 minutes less than for the CT group (123.96 ± 32.17 minutes). The length of hospital stay in the HS group was significantly shorter than in the CT group (P = 0.001), and the HS group had significantly less postoperative drainage (P = 0.001). There was no between-group difference in amount of intraoperative bleeding, transient hypocalcemia, seroma, and hematoma. No patient had permanent RLN palsy or hypoparathyroidism. All seromas resolved with repeated needle aspiration and compression dressings. No major hematoma formation occurred, although 1 patient in the HS group had a small hematoma, which originated from a tiny bleeder in the anterior surface of the strap muscle. The hematoma was evacuated at bedside without difficulty.
Serum levels of serum TSH, Tg, and TgAbs at the time of 131I ablation in the two groups are summarized in Table 3. At the time of 131I ablation, mean serum TSH was 80.47 ± 21.77 mU/L in the HS group and 69.74 ± 21.17 mU/L in the CT group, with significant between-group differences (P = 0.001). Mean serum Tg levels after TSH stimulation were 1.57 ± 3.17 ng/mL for the HS group and 3.95 ± 10.14 ng/mL for the CT group, with significant between-group differences (P = 0.028). There was no significant difference in serum TgAbs levels between the groups.
Surgeons who treat PTC have always been concerned with surgical and oncologic safety. Surgical safety can be defined as the best way to reduce perioperative morbidity in surgical patients. Oncologic safety can be defined as the best way to improve treatment outcome in cancer patients. Until now, most reports of use of the HS in thyroid surgery have emphasized its utility in terms of time saving and perioperative morbidity without demonstrating its oncologic safety in relation to surgical completeness. Our study included only PTC patients who underwent TT so that we could evaluate how effective the HS was in completely removing the diseased thyroid gland.
Our results show the HS was a faster surgical technique than CT, saving 36 minutes on average, consistent with most studies [6-9,11]. The shorter operating time implies the possibility for treatment of more patients in the same operative sessions. Ultimately, HS could enable significant reduction of patients awaiting surgery in Yonsei University Health System.
Unlike other studies, we did not find statistically less intraoperative bleeding in the HS group [11,17,18]. Possibly the CT group had too little intraoperative bleeding for detection of a meaningful difference between the groups. Our effort to consistently maintain a dry operative field through meticulous hemostasis in the CT group could also have made the operation easier and resulted in our favorable data.
In this study, the amount of postoperative drainage was less in the HS group than in the CT group, similar to prior reports [7,12]. The explanation is that the HS achieves efficient hemostasis and minimal tissue manipulation during surgery. The reduction in postoperative drainage after HS surgery resulted in 1-day shorter hospital stays for the HS group and related cost savings. All patients in the study were admitted to the hospital the day before surgery and were not discharged until drains were removed.
Despite our positive findings for the use of HS in thyroid surgery, the technique has drawbacks. Mallur et al. [19] reported that with prolonged activation the HS generates considerable residual heat that can lead to unintended burning of adjacent tissue and skin. In addition, to avoid permanent complications, a safety margin of 3 to 5 mm is required between the active curved blade and the RLN and parathyroid glands [20]. It is recommended that the inactive blade be the nearest tip to the nerve during cutting and coagulation. In our study, we found no statistical difference in complication rates between the two groups. Of particular importance, there were no cases with permanent RLN palsy or permanent hypoparathyroidism. We attribute this result to our use of HS in thyroid surgery only after initial training and overcoming the learning curve of a surgeon's adaption.
Although the extent of thyroidectomy in PTC patients is still under debate, Mazzaferri [4] reported that TT was the best operation in terms of oncologic safety. Most PTC patients have TT followed by 131I ablation of the thyroid remnant, resulting in fewer recurrences, improved survival, and easier follow-up. Nevertheless, the current opinion is that, despite surgeons' best efforts, TT is rarely achievable. Microscopic or macroscopic thyroid remnants almost always remain and 131I treatment is usually necessary for ablation of the remnants [21].
In the present study, we found that at 131I ablation, patients in the HS group had higher serum TSH levels and lower serum Tg levels than patients in the CT group. Theoretically, TSH stimulation of thyroid cells is required for optimal imaging with 131I, because elevated TSH stimulates radioiodine uptake in residual thyroid tissue and thyroid carcinoma. Therefore, the HS appears to maximize the effect of 131I ablation by effectively raising TSH levels more than conventional TT. Serum Tg level reflects the size of the thyroid remnant. One gram of thyroid tissue releases approximately 1 ng/mL of Tg when TSH is <0.1 mU/L and there is a >3-fold increase in serum Tg values following TSH stimulation [22]. On the basis of this theory, mean off Tg levels in the HS and CT groups are 1.57 ng/mL and 3.95 ng/mL, respectively, which can be calculated to represent approximately 0.52 g of thyroid remnant in the HS group and 1.32 g of thyroid remnant in the CT group, respectively. Either is within an acceptable range because 131I ablation treatment with 30 mCi (1100 MBq), the protocol used in our hospital, usually destroys the thyroid remnant, providing that it is <2 to 3 g [4]. Therefore, the HS provided PTC patients with surgical completeness in that the optimal treatment goal is to eliminate all malignant thyroid tissue.
We questioned why patients in the HS group showed higher serum TSH levels and lower serum Tg levels at 131I ablation than those in the CT group. We speculate that a considerable amount of residual heat (between 50℃ and 100℃) generated by the HS may be transmitted to the microscopic thyroid remnant, which may have an additional intraoperative ablative effect on remnant thyroid tissue by denaturing proteins. Eventually, the intraoperative ablation effect by the HS minimizes the amount of thyroid remnant and enhances the efficacy of 131I ablation treatment by increasing TSH levels and decreasing Tg levels.
The present study had several limitations. The sample size was relatively small, and our study included only the short-term follow-up outcome because our goal was primarily to evaluate the surgical completeness of the HS technique. The short-term follow-up data for evaluating the effect by HS make assertions about surgical completeness and oncologic safety unclear. Therefore, large-scale randomized trials and long-term follow-up data are required to confirm our findings before definitive conclusions can be made.
In conclusion, TT using the HS is a relatively safe and efficient technique for use in PTC patients. In addition, the HS provides surgical completeness and a beneficial effect on successful ablation.
Figures and Tables
References
1. Davies L, Welch HG. Increasing incidence of thyroid cancer in the United States, 1973-2002. JAMA. 2006. 295:2164–2167.
2. Minister of Health & Welfare. Cancer incidence in Korea 1999-2001. 2005. Seoul: Minister of Health & Welfare.
3. Esnaola NF, Cantor SB, Sherman SI, Lee JE, Evans DB. Optimal treatment strategy in patients with papillary thyroid cancer: a decision analysis. Surgery. 2001. 130:921–930.
4. Mazzaferri EL. An overview of the management of papillary and follicular thyroid carcinoma. Thyroid. 1999. 9:421–427.
5. Bergamaschi R, Becouarn G, Ronceray J, Arnaud JP. Morbidity of thyroid surgery. Am J Surg. 1998. 176:71–75.
6. Ortega J, Sala C, Flor B, Lledo S. Efficacy and cost-effectiveness of the UltraCision harmonic scalpel in thyroid surgery: an analysis of 200 cases in a randomized trial. J Laparoendosc Adv Surg Tech A. 2004. 14:9–12.
7. Voutilainen PE, Haapiainen RK, Haglund CH. Ultrasonically activated shears in thyroid surgery. Am J Surg. 1998. 175:491–493.
8. Kang SK, Kunanandam T, Clark L. Prospective, case-control study of surgical efficiency of ultrasonic shear ('harmonic scalpel') thyroidectomy compared with conventional thyroidectomy. J Laryngol Otol. 2008. 122:1194–1196.
9. Koh YW, Park JH, Lee SW, Choi EC. The harmonic scalpel technique without supplementary ligation in total thyroidectomy with central neck dissection: a prospective randomized study. Ann Surg. 2008. 247:945–949.
10. Bandi G, Wen CC, Wilkinson EA, Hedican SP, Moon TD, Nakada SY. Comparison of blade temperature dynamics after activation of Harmonic Ace scalpel and the Ultracision Harmonic Scalpel LCS-K5. J Endourol. 2008. 22:333–336.
11. Cordon C, Fajardo R, Ramirez J, Herrera MF. A randomized, prospective, parallel group study comparing the Harmonic Scalpel to electrocautery in thyroidectomy. Surgery. 2005. 137:337–341.
12. Miccoli P, Berti P, Dionigi G, D'Agostino J, Orlandini C, Donatini G. Randomized controlled trial of harmonic scalpel use during thyroidectomy. Arch Otolaryngol Head Neck Surg. 2006. 132:1069–1073.
13. Miccoli P, Berti P, Ambrosini CE. Perspectives and lessons learned after a decade of minimally invasive video-assisted thyroidectomy. ORL J Otorhinolaryngol Relat Spec. 2008. 70:282–286.
14. Koh YW, Park JH, Kim JW, Lee SW, Choi EC. Clipless and sutureless endoscopic thyroidectomy using only the harmonic scalpel. Surg Endosc. 2010. 24:1117–1125.
15. American Thyroid Association (ATA) Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid Cancer. Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, et al. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2009. 19:1167–1214.
16. Morris LF, Waxman AD, Braunstein GD. Thyroid stunning. Thyroid. 2003. 13:333–340.
17. Meurisse M, Defechereux T, Maweja S, Degauque C, Vandelaer M, Hamoir E. Evaluation of the ultracision ultrasonic dissector in thyroid surgery: prospective randomized study. Ann Chir. 2000. 125:468–472.
18. Ecker T, Carvalho AL, Choe JH, Walosek G, Preuss KJ. Hemostasis in thyroid surgery: harmonic scalpel versus other techniques--a meta-analysis. Otolaryngol Head Neck Surg. 2010. 143:17–25.
19. Mallur PS, Jethanamest D, Shemen LJ. Potential hazards of the harmonic scalpel. Otolaryngol Head Neck Surg. 2009. 141:303–304.
20. Manouras A, Markogiannakis HE, Kekis PB, Lagoudianakis EE, Fleming B. Novel hemostatic devices in thyroid surgery: electrothermal bipolar vessel sealing system and harmonic scalpel. Expert Rev Med Devices. 2008. 5:447–466.
21. Wartofsky L, Sherman SI, Gopal J, Schlumberger M, Hay ID. The use of radioactive iodine in patients with papillary and follicular thyroid cancer. J Clin Endocrinol Metab. 1998. 83:4195–4203.
22. Spencer CA, LoPresti JS, Fatemi S, Nicoloff JT. Detection of residual and recurrent differentiated thyroid carcinoma by serum thyroglobulin measurement. Thyroid. 1999. 9:435–441.




 ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download