Abstract
Purpose
Hepatobiliary surgery has changed dramatically in recent decades with the advent of laparoscopic techniques. The aim of this retrospective study was to compare survival rates according to stages, adjusting for important prognostic factors.
Methods
A retrospective study of a 17-year period from January 1994 to April 2011 was carried out. The cases studied were divided into two time period cohorts, those treated in the first 9-years (n = 109) and those treated in the last 7-years (n = 109).
Results
An operation with curative intent was performed on 218 patients. The 5-year survival rates according to the depth of invasion were 86% (T1), 56% (T2), 45% (T3), and 5% (T4). The number of cases of incidental gallbladder cancer found during 3,919 laparoscopic cholecystectomies was 96 (2.4%). Incidental gallbladder cancer revealed a better survival rate (P = 0.003). Iatrogenic bile spillage was found in 20 perforations of the gallbladder during laparoscopic cholecystectomies, 16 preoperative percutaneous transhepatic gallbladder drainages and 16 percutaneous transhepatic biliary drainages; only percutaneous transhepatic biliary drainage patients showed a significantly lower survival rate than patients without iatrogenic bile spillage (P < 0.034). Chemoradiation appeared to improve overall survival (P < 0.001). Multivariate analysis also revealed that time period, type of surgery, surgical margin, lymphovascular invasion, lymph node involvement, and chemoradiation therapy had significant effects.
The incidence of gallbladder cancer (GBC) shows wide racial and geographical variation, and some genetic and environmental factors have been suggested with regards to etiologic association in the development of GBC. These factors include gallstones, presence of chronic inflammation, adenoma, anomalous pancreatobiliary duct union, sex, age, obesity, and parity. The incidence of GBC is high in Korea, Japan, and Central and Eastern European countries [1]. GBC is an uncommon cancer that has traditionally been associated with a poor prognosis. This poor prognosis is considered to be related to advanced stage at diagnosis, which is due to both the anatomic position of the gallbladder, and the vagueness and non-specificity of symptoms. In the era of laparoscopic cholecystectomy (LC), incidental GBC has dramatically increased and is now the major way patients present with GBC [2,3]. In many cases, the diagnosis is made after a cholecystectomy has been performed and an incidental tumor is identified in the specimen. Frozen section diagnosis is often challenging and has its own limitations because of sampling problems and freezing artifacts [4]. The risk of peritoneal seeding caused by inadvertent spillage of cancer contaminated bile during percutaneous transhepatic gallbladder drainage (PTGBD) and percutaneous transhepatic biliary drainage (PTBD) may be high, but has rarely been reported [5]. GBC is a fatal disease that can only be cured by radical surgical resection. The goal of radical resection should be cholecystectomy with en bloc resection of the invaded organs (most commonly the liver) around the tumor to provide reasonable margins and to resect regional lymph nodes. However, there is still a debate about the extent of hepatic resection and the extent of regional lymphadenectomy [6,7].
The aim of this retrospective study was to compare survival rates according to tumor stages, using Cox regression comparison of survival by stage adjusting for important prognostic factors.
A retrospective study spanning a 17-year period from January 1994 to April 2011 was performed, and 218 consecutive inpatients were identified. Cases were divided into two time-period cohorts: those treated in the first 9 years (n = 109) and those treated in the last 7 years (n = 109). Survival analysis was performed considering patient variables (age and gender), operative variables (LC only, LC with conversion open cholecystectomy, radical second resection, primary open cholecystectomy, and hemi-hepatectomy), incidentality, iatrogenic bile spillage, chemoradiation, and pathologic variables (T-stage, histologic type, degree of differentiation, surgical margin status, lympho vascular invasion, perineural invasion, and lymph node involvement). Our standard radical operative procedure was extended cholecystectomy (cholecystectomy plus partial resection of approximately 2 cm from the gallbladder bed) with lymph node dissection in the hepatoduodenal ligament, skeletonizing the portal vein and hepatic artery. Hemi-hepatectomy has also been described by the Couinaud segments resected. After exploratory surgery, opening the gallbladder on the back table and identifying the type of disease that is present, as well as intraoperative frozen sections, were also performed in all except four cases. Clinical staging of the disease was according to the American Joint Committee on Cancer (AJCC) staging system (7th edition). We recommended additional surgery when the tumor stage was over T2 (tumor invades the perivascular connective tissue). Adjuvant therapy after surgical resection was not strictly protocol driven and was administered at the discretion of surgeons and oncologists during the treatment of patients. When the resection margin was positive for tumor infiltration and the patient refused an additional second operation, chemoradiation therapy to the tumor bed was performed. Patients were regularly followed up in the outpatient clinic every 3 to 6 months.
Data were summarized using descriptive statistics that included frequency and percentage for categorical variables and mean ± standard deviation for continuous variables. Differences in patient demographic and clinical characteristics were compared across subgroups using the chi-square test for categorical variables and analysis of variance for continuous variables. Overall survival (OS; defined as the time from date of surgery to death) was estimated using Kaplan-Meier curves. Survival curves were compared between groups using the log-rank test. Univariate analyses of prognostic factors were performed using Cox regression to examine differences with respect to OS. The potential prognostic factors considered are shown in Tables 1 and 2. Multivariate analyses using Cox regression were performed to identify prognostic factors independently related to OS. Cox regression was used to assess the difference between groups adjusting for significant prognostic factors. In particular, the main analysis addressing the primary objective was a Cox regression comparison of OS by stage, adjusting for important prognostic factors. All P-values < 0.05 were considered statically significant. This study was explorative and therefore no adjustment for multiple testing was applied. All statistical analyses were carried out using SAS 9.1.3 (SAS Institute Inc., Cary, NC, USA) and R 2.9.2 (R Foundation for Statistical Computing, Vienna, Austria) statistical software.
Between January 1994 and April 2011, 218 patients underwent evaluation and surgical treatment for adenocarcinoma of gallbladder. There was no postoperative death. Median age was 63 years (range, 35 to 90 years) and 123 patients were female (56%). The stage of the GBC was T1 in 53 (24%) patients, T2 in 97 (45%) patients, T3 in 49 (23%), and T4 in 19 (9%) patients.
The stage of disease at presentation affected the survival in all time periods. The 5-year estimated survival rates of patients according to the depth of invasion were: stage I (estimated survival rates limited to mucosa, muscularis, 86%; 95% confidence interval [CI], 0.73 to 0.94; P < 0.0001), stage II (subserosa, 56%; 95% CI, 0.44 to 0.66), stage III (serosa, 45%; 95% CI, 0.31 to 0.6), and stage IV (serosa with invasion to adjacent organs, 5%; 95% CI, 0.01 to 0.29).
Table 1 shows the distribution of patients by stage and time period. The notable change in tumor stage during the late period increased in the frequency of patients diagnosed with stage I and II and decreased in stage III and IV disease (Fig. 1). Overall median survival improved comparing early and late periods (Fig. 2). LC operations were more frequently performed in the late period and appeared to result in the earlier discovery of GBC, resulting in increased probability of survival.
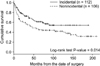
During the 17-year period evaluated in this study, 3,919 LCs were performed, of which 96 (2.4%) cases of GBC were incidentally discovered, and GBC was found incidentally in 112 of the 218 patients (50%) by permanent histological examination. Eighty nine (89%) of those patients whose GBC was found incidentally were stage T1 or T2. Patients who were found to have GBC incidentally at LC had a significant increase in survival when compared with those who were admitted electively with a known diagnosis (P = 0.014) (Fig. 3).
Due to biliary colic, acute cholecystitis, cholangitis, choledocholithiasis, and gallstone pancreatitis, 16 patients had PTGBD, and 16 had PTBD with or without endoscopic sphincterotomy for the clearance of common bile duct stones prior to surgery. Gallbladder perforation during LC was found in 20 out of 218 patients (9%). Comparison of OS according to incidence of bile leakage, iatrogenic bile spillage group (20 intraoperative bile leakage, 16 PTGBD, and 16 PTBD) demonstrated significantly worse survival (P = 0.021) (Fig. 4).
The procedures performed as resection with curative intent included 11 (5%) major liver resection (≥hemihepatectomy) and 111 (51%) primary open cholecystectomy. Twenty nine patients (13%) were noted to have GBC during the laparoscopic procedures and were converted to open surgery. Four patients (2%) with histologically proven GBC after LC underwent potentially curative resection, whereas 63 (29%) underwent LC only. In the LC only group, 55 patients (87%) were early stage (T1, T2) and, in the primary open cholecystectomy group, 47 patients (42%) were late stage (T3, T4). In T1 and T2 comparison of 5-year OS according to type of surgery (LC only vs. radical LC), there were no statistically significant differences (T1, P = 0.502; T2, P = 0.216). In comparison of 5-year survival according to type of surgery (five categories), better survival was seen in re-open after LC (radical second resection) and LC plus conversion during the laparoscopic procedures (conversion open cholecystectomy). On the other hand, primary open cholecystectomy and hemihepatectomy showed poor survival (P = 0.0001).
The distribution of histologic subtypes in the current report was similar to that reported from other centers, in which adenocarcinoma predominated (adenocarcinoma, 97%; adenosquamous, 1%; squamous, 1%). The majority of tumors were well differentiated (64%), 28% were moderately differentiated, and the remaining 7% were poorly differentiated. The T-stage of disease correlated with the likelihood of lymph node involvement, lymphovascular and perineural invasion, and surgical margin status. Of note, 34 cases (16%) involved regional lymph nodes, 56 (26%) exhibited perineural invasion, and 58 (27%) lymphovascular invasion, whereas 29 cases (13%) were surgical margin positive histologically.
A total of 73 patients (34%) underwent adjuvant chemotherapy and 62 patients (28%) underwent adjuvant chemotherapy with radiation, whereas the remaining 83 (38%) did not receive adjuvant therapy. Patients received a variety of doses and number of cycles of chemotherapy regimens and chemoradiation with fluorouracil and gemcitabine hydrochloride, which were the standard of care given to most patients. The chemotherapy alone group demonstrated a statistically significant improvement in survival than the no therapy or chemoradiation groups (P = 0.005) (Fig. 5).
We examined the prognostic significance of the following factors: sex, age, T-stage, year of surgery, surgery type, incidentality, iatrogenic bile spillage, histologic type, differentiation of tumor, lymphovascular invasion, perineural invasion, lymph node involvement, surgical margin status, and postoperative chemoradiation therapy for patients who underwent resection with curative intent. These clinical and pathologic variables are summarized in Tables 1 and 2. The results of univariative and multivariative analysis for the factors that significantly influenced the survival are summarized in Table 3. In univariate analyses, stage, year of surgery performed, type of surgery, incidentality, intervention, differentiation, surgical margin, lymphovascular, perineural invasion, lymphnode, and chemotherapy statistically affected OS. The hazard ratio (HR) for OS in the late stage patients compared with that in the early stage patients was 2.61 (P < 0.0001; 95% CI, 1.75 to 3.89). Comparing male and female patients, there was no significant difference on survival (P = 0.98). The multivariate model was created using a backward elimination method, and the probability was set at 0.10 for removal. HRs and 95% CIs were calculated for death. In a multivariate analysis for OS, Cox models including all main effects were considered. A Cox model including year of surgery performed, type of surgery, surgical margin, lymphovascular, lymph node, and chemotherapy showed significant main effects.
The advent of LC has lowered the threshold for symptomatic patients with gallbladder disease. It appears possible that if gallbladder disease in general is operated on earlier, incidental GBCs may also be detected at an earlier stage, increasing the chance for survival.
As increasing numbers of LCs are being performed, their role in the management of potentially malignant disease must be carefully examined. LC should not be performed when GBC has been diagnosed or is suspected preoperatively [8,9]. On the other hand, LC is now performed by surgeons with a reasonable degree of confidence, even in cases of possible malignant lesions [2,10]. GBC has one of the poorest OS rates of all the gastrointestinal malignancies. The dismal results are due to the aggressive biology of this tumor [11].
In a review of the literature, GBC was suspected preoperatively in only 30% of patients and, in the remaining 70% of cases, GBC was incidentally discovered by the attending pathologist [3]. In our series, 80% of the patients that were found incidentally were stage I or II, and OS improved in the later period (2004 to 2011). Patients found to have GBC incidentally at LC had significant increased survival when compared with those who were admitted electively with a known diagnosis. Large quantities of viable tumor cells in the bile that spill out during the operation or perioperatively undoubtedly indicate the actual threat of implantation metastasis by the spilled bile. Spillage of tumor-laden bile may be a cause of port site/peritoneal recurrence following LC. Bile spillage and injuries to the biliary system occur more often during the laparoscopic procedure than during the conventional open method, and can convert potentially curable GBC to an incurable disease [12]. Thus, patients with preoperative findings suspicious for GBC should undergo open exploration with an intent to perform a radical cancer operation as a primary procedure if the diagnosis is confirmed intraoperatively [8,12].
Increasing numbers of reports have documented that mean survival is statistically shorter when complications (gallbladder perforation, injury to common bile duct, or tumor violation) occur during LC for GBC. It is thought that in addition to perioperative bile leak, factors such as the biological properties of the tumor, tumor stage, operative maneuvers and impact of pneumoperitoneum pressure may be involved in the onset of peritoneal and port site recurrence [9].
Recently, the single port LC technique was reported to also increase the risk of bile leakage into the abdomen because of "critical view of safety" [13]. It is undoubtedly a consequence of cancer-contaminated bile spillage through the liver pores created by PTGBD or PTBD, and subsequent cancer growth on the peritoneum [5]. In the current study, 20 biliary leakage incidences were reported during LC, 16 during PTGBD, and 16 during PTBD, only PTBD patients showed significantly worse survival.
Complete surgical resection is the only potential curative treatment of GBC. If GBC is suspected preoperatively, an open cholecystectomy should be performed to enable a complete evaluation and radical resection [14].
Controversy still remains as to whether laparotomy and local additional excision should be performed when a diagnosis of GBC is made during or after LC, and some groups recommended radical surgery [15-17], while others have come to the conclusion that further surgical intervention offers no advantage [18].
At our institution, early tumors (T1s or T1a) that are recognized incidentally are curable with simple cholecystectomy alone. Also, extended cholecystectomy is not evidence-based in patients with T1b GBC. After postoperative diagnosis of incidental over T2 GBC, there is a need for a second radical procedure. In advanced GBC, radical surgery can cure only a small subset of patients. In our series, radical second resection showed statistically better survival, whereas hemihepatectomy showed worse prognosis.
It is impossible to diagnosis the T stage of GBC precisely before histological confirmation, even if the best diagnostic modalities are employed. Also, frozen biopsies have limited accuracy for the T staging of GBC because of sampling error and freezing artifacts. Sometimes frozen tissue diagnosis and the final diagnosis are not identical [4,14].
Patients found to have GBC incidentally during LC appear to have a survival advantage if resected with curative intent. There have been suggestions that prognosis after two operations is less favorable than for patients treated with a single procedure [19]. Also, if GBC is diagnosed postoperatively after LC, only about one-third of patients eventually undergo a second procedure after LC for GBC [7,20].
Recently, some reports showed the feasibility and safety of total laparoscopic completion radical cholecystectomy for incidentally detected early GBC [21,22]. The magnitude of partial hepatectomy in terms of number of excised nodes and integrity of the specimen did not differ between the open and laparoscopic approach [23]. Larger and prospective studies are needed to support the oncologic safety and efficacy of laparoscopic completion radical surgery in early GBC.
Features of GBC are characterized by a wide range of tumor extent, cancer stage-dependent survival and extent of standard resection are not yet established. Tumor-node-metastasis stage was found to be a significant prognostic factor. The prognosis worsened with increasing disease stage and the survival rate decreased with increasing age, especially after the age of 75 [24]. Our study demonstrated a similar result, but the age factor did not influence survival rate.
No consensus regarding the optimal extent of liver resection has been established. In our series, we obtained 2 to 3 cm of negative margin for the standard resection. Perineural invasion also has been reported as a factor responsible for poor prognosis [9,25]. Also, lymph node micrometastasis has a significant survival impact in patients with GBC [26]. The results of the current study are similar to previous publication from other centers [27,28].
The effectiveness of a radical surgical approach for GBC has been the subject of a number of reports. When considering the optimal operation for GBC, there are two major issues: the extent of hepatic resection and the extent of regional lymphadenectomy. Extended lymphadenectomy may prolong survival in selected patients with GBC, but the extent of lymph node resection for the optimal treatment of GBC has not been clearly established [15,27]. The AJCC suggests a minimum of three lymph nodes need to be assessed for appropriate pathologic nodal staging of GBC, and there are no established standards. Investigators from Western centers rely on limited nodal dissection involving hepato-duodenal ligament, while those from the East recommend extended lymphadenectomy including pericholedochal, periportal, common hepatic, peripancreatic, and paraaortic lymph nodes, even if overt nodal metastasis is absent.
This difference in surgical approaches has led to higher lymph nodal yield reported in Eastern studies compared to Western studies [26,28]. Lymph node dissection at our institution involves complete portal dissection, skeletonization of the biliary tree, hepatic artery and portal vein, and the pericholedochal and retropancreatic lymph nodes those are the most frequently involved nodal basins. Optimal extent of lymph node dissection for the GBC should be decided keeping in mind various factors including the patients' general condition and tumor stage.
Complete surgical resection is the only potential curative treatment. The role of chemotherapy and radiation therapy in the management of GBC remains undefined. A better understanding of the pathogenesis of the disease is needed to develop a more effective targeted adjuvant therapy [29,30]. The heterogenecity of the patient and the regimen used makes it difficult to extrapolate any conclusion. In our series, after adjusting for the stage parameters, the data supported the view that adjuvant chemoradiotherpy might improve OS for patients with GBC. The main limitation of this study was its retrospective, nonrandomized, short follow-up period, which prevented survival curve analysis. On the other hand, by comparing outcomes in the later 7 years to those in the first 9 years, we used historical controls as a reference point for the new surgical approach. The main drawback to this type of comparison is that it is possible that the overall management of these patients has changed over time and is variable among surgeons, irrespective of surgical factors.
In conclusion, the stage of disease at presentation affected the survival in all time periods. It is most likely that tumor biology and tumor stage, rather than extent of hepatectomy, determine long-term prognosis. Complete surgical resection is the only potentially curative treatment. Heightened awareness of the possibility of GBC and the knowledge of appropriate management are important for surgeons practicing LC. Early diagnosis, appropriate surgical resection, and better adjuvant therapy will be key factors in improving results in the future.
Figures and Tables
 | Fig. 4Comparison of overall survival according to iatrogenic bile spillage. PTGBD, percutaneous transhepatic gallbladder drainage; PTBD, percutaneous transhepatic bile duct drainage. |
References
1. Konstantinidis IT, Deshpande V, Genevay M, Berger D, Fernandez-del Castillo C, Tanabe KK, et al. Trends in presentation and survival for gallbladder cancer during a period of more than 4 decades: a single-institution experience. Arch Surg. 2009. 144:441–447.
2. Goetze T, Paolucci V. Does laparoscopy worsen the prognosis for incidental gallbladder cancer? Surg Endosc. 2006. 20:286–293.
3. Shih SP, Schulick RD, Cameron JL, Lillemoe KD, Pitt HA, Choti MA, et al. Gallbladder cancer: the role of laparoscopy and radical resection. Ann Surg. 2007. 245:893–901.
4. Yokomizo H, Yamane T, Hirata T, Hifumi M, Kawaguchi T, Fukuda S. Surgical treatment of pT2 gallbladder carcinoma: a reevaluation of the therapeutic effect of hepatectomy and extrahepatic bile duct resection based on the long-term outcome. Ann Surg Oncol. 2007. 14:1366–1373.
5. Tanaka N, Nobori M, Suzuki Y. Does bile spillage during an operation present a risk for peritoneal metastasis in bile duct carcinoma? Surg Today. 1997. 27:1010–1014.
6. D'Angelica M, Dalal KM, DeMatteo RP, Fong Y, Blumgart LH, Jarnagin WR. Analysis of the extent of resection for adenocarcinoma of the gallbladder. Ann Surg Oncol. 2009. 16:806–816.
7. Goetze TO, Paolucci V. Adequate extent in radical re-resection of incidental gallbladder carcinoma: analysis of the German Registry. Surg Endosc. 2010. 24:2156–2164.
8. Weiland ST, Mahvi DM, Niederhuber JE, Heisey DM, Chicks DS, Rikkers LF. Should suspected early gallbladder cancer be treated laparoscopically? J Gastrointest Surg. 2002. 6:50–56.
9. Kondo S, Takada T, Miyazaki M, Miyakawa S, Tsukada K, Nagino M, et al. Guidelines for the management of biliary tract and ampullary carcinomas: surgical treatment. J Hepatobiliary Pancreat Surg. 2008. 15:41–54.
10. Ouchi K, Mikuni J, Kakugawa Y. Organizing Committee, The 30th Annual Congress of the Japanese Society of Biliary Surgery. Laparoscopic cholecystectomy for gallbladder carcinoma: results of a Japanese survey of 498 patients. J Hepatobiliary Pancreat Surg. 2002. 9:256–260.
11. Vollmer CM, Drebin JA, Middleton WD, Teefey SA, Linehan DC, Soper NJ, et al. Utility of staging laparoscopy in subsets of peripancreatic and biliary malignancies. Ann Surg. 2002. 235:1–7.
12. Vollmer CM Jr. Unexpected identification of gallbladder carcinoma during cholecystectomy. J Gastrointest Surg. 2009. 13:2034–2036.
13. Allemann P, Schafer M, Demartines N. Critical appraisal of single port access cholecystectomy. Br J Surg. 2010. 97:1476–1480.
14. Sikora SS, Singh RK. Surgical strategies in patients with gallbladder cancer: nihilism to optimism. J Surg Oncol. 2006. 93:670–681.
15. Lee BS, Kim DH, Chang YS, Kang JH, Lee TS, Han JG. Radical reresection for T2 gallbladder cancer patients diagnosed following laparoscopic cholecystectomy. J Korean Surg Soc. 2010. 78:398–404.
16. Goetze TO, Paolucci V. Benefits of reoperation of T2 and more advanced incidental gallbladder carcinoma: analysis of the German registry. Ann Surg. 2008. 247:104–108.
17. Wakai T, Shirai Y, Hatakeyama K. Radical second resection provides survival benefit for patients with T2 gallbladder carcinoma first discovered after laparoscopic cholecystectomy. World J Surg. 2002. 26:867–871.
18. Toyonaga T, Chijiiwa K, Nakano K, Noshiro H, Yamaguchi K, Sada M, et al. Completion radical surgery after cholecystectomy for accidentally undiagnosed gallbladder carcinoma. World J Surg. 2003. 27:266–271.
19. Fong Y, Jarnagin W, Blumgart LH. Gallbladder cancer: comparison of patients presenting initially for definitive operation with those presenting after prior noncurative intervention. Ann Surg. 2000. 232:557–569.
20. Pawlik TM, Gleisner AL, Vigano L, Kooby DA, Bauer TW, Frilling A, et al. Incidence of finding residual disease for incidental gallbladder carcinoma: implications for re-resection. J Gastrointest Surg. 2007. 11:1478–1486.
21. Belli G, Cioffi L, D'Agostino A, Limongelli P, Belli A, Russo G, et al. Revision surgery for incidentally detected early gallbladder cancer in laparoscopic era. J Laparoendosc Adv Surg Tech A. 2011. 21:531–534.
22. Gumbs AA, Hoffman JP. Laparoscopic radical cholecystectomy and Roux-en-Y choledochojejunostomy for gallbladder cancer. Surg Endosc. 2010. 24:1766–1768.
23. Cho JY, Han HS, Yoon YS, Ahn KS, Kim YH, Lee KH. Laparoscopic approach for suspected early-stage gallbladder carcinoma. Arch Surg. 2010. 145:128–133.
24. Kayahara M, Nagakawa T. Recent trends of gallbladder cancer in Japan: an analysis of 4,770 patients. Cancer. 2007. 110:572–580.
25. Yamaguchi R, Nagino M, Oda K, Kamiya J, Uesaka K, Nimura Y. Perineural invasion has a negative impact on survival of patients with gallbladder carcinoma. Br J Surg. 2002. 89:1130–1136.
26. Sasaki E, Nagino M, Ebata T, Oda K, Arai T, Nishio H, et al. Immunohistochemically demonstrated lymph node micrometastasis and prognosis in patients with gallbladder carcinoma. Ann Surg. 2006. 244:99–105.
27. Jensen EH, Abraham A, Jarosek S, Habermann EB, Al-Refaie WB, Vickers SA, et al. Lymph node evaluation is associated with improved survival after surgery for early stage gallbladder cancer. Surgery. 2009. 146:706–711.
28. Negi SS, Singh A, Chaudhary A. Lymph nodal involvement as prognostic factor in gallbladder cancer: location, count or ratio? J Gastrointest Surg. 2011. 15:1017–1025.
29. Andre T, Reyes-Vidal JM, Fartoux L, Ross P, Leslie M, Rosmorduc O, et al. Gemcitabine and oxaliplatin in advanced biliary tract carcinoma: a phase II study. Br J Cancer. 2008. 99:862–867.
30. Gold DG, Miller RC, Haddock MG, Gunderson LL, Quevedo F, Donohue JH, et al. Adjuvant therapy for gallbladder carcinoma: the Mayo Clinic Experience. Int J Radiat Oncol Biol Phys. 2009. 75:150–155.




 ePub
ePub Citation
Citation Print
Print








 XML Download
XML Download