Abstract
Purpose
Consensus for endoscopic retrograde cholangiopancreatography (ERCP) related perforation management is lacking. We aimed to identify candidate patients for conservative management by examining treatment results and to introduce a simple, algorithm-based management guideline.
Methods
A retrospective review of 53 patients with ERCP-related perforation between 2000 and 2010 was conducted. Data on perforation site (duodenum lateral wall or jejunum, type I; para-Vaterian, type II), management method, complication, mortality, hospital stay, and hospital cost were reviewed. Comparative analysis was done according to the injury types and management methods.
Results
The outcome was greater
in the conservative group than the operative group with shorter hospital stay (20.6 days vs. 29.8 days, P = 0.092), less cost (10.6 thousand United States Dollars [USD] vs. 19.9 thousand USD, P = 0.095), and lower morbidity rate (22.9% vs. 55.6%, P = 0.017). Eighty-one percent (17/21) of type I injuries were operatively managed and 96.9% (31/32) of type II injuries were conservatively managed. Between the types, type II showed better results over type I with shorter hospital stay (19.3 days vs. 30.6 days, P = 0.010), less cost (9.5 thousand USD vs. 20.1 thousand USD, P = 0.028), and lower complication rate (18.8% vs. 57.1%, P = 0.004). There was no difference in mortality.
Conclusion
Type II injuries were conservatively manageable and demonstrated better outcomes than type I injuries. The management algorithm suggests conservative management in type II injuries without severe peritonitis or unsolved problem requires immediate surgical correction, including operative management in type I injuries unless endoscopic intervention is possible. Conservative management offers socio-medical benefits. Conservative management is recommended in well-selected patients.
Endoscopic retrograde cholangiopancreatography (ERCP) was first introduced in 1968 by McCune et al. [1], and has evolved over the decades. Currently, it is a valuable, widely used diagnostic and therapeutic tool in hepato-biliary-pancreas diseases. However, ERCP has a relatively high complication rate of nearly 10% and a mortality rate of 0.1 to 1% [2,3]. As therapeutic aspects of ERCP are becoming more important and endoscopists take on increasingly more complex cases, the risk of complication is increasing. Although pancreatitis, cholangitis, and hemorrhage are more frequent ERCP complications [3,4], ERCP-related perforation is one of the most feared, due to its potentially lethal nature.
The reported perforation incidence is 0.3 to 2.0% [3,5-9], and the mortality rate is 12 to 25% [2,3,9-11]. Hazardous as it is, appropriate management of ERCP-related perforation is essential to avoid detrimental outcome. Surgical management was considered the standard management of perforations. Many authors advocated early surgical management for ERCP-related perforations [8,9,12]. Most recent studies, however, indicate that carefully selected patients may recover uneventfully with conservative management alone [10,11,13-17]. Many treatment guidelines are being proposed [10,11,16-18], but a consensus has not been reached. To establish a consensual guideline with appropriate validation, a randomized controlled trial (RCT) is preferable; however, RCTs for ERCP-related perforation are unlikely due to ethical problems. Therefore, detailed analyses of large-scale case series are a better alternative.
This study aimed to identify patients who may be managed conservatively by examining the ERCP perforation treatment results. At the same time, we aimed to establish a simple ERCP perforation management guideline with a management algorithm based on a review of 53 cases.
From January 2000 to December 2010, 8,381 ERCP procedures were done at a tertiary referral center in Seoul, Korea. During that period 53 ERCP-related perforations (0.63%) occurred. The 53 patients were managed according to the management guideline at Seoul National University Hospital. Surgical indications were: 1) remaining problem unsolved by endoscopic procedure that requires immediate correction, such as retained hardware or biliary stone failed to be removed during ERCP; 2) duodenum lateral wall or jejunum injury without possibility of minimal leakage through adhesions or interventions (jejunum was included because of relatively high incidence of altered anatomy due to gastrojejunostomy in Korea); and 3) initial or subsequent symptoms/signs of severe sepsis/peritonitis. Patients with one or more of these indications underwent surgical management, and patients without any of the above were managed conservatively.
Conservative management consisted of antibiotics administration, non-per oral, parenteral nutritional support, and percutaneous/endoscopic drainage where appropriate. Operative management consisted of 9 primary repairs, 4 pyloric exclusions, 3 diverticularizations, 1 common bile duct (CBD) excision, and 1 exploration with irrigation and T-tube insertion.
Injuries were classified into two types: type I were duodenum lateral wall or jejunum injuries and type II were para-Vaterian injuries which includes periampullary injury and bile duct injury.
After acquiring approval from our Institutional Review Board, data on demographic information, ERCP indication and purpose, perforation site, management method, related complication, mortality, hospital stay, and hospital cost of the patients were collected from the patient's electronic medical records. Treatment outcome was assessed by evaluating the hospitalized duration, hospital cost, and related morbidity and mortality rates.
Comparative analysis, according to injury type and management method, was done using chi-square or Fisher's exact tests for categorical variables and Mann-Whitney U tests for continuous variables. Mean values are reported as mean ± standard error of mean. All statistic values with P-value < 0.05 were considered statistically significant. IBM SPSS ver. 19 (IBM Co., Armonk, NY, USA) was used for statistical analysis.
Over the 11-year period, 8,381 ERCP procedures were undertaken and 53 (0.63%) ERCP-related perforations occurred. Among the 53 patients, 22 (41.5%) were male and 31 (58.5%) were female. Mean age was 66.7 ± 1.6 years (range, 21 to 91 years).
The most frequent diagnosis was biliary stones (n = 30), followed by periampullary cancer (n = 6) and Klatskin tumor (n = 4). There were 3 cases each of gallbladder cancer, advanced gastric cancer, and benign biliary stricture. Other diagnoses included one case each of intraductal papillary mucinous neoplasm, biliary cystadenocarcinoma, hepatic cyst, and duodenal carcinoid tumor.
Diagnostic ERCP was performed in 8 patients (15.1%), and therapeutic ERCP in 45 (84.9%). Diagnostic procedures were either biopsy or cholangiography, and therapeutic procedures included endoscopic sphincterotomy, endoscopic naso-biliary drainage, stent insertion, stone removal, and endoscopic mucosal resection.
Type I injuries occurred in 39.6% (21 patients) of the cases. Type I patients included 6 with jejunal insult in Billroth II anatomy. Type II injuries occurred in 60.4% (32 patients). Of the type II, 24 patients received periampullary injury, mostly related to endoscopic sphincterotomy. The remaining 8 type II patients had bile duct injuries: 6 with CBD injuries mostly as result of balloon dilatation or stone removal, 1 with guidewire-related left intrahepatic duct stump injury (that patient previously received hepatic surgery), and 1 with a guidewire-related injury to a choledochoduodenal fistula.
Most of the injuries (39 cases, 73.6%) were immediately detected during the ERCP procedure, but 14 cases (26.4%) had delayed diagnoses. The mean delay time until detection was 28.4 ± 5.7 hours (range, 1 to 55.2 hours). Of the delayed patients, 12 experienced severe postprocedural abdominal pain, with or without fever, which warranted radiologic examinations. Perforation was confirmed by computed tomography (CT) in 11 patients and by plain abdominal radiography in 1 patient (Fig. 1). The remaining 2 cases were incidentally detected during follow-up CT and plain abdominal radiography, each.
The mean hospital stay was 23.7 ± 2.7 days (range, 0 to 86 days) and the mean hospital cost was 13.7 ± 2.1 thousand United States Dollars (USD) (range, 2.3 to 80.4 thousand USD). The morbidity and mortality rates were 34.0% (18/53) and 5.7% (3/53), respectively.
The demographics and procedure/injury related data for the 21 type I and 32 type II patients did not show significant differences; however, management method was significantly different. Type I injuries were mainly managed operatively (17/21, 81.0%) because a type I injury without possible adhesion or intervention was the operative indication at Seoul National University Hospital. Nearly all type II injuries were managed conservatively (31/32, 96.9%). The operative indication for the surgically managed type II patient was a large retained, impacted CBD stone with stricture distally. The stone could not be removed due to the stricture, even after balloon dilatation. Free air was detected after the procedure, and the patient was referred for surgery.
Comparative analyses of management outcomes demonstrated superior results in type II patients over type I (Table 1). Hospital stay was significantly shorter (19.3 ± 2.8 days vs. 30.6 ± 5.0 days, P = 0.010) and hospital cost was significantly less (9.5 ± 1.1 thousand USD vs. 20.1 ± 4.6 thousand USD, P = 0.028) for type II patients compared to type I patients. The morbidity rate was also significantly lower in type II patients (18.8% vs. 57.1%, P = .004). There was no difference in mortality.
Within the type II group, analysis comparing 24 periampullary injuries and 8 bile duct injuries was done. Demographic and procedure/injury related data were similar in both groups. Treatment outcomes were better in bile duct injury patients with shorter hospital stay (11.1 ± 2.4 days vs. 22.0 ± 3.4 days, P = 0.150), less cost (7.0 ± 2.4 thousand USD vs. 10.4 ± 3.4 thousand USD, P = 0.372), lower morbidity (12.5% vs. 20.8%), and null mortality (0.0% vs. 4.2%). However, none of these differences were significant.
Thirty-five patients received conservative management and 18 patients received operative management. No significant differences were found demographically or with respect to procedure and to detection delay between the management groups. However, between the groups, injury type and mean delayed detection time were significantly different (Table 1). In the conservative group, 88.6% (31/35) were type II injuries whereas in the operative group 94.4% (17/18) were type I (P < 0.001). Moreover, the mean delayed detection time was longer in the conservative group (36.0 ± 6.8 hours vs. 14.8 ± 7.7 hours, P = 0.031).
With regard to management outcomes, the mean hospital stay was shorter (20.6 ± 2.6 vs. days 29.8 ± 5.8 days, P = 0.092) and the mean hospital cost was lower (10.6 ± 1.3 thousand USD vs. 19.9 ± 5.3 thousand USD, P = 0.095) in the conservative group than in the operative group (Table 1). The conservative group suffered significantly less morbidity (22.9% vs. 55.6%, P = 0.017). The mortality rates were similar: 5.7% (1/18) and 5.6% (2/35) in the conservative and operative groups, respectively. Marginal significance was observed in hospital stay and hospital cost.
According to the surgical indication approach of our institution, type I injuries need surgery. However, 4 of 21 type I patients were not managed in accord with that guideline. Of those, there was 1 mortality case and 1 failed and 2 successful conservative management cases (Table 2). One of the successful cases involved endoscopic clipping (Fig. 2). The reason for the conservative management attempts in mainly Billroth II anatomy patients was the possibility of perforation sites localized with adhesions from previous surgery. There were not any specific indications in predicting the possibility of spontaneous sealing, and this prediction was based on the clinician's decision.
The outcomes of conservatively managed type I injuries were similar with those of the operatively managed type I injuries in terms of hospital stay (28.5 ± 6.9 days vs. 31.1 ± 6.0 days, P = 0.658), cost (18.1 ± 6.6 thousand USD vs. 20.6 ± 5.5 thousand USD, P = 0.929), morbidity (50.0% vs. 58.8%, P = 1.000), and mortality (25.0% vs. 5.9%, P = 0.352).
Additionally, although statistical significance was not demonstrated, conservatively managed type I injuries had longer hospital stay (28.5 ± 6.9 days vs. 19.6 ± 2.8 days, P = 0.153), higher cost (18.1 ± 6.6 thousand USD vs. 9.6 ± 1.2 thousand USD, P = 0.265), higher morbidity rate (50.0% vs. 19.4%, P = 0.218), and higher mortality rate (25.0% vs. 3.2%, P = 0.218) than type II injuries.
Of 53 patients, 18 (34.0%) experienced complication(s) during management. There were 31 complications: 17 in the surgical group and 14 in the conservative group. In the surgical group, surgery-related complications such as wound complications (n = 5) and repair site leakage (n = 3) were common. In conservative group, intra-abdominal fluid collection requiring percutaneous drainage (n = 5) and sepsis (n = 3) were most frequent.
There were 3 mortalities. One was a 75-year-old male who underwent ERCP for evaluation and stent insertion of CBD stricture. The patient had underlying Child-Pugh class C liver cirrhosis and Billroth II anatomy. Microperforation distal to the ampulla of Vater (type I injury) was detected during ERCP. The patient's condition aggravated, even after percutaneous drainage. Operation was not possible due to severe liver cirrhosis. Sepsis occurred and he expired after 17 days.
A 65-year-old female with extrahepatic duct obstruction, due to gallbladder cancer with liver metastasis, underwent ERCP for stent replacement. Perforation of the duodenum first portion was immediately detected, and primary repair with palliative cholecystectomy was done. The patient recovered relatively well, but expired from the terminal state of gallbladder cancer 66 days postoperatively.
The third mortality was an 85 year-old male with Klatskin tumor. ERCP was done for stent insertion and a type II injury was discovered 2 days later. The patient was recovering well with conservative management, but expired of cardiovascular accident 23 days later.
There have been continuous discussions on perforation management, and ERCP-related perforation was traditionally known to require prompt surgical management [8,9,12,19]. However, successful conservative managements have been reported, and currently is being widely accepted in selected patients [10,11,13-18]. A key discussion issue is who can be conservatively managed and who should be promptly operated upon. This is important since many have reported high morbidity and mortality rates in failed conservative management [8,10,14]. As the best outcome in a perforated patient can only be ensured by prompt and appropriate management, an accurate and simple guideline is needed.
Many studies report that around 70% of patients with ERCP-related perforation can be managed conservatively [16,17,20]. This percentage may vary depending on management policy. Following the treatment guideline at our institution, 66.0% of perforated patients were conservatively managed. Excluding mortalities, the conservative management failure rate was only 3.0% (1/33). To evaluate the validity of conservative management, conservative and operative groups were compared. Outcome comparison showed a significantly lower morbidity rate in the conservative group; also, with marginal significance, their hospital stay was shorter and cost was less (Table 1). These results suggest conservative management offers a better outcome than operative management. Therefore, any patient suitable for conservative management should be properly guided as to avoid unnecessary operation that may lead to an inferior outcome.
An important and significant difference between conservative and operative groups was in injury type. Most of the operative group had type I injuries, and nearly all of the type II injuries were managed conservatively. This implies that management method can simply be determined on the basis of injury type. Several researchers have classified perforations according to injury location or mechanism, and have proposed treatment recommendations for each class (Table 3) [10,15,21]. There is general acceptance that duodenum lateral wall perforation requires immediate surgery and that the remaining cases can be managed conservatively, in most cases. Based on our results and on previous opinions, ERCP-related perforations in the current study were classified into two types (rather than 3 or 4 types) to simplify the treatment algorithm.
Our type I was defined as duodenum lateral wall or jejunum injuries. The main reason for including jejunum injury is the high incidence of gastric cancer in Korea. Thus, encountering Billroth II anastomosis (gastrojejunostomy) during ERCP is not rare, especially in large tertiary referral center. In addition to their relatively frequent incidence, complexity due to anatomic alteration increases perforation risk. Eight of 53 cases (15.1%) in this series were patients with Billroth II anastomosis.
Type II represents para-Vaterian injuries defined as periampullary or bile duct injuries. Type II includes sphincterotomy-related and guidewire-related perforations because para-Vaterian injuries are mostly associated with endoscopic sphincterotomy or interventions and guidewire manipulations. We saw little use in classifying periampullary, bile duct, and guidewire-related perforations separately; moreover, nearly all guidewire perforations are periampullary or bile duct injuries. Furthermore, management outcome and treatment strategy do not differ for periampullary and bile duct injuries. These injuries can be managed conservatively and may be further improved by employing immediate endoscopic interventions to divert bile and pancreatic juice from the injury site [16,21,22]. Therefore, we integrated them into a single type for the sake of simplicity and to allow for quick countermeasures. The fact that the outcomes of conservatively managed bile duct injury were equivalent or superior to that of periampullary injury further supports the validity of merging bile duct and periampullary injuries. Although type II injuries can be successfully managed conservatively, an operation should be executed without hesitation in cases with evidence of severe sepsis/peritonitis or unsolved problems requiring correction such as retained biliary stone or hardware. Problems requiring surgical corrections other than the ones mentioned above are better dealt with elective surgery after recovery.
The management outcomes of type I and type II injury differ significantly in terms of hospital stay, cost, and morbidity rate. Table 1 clearly demonstrates superior outcomes for type II over type I injuries. Whether applying conservative management to type I injury would improve type I injury outcome can be questioned. The outcomes of conservative management of type I were not very different from those of operative management in type I injuries. Therefore, conservative management does not seem to guarantee improved outcome in type I injuries.
However, conservative management of type I injury after endoclipping seems promising. With the development of endoscopic techniques and equipment, there are more reports on nonsurgical treatments for small perforations in the upper gastrointestinal tract [23-25]. If endoclipping of small type I perforations at the time of injury is successful, conservative management may be attempted. One type I patient in our series was successfully managed in such a manner, and was discharged 19 days after the incident. Actual full recovery was achieved in 7 days but there was a 12 day delay due to financial disputes. Therefore, in cases where endoscopic clipping is possible, better outcomes can be anticipated, even in type I injuries. This warrants further investigations into the application of endoclipping and the feasibility of conservative management in type I injuries.
Based on our findings, we propose a simple management algorithm which can be readily and easily used (Fig. 3). If type I injury is detected, a prompt operation is recommended. Even in type I injury, conservative management can be attempted if endoclipping is possible at injury occurrence. In type II injury, conservative management may be initiated unless there are unsolved problems requiring surgical correction or any signs of severe sepsis/peritonitis, in which case surgery would be recommended. Defining severe sepsis/peritonitis objectively remains a task to be solved.
An obvious limitation of this field of study is that an RCT is not possible due to major ethical issues; thus, such study inevitably leads to retrospective case reviews. Another limitation is the small number of ERCP-related perforation cases. To our best knowledge, our number of analyzed cases (53 cases) from a single center is second only to a study by Fatima et al. [17] (75 cases). Even so, our sample size is insufficient for subgroup analyses. Rare as such cases are, acquiring enough cases from a single center is inefficient. For a quality conclusion, accumulation of data from multiple centers with same management guidelines or a comprehensive meta-analysis is required.
In summary, conservative management is feasible and produces better outcome than operative management in well-selected patients. Nearly all type II injuries and some type I injuries where endoclipping is possible may be successfully managed conservatively. Therefore, for convenience, injury may be classified simply into type I and type II injuries, and the appropriate management method determined accordingly. By following a simple and easy-to-remember management algorithm, satisfactory treatment outcomes can be expected.
Figures and Tables
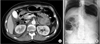 | Fig. 1Radiologic findings of endoscopic retrograde cholangiopancreatography perforations are demonstrated. (A) Computed tomography shows pneumoperitoneum, pneumoretroperitoneum, and fluid collection adjacent to duodenum. (B) Massive bilateral subdiaphragmatic pneumoperitoneum is detected on simple radiography. |
 | Fig. 2Perforation site endoclipping is presented. The patient was conservatively managed and discharged uneventfully. (A) The perforation site at posterior wall of duodenal bulb is identified. (B) Perforation site is successfully sealed with endoclips. |
 | Fig. 3Simple, easy-to-remember management algorithm is proposed based on the findings of current study. |
References
1. McCune WS, Shorb PE, Moscovitz H. Endoscopic cannulation of the ampulla of vater: a preliminary report. Ann Surg. 1968. 167:752–756.
2. Cotton PB, Lehman G, Vennes J, Geenen JE, Russell RC, Meyers WC, et al. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991. 37:383–393.
3. Freeman ML, Nelson DB, Sherman S, Haber GB, Herman ME, Dorsher PJ, et al. Complications of endoscopic biliary sphincterotomy. N Engl J Med. 1996. 335:909–918.
4. Loperfido S, Angelini G, Benedetti G, Chilovi F, Costan F, De Berardinis F, et al. Major early complications from diagnostic and therapeutic ERCP: a prospective multicenter study. Gastrointest Endosc. 1998. 48:1–10.
5. Wu HM, Dixon E, May GR, Sutherland FR. Management of perforation after endoscopic retrograde cholangiopancreatography (ERCP): a population-based review. HPB (Oxford). 2006. 8:393–399.
6. Masci E, Toti G, Mariani A, Curioni S, Lomazzi A, Dinelli M, et al. Complications of diagnostic and therapeutic ERCP: a prospective multicenter study. Am J Gastroenterol. 2001. 96:417–423.
7. Christensen M, Matzen P, Schulze S, Rosenberg J. Complications of ERCP: a prospective study. Gastrointest Endosc. 2004. 60:721–731.
8. Sarr MG, Fishman EK, Milligan FD, Siegelman SS, Cameron JL. Pancreatitis or duodenal perforation after peri-Vaterian therapeutic endoscopic procedures: diagnosis, differentiation, and management. Surgery. 1986. 100:461–466.
9. Bell RC, Van Stiegmann G, Goff J, Reveille M, Norton L, Pearlman NW. Decision for surgical management of perforation following endoscopic sphincterotomy. Am Surg. 1991. 57:237–240.
10. Stapfer M, Selby RR, Stain SC, Katkhouda N, Parekh D, Jabbour N, et al. Management of duodenal perforation after endoscopic retrograde cholangiopancreatography and sphincterotomy. Ann Surg. 2000. 232:191–198.
11. Avgerinos DV, Llaguna OH, Lo AY, Voli J, Leitman IM. Management of endoscopic retrograde cholangiopancreatography: related duodenal perforations. Surg Endosc. 2009. 23:833–838.
12. Booth FV, Doerr RJ, Khalafi RS, Luchette FA, Flint LM Jr. Surgical management of complications of endoscopic sphincterotomy with precut papillotomy. Am J Surg. 1990. 159:132–135.
13. Martin DF, Tweedle DE. Retroperitoneal perforation during ERCP and endoscopic sphincterotomy: causes, clinical features and management. Endoscopy. 1990. 22:174–175.
14. Scarlett PY, Falk GL. The management of perforation of the duodenum following endoscopic sphincterotomy: a proposal for selective therapy. Aust N Z J Surg. 1994. 64:843–846.
15. Enns R, Eloubeidi MA, Mergener K, Jowell PS, Branch MS, Pappas TM, et al. ERCP-related perforations: risk factors and management. Endoscopy. 2002. 34:293–298.
16. Assalia A, Suissa A, Ilivitzki A, Mahajna A, Yassin K, Hashmonai M, et al. Validity of clinical criteria in the management of endoscopic retrograde cholangiopancreatography related duodenal perforations. Arch Surg. 2007. 142:1059–1064.
17. Fatima J, Baron TH, Topazian MD, Houghton SG, Iqbal CW, Ott BJ, et al. Pancreaticobiliary and duodenal perforations after periampullary endoscopic procedures: diagnosis and management. Arch Surg. 2007. 142:448–454.
18. Kim BS, Kim IG, Ryu BY, Kim JH, Yoo KS, Baik GH, et al. Management of endoscopic retrograde cholangiopancreatography-related perforations. J Korean Surg Soc. 2011. 81:195–204.
19. Chaudhary A, Aranya RC. Surgery in perforation after endoscopic sphincterotomy: sooner, later or not at all? Ann R Coll Surg Engl. 1996. 78(3 Pt 1):206–208.
20. Knudson K, Raeburn CD, McIntyre RC Jr, Shah RJ, Chen YK, Brown WR, et al. Management of duodenal and pancreaticobiliary perforations associated with periampullary endoscopic procedures. Am J Surg. 2008. 196:975–981.
21. Howard TJ, Tan T, Lehman GA, Sherman S, Madura JA, Fogel E, et al. Classification and management of perforations complicating endoscopic sphincterotomy. Surgery. 1999. 126:658–663.
22. Dunham F, Bourgeois N, Gelin M, Jeanmart J, Toussaint J, Cremer M. Retroperitoneal perforations following endoscopic sphincterotomy; clinical course and management. Endoscopy. 1982. 14:92–96.
23. Kaneko T, Akamatsu T, Shimodaira K, Ueno T, Gotoh A, Mukawa K, et al. Nonsurgical treatment of duodenal perforation by endoscopic repair using a clipping device. Gastrointest Endosc. 1999. 50:410–413.
24. Jeong G, Lee JH, Yu MK, Moon W, Rhee PL, Paik SW, et al. Non-surgical management of microperforation induced by EMR of the stomach. Dig Liver Dis. 2006. 38:605–608.
25. Charabaty-Pishvaian A, Al-Kawas F. Endoscopic treatment of duodenal perforation using a clipping device: case report and review of the literature. South Med J. 2004. 97:190–193.




 ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download