Abstract
Stent fracture is one of the major factors compromising implanted stent patency due to its consequences including in-stent restenosis, thrombosis, perforation, and migration. Stent fracture can occur from stress (extrinsic or intrinsic) and biomechanical forces at different implantation sites. We report on 2 cases of stent fractures and pertinent literature. One patient, a 75-year-old male, presented with recurrence of claudication 14 months after superficial femoral artery stenting; a femoral artery occlusion with stent fracture was found, and he underwent femoropopliteal bypass. The other patient, a 72-year-old male presented with recurrence of claudication; a stent fracture was found without femoral artery occlusion, and he was treated with additional femoral artery stenting to secure the fracture site.
Angioplasty and stent implantation are often used in the treatment of peripheral arterial occlusive disease (PAOD). Risk factors that limit stent patency have been extensively evaluated. Nitinol alloys, the most commonly used as a self-expanding stent material, provide increased flexibility and radial force that allow the stent to adapt to the vessel shape. However, specific stresses and physiological environments can lead to stent fracture [1]. Stent fracture is a risk factor for stent occlusion though it is usually asymptomatic. The authors experienced 2 cases of stent fracture among 40 cases of superficial femoral artery (SFA) stenting for 14 months. Here, we report on 2 cases of stent fractures and include a pertinent literature review.
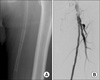
A 75-year-old man presented with recurrence of short distance claudication in the left leg. The patient had hypertension and a previous history of femoropopliteal bypass due to PAOD on his right SFA. Fourteen months ago, the patient underwent primary stenting of the left SFA to treat total occlusion with two overlapping self-expanding stents (Smart, Cordis, Miami, FL, USA). The stent deployed in the distal SFA was 7 mm in diameter and 15 cm in length, and the stent deployed in the proximal SFA was 7 mm in diameter and 12 cm in length with an overlap of 2 to 3 cm. Roentgenogram of stents showed complete transverse linear fracture with partial displacement in Hunter's canal distal to the stent overlap area (Fig. 1). Subsequent angiography revealed recurrent occlusion of the stented site (Fig. 2). Femoropopliteal artery bypass with reversed great saphenous vein was done resulting in the resolution of the claudication (Fig. 3).
A 72-year-old man with hypertension and ischemic coronary artery disease presented with recurrence of 500 m claudication in both legs. Four months ago, the patient underwent primary stenting for chronic total occlusion of SFA due to symptoms of the 500 m claudication. Two self-expanding nitinol stents (Smart, Cordis) were implanted. The distal stent was 7 mm in diameter and 15 cm in length, and the proximal stent was 7 mm in diameter and 12 cm in length with 2 cm of overlap in mid SFA. Roentgenogram revealed 3 strut fractures without displacement in the mid-SFA portion (Fig. 4), and subsequent angiography revealed multiple in-stent restenosis as well as stent fracture sites (Fig. 5). The narrowed portion of the stented site was dilated with a 6 mm balloon and a 7 × 60 mm stent was inserted at the site of stent fractures (Fig. 6). Angiographic results were satisfactory with symptom resolution.
Revascularization with nitinol stent implantation has better long-term results than angioplasty alone [2]; however, the cumulative incidence of femoropopliteal stent fracture varies from 2 to 65% in several studies looking specifically for stent fractures [3]. Stent fractures can be classified into five types. Type I fracture involves only a single strut; type II involves multiple struts that can occur at different sites; type III involves multiple strut fractures resulting in a complete transverse fracture without displacement; type IV results in a complete transverse linear fracture with stent displacement; and type V is spiral fracture. Mild stent fractures rarely lead to complications, however, multiple, migrated severe stent fractures are associated with restenosis or re-occlusion at the stented site.
Stent fractures occur as a result of a combination of several factors; physical and anatomical environment, procedural choice, and structural characteristics of the stent itself [1]. SFA is the most common site of infrainguinal PAOD, but revascularization using an endovascular stent in the SFA is subject to some vulnerable points in this physical and anatomical environment. The superficial anatomic course of the SFA is subject to external compression or torsion. The mechanical force exerted by the surrounding thigh muscle may cause stent compression or fracture. Furthermore, atherosclerosis usually involves long segments of the SFA. Scheinert et al. [4] reported that stent fracture incidence increases with stent length, with the fracture rate being significantly lower in segments less than 8 cm. Procedural choice such as use of overlapping stents has a role in stent fracture. Stent overlapping also makes the stent susceptible to fracture. The overlapped segment may act as fulcrum for stent fracture by focusing the stress on a specific stent site [5]. Structural characteristics of the stent also contribute to stent fracture when implanted in a specific setting. Nitinol stents, the most commonly used self-expanding stents, have great biocompatibility, elasticity and shape-memory properties; however their super-elasticity limits the stiffness of the stented vessel creating a hinge point predisposing to stent fracture [6].
Restenosis, occlusion and pseudoaneurysm are the complications associated with stent fracture in SFA. These complications may lead to recurrent symptoms, and revascularization may be required. Revascularization may be achieved by re-intervention or bypass surgery. Angioplasty with or without re-stent implantation constitutes the majority of interventions. However, at times, re-canalization of the occluded stent is impossible. In this case, organization and fibrotic thrombotic in-stent material is the main cause, and many attempts for treatment have been reported by several authors. Duterloo et al. [7] reported subintimal double-barrel restenting of an occluded primary stented SFA, they passed a guide wire through the subintima of the occluded stent, and created a neo-lumen side-by-side with the occluded primary stent leading to native lumen. Two self-expandable stents were positioned in a double-barrel fashion to prevent elastic recoil. Otherwise, Palena et al. [8] reported a direct stent puncture technique, which consisted in puncturing directly at the occluded point and introduction of a guide wire with a J-shaped tip. Another proximal site was punctured and the guide wire was snared through the occluded point recanalizing the occluded lumen with a satisfactory angiographic result.
Early detection of stent fracture and close follow-up might allow endovascular revascularization of stent obstruction. Although there is no universal consensus, Jaff et al. [9] suggests a standardized stent surveillance program in which high resolution digital X-ray images are obtained, and follow-up images at 12, 36, 60 months after stent deployment are compared to the baseline image obtained following stenting. At each time point, it is recommended to obtain at least 2 views of the stent with different anatomic positions of the limb such as extended and flexed knee.
In conclusion, femoral artery stenting is a common treatment for PAOD. However, stent fracture is one of the factors limiting long-term patency. We experienced two cases of stent fractures and recognized that a stent surveillance program is important for early detection and treatment before stent occlusion.
Figures and Tables
 | Fig. 2The angiography revealed stent occlusion in long segment of stented superficial femoral artery. |
References
1. Adlakha S, Sheikh M, Wu J, Burket MW, Pandya U, Colyer W, et al. Stent fracture in the coronary and peripheral arteries. J Interv Cardiol. 2010. 23:411–419.
2. Schillinger M, Sabeti S, Loewe C, Dick P, Amighi J, Mlekusch W, et al. Balloon angioplasty versus implantation of nitinol stents in the superficial femoral artery. N Engl J Med. 2006. 354:1879–1888.
3. Iida O, Nanto S, Uematsu M, Morozumi T, Kotani J, Awata M, et al. Effect of exercise on frequency of stent fracture in the superficial femoral artery. Am J Cardiol. 2006. 98:272–274.
4. Scheinert D, Scheinert S, Sax J, Piorkowski C, Braunlich S, Ulrich M, et al. Prevalence and clinical impact of stent fractures after femoropopliteal stenting. J Am Coll Cardiol. 2005. 45:312–315.
5. Bates MC, Campbell JR, Campbell JE. Late complication of stent fragmentation related to the "lever-arm effect". J Endovasc Ther. 2008. 15:224–230.
6. McKelvey AL, Ritchie RO. Fatigue-crack propagation in Nitinol, a shape-memory and superelastic endovascular stent material. J Biomed Mater Res. 1999. 47:301–308.
7. Duterloo D, Lohle PN, Lampmann LE. Subintimal double-barrel restenting of an occluded primary stented superficial femoral artery. Cardiovasc Intervent Radiol. 2007. 30:474–476.
8. Palena LM, Cester G, Manzi M. Endovascular treatment of in-stent occlusion: new technique for recanalization of long superficial femoral artery occlusion (direct stent puncture technique). Cardiovasc Intervent Radiol. 2012. 35:418–421.
9. Jaff M, Dake M, Pompa J, Ansel G, Yoder T. Standardized evaluation and reporting of stent fractures in clinical trials of noncoronary devices. Catheter Cardiovasc Interv. 2007. 70:460–462.




 ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download