Abstract
Purpose
In secondary hyperparathyroidism (sHPT), it is unclear which criterion for intraoperative parathyroid hormone (ioPTH) decline performs best and whether ioPTH monitoring is sufficiently efficacious in predicting postoperative surgical cure by retrospective review.
Methods
In 80 parathyroidectomies for sHPT, patients with ioPTH monitoring and follow-up PTH assay were categorized into physiologically accepted and failed groups. Receiver operating characteristic (ROC) curves were used to identify the criterion with the best performance and to determine the regression equation for prediction of surgical success.
Results
There was a statistically significant difference in the percentage reduction of ioPTHs between the two groups (P < 0.05). With our criterion, cure was predicted with a sensitivity of 86% and specificity that could be improved to 60% using an 85% ioPTH decrease as cut-off level when this value was compared to the Miami Criterion. There was a slightly negative correlation between the natural logarithm of percentage reduction of ioPTH and percentage reduction of PTH at follow-up (R2 = 0.109, P = 0.003).
Conclusion
ioPTH measurements are a useful tool for improvement of the cure rate of operations for sHPT. Because this study aimed at 40 minutes (ioPTH3) as an optimal process in the operation, we recommend using a criterion of more than 85% ioPTH decline at 40 minutes by use of the ROC curve, and the use of the presently calculated regression equation may enable prediction of success.
Secondary hyperparathyroidism (sHPT) is a common complication of chronic kidney disease (CKD), and is characterized by persistently elevated levels of parathyroid hormone (PTH) and parathyroid hyperplasia. It develops early in the course of CKD as an adaptive response to altered mineral homeostasis due to decreased kidney functions such as hyperphosphatemia, hypocalcemia, and 1,25(OH)2D deficiency [1]. Early stages of sHPT can be treated medically with the use of calcium supplementation, vitamin D analogues, phosphate binders, a low phosphate diet, and calcimimetic agents, whereas more advanced stages often require surgery. Indications for parathyroidectomy are medical treatment failure of severe sHPT resulting in excessive PTH and uncontrollable calcium/phosphate products, clinical signs such as pruritus and bone pain, biopsy-proven hyperparathyroid bone disease, pathological fractures, and calciphylaxis [2]. Surgical treatment is recommended in 0.5 to 2.6% of patients with sHPT [3,4]. The practice of parathyroidectomy in sHPT is well-established, and subtotal parathyroidectomy with the goal of retaining some parathyroid function has been preferentially performed [4]. Critics of subtotal parathyroidectomy quote high recurrence rates that approach 30% [5]. More recently, total parathyroidectomy has attracted increased interest [3], although no consensus view has emerged as to which approach is best. Intraoperative parathyroid hormone (ioPTH) measurement is a functional diagnostic tool during parathyroid surgery that permits prediction of postoperative outcome and helps the surgeon to decide whether further exploration is necessary [6]. A reduction in ioPTH levels of ≥50% indicates surgical success with a sensitivity of 98% and specificity of 91% in primary hyperparathyroidism, and has been suggested as appropriate for ioPTH monitoring in surgical treatment of sHPT [4,6-10]. Nonetheless, there is no standard definition of success in sHPT. The aim of our study was to establish which criterion of ioPTH decline performs best and to assess the efficacy of ioPTH monitoring in predicting postoperative outcome in patients with sHPT.
For this study, we analyzed the outcomes of 102 operations for sHPT guided by ioPTH assays performed at Korea University Guro Hospital between January 2003 and October 2010. All patients with sHPT had chronic renal failure as the underlying disease leading to HPT and received hemodialysis. Twenty-two patients were lost to follow-up. Thus, 80 patients were enrolled. Informed consent was obtained from all patients. We performed radiologic imaging studies such as sestamibi scans, ultrasonography, and computed tomography for most patients preoperatively. For patients undergoing surgery for the first time, surgery was performed by exploration of the neck, initially focusing at the usual anatomic sites that harbor the upper and lower parathyroid glands bilaterally. If supernumerary glands were discovered during this dissection, these were also excised. All excised specimens from suspected supernumerary glands were identified as parathyroid glands by frozen section biopsy. However, if fewer than four parathyroid glands were located during this process, the search for the remaining parathyroid glands proceeded by systematic sequential ipsilateral dissection of the thymus, level VI clearance, and sequential opening of the retropharyngeal space, retroesophageal space, and carotid sheath. Patients scheduled for revision surgery underwent preoperative investigations in an attempt to identify the location of residual parathyroid tissue. If the intraoperative approach was negative for parathyroid tissue, a systematic bilateral search for the remaining parathyroid glands was performed as described above. All procedures were performed by the same surgeon. In cases where enlargement of three or four glands was noted, a subtotal or total parathyroidectomy with autotransplantation was carried out. We performed subtotal parathyroidectomy for patients who were scheduled or willing to undergo kidney transplantation. For subtotal parathyroidectomy, three glands were removed completely, and approximately 50% of the smallest and most normal-appearing gland (fourth gland) was left in the neck. For total parathyroidectomy, all glands were removed during the autotransplantation and 10 to 15 1 mm pieces of the smallest gland were simultaneously autotransplanted in the forearm. Baseline levels of ioPTH (ioPTH1) were determined prior to incision. After exploration and resection of all enlarged parathyroid glands, ioPTH levels were determined in the same fashion at 20 minutes (ioPTH2) and 40 minutes (ioPTH3) after excision. PTH levels were determined with an Elecsys 2010 apparatus (Roche Diagnostics Co., Indianapolis, IN, USA). Patient characteristics and factors possibly predicting a successful operation are shown in Table 1. The chi-square test and unpaired t-test were used to analyze nominal and continuous data, respectively. Empirical receiver operating characteristic (ROC) curves were used to compare criteria based on different percentages of ioPTH decline. Differences between ROC curves were tested with a bootstrap technique. A P-value < 0.05 was considered statistically significant. A scatterplot with data derived from all patients was constructed to predict the final PTH from the percentage reduction in ioPTH.
During the study period, 81 surgical total parathyroidectomies were performed on 80 patients diagnosed with sHPT. One patient underwent two procedures (one primary and one revision) for recurrent sHPT due to a supernumerary gland in the mediastinum. Twenty-four patients underwent subtotal parathyroidectomy and 56 underwent total parathyroidectomy and autotransplantation in the brachiocephalis muscle of the forearm. Four patients had supernumerary glands. Two patients were known to have supernumerary glands prior to the operation based on radiologic imaging studies, while the supernumerary glands of the other two patients were discovered during surgery.
The male-to-female ratio was 1.1:1. The average age at time of surgery was 45.9 years for males and 51.3 years for females. The average length of follow-up was 40.0 ± 25.1 months (median, 54 months; range, 12 to 95 months). The mean ± standard deviation (SD) ioPTH1 ioPTH2, and ioPTH3 values were 1,422.1 ± 828.9 pg/mL, 362.7 ± 218.5, and 214.5 ± 268.3 pg/mL, respectively. The 1-year levels of ioPTH 1, 2, 3, and PTH for all patients are shown in Fig. 1. All patients showed >50% reduction in ioPTH; the mean reduction in ioPTH2 and ioPTH3 was 74.7 ± 20.6% and 86.3 ± 11.9%, respectively. Histologic analysis of tissue from the 286 excised parathyroid glands revealed that nearly all (98.2%) were hyperplastic parathyroid glands, 1.0% were adenomas, and 0.8% were histologically normal parathyroid glands. At the end of the follow-up period, 57 of 80 patients (71.3%) had a physiologically acceptable cure with a PTH level ≤300 pg/mL in the first 12 postoperative months (group 1), and 23 of 80 patients (28.7%) were considered surgical failures with a PTH level >300 pg/mL (group 2). Fig. 2 shows the percentage reduction in ioPTH for each group for the two potential outcomes. The median percentage reduction was 89.4% (range, 53.9 to 98.0%) for group 1 patients, which was considered physiologically acceptable, and 84.7% (range, 64.0 to 96.0%) for group 2 patients, which was considered as a failure. The range and interquartile range are shown as a box and whisker plot for each group in Fig. 2. A significant difference in the percentage of ioPTH decline was evident between the successful and unsuccessful operations for both ioPTH2 and ioPTH3 (Table 1). Furthermore, serum phosphate concentrations differed significantly at one year between the two groups. We next assessed the percentage of PTH decline that was most accurate at predicting postoperative success. When different percentages of ioPTH decline were considered, the ROC curves for the percentage decline using ioPTH2 were slightly, but not significantly, less accurate than the ROC curves based on ioPTH3 values (Fig. 3; n = 80 without any missing values, difference in area under the curve 0.051 with a confidence interval of -0.074 to 0.177). Given these slightly better ratios for sensitivity and specificity based on ioPTH3 data and the goal of maintaining sensitivity (approximately 86%), the criterion of a 85% decline in ioPTH2 as the cut-off point resulted in the best ratio with a sensitivity of 86% and a specificity of 60% (Fig. 3). However, this did not differ significantly from the best ratio of ioPTH2 (75% decline), with a sensitivity of 83% and specificity of 48%.
Fig. 4 is a scatterplot with data derived from all patients. A comparison was made for the entire cohort between the percentage reduction in ioPTH versus the 1-year PTH at follow-up, expressed as the natural logarithm of the percentage of the ioPTH1 assay. The calculated regression line displayed a slight negative correlation (R2 = 0.109, P = 0.003). The equation for the regression line derived from these data was y = 6.755 + (-0.054)x.
At the 1-year follow-up, we found that 71.3% of the operations had yielded a physiologically acceptable cure, defined as a PTH level ≤300 pg/mL. This result seems rather good, even in light of literature reporting a 35% chance of persistent or recurrent disease for patients with sHPT [11-13]; however, our criterion for cure might be different. We categorized patients into two groups -a physiologically acceptable group and a surgically failed group-based on a PTH level of 300 pg/mL. The ideal blood concentration of PTH is not known for uremic subjects, but the levels advocated by different researchers vary from 75 to 175 pg/mL [10]. Our criterion was based on the Kidney Disease Outcomes Quality Initiative (K/DOQI) guidelines for the target range of intact plasma PTH according to the stage of CKD [14]. The target range of PTH according to the K/DOQI guidelines is 150 to 300 pg/mL in stage 5 of CKD (dialysis or glomerular filtration rate <15 mL/min/1.73 m2). Different ioPTH decline criteria have been suggested for prediction of postoperative outcomes in patients with sHPT [4,6,9]. When using the intact PTH assay, several authors have suggested using the same criterion as that used in patients with primary hyperparathyroidism (the Miami Criterion of >50% decline from baseline PTH 5 to 10 minutes after excision) [7,15], whereas other authors argued that higher percentages of decline or absolute values at other time points after excision are necessary [9]. Given that in the present series of patients the reduction in ioPTH was well over 50% in all patients, yet 28.7% of patients were subsequently categorized as surgical failures, the 50% rule for ioPTH reduction has no relevance in the surgical management of sHPT. We analyzed the ROC curves with the primary goal of maintaining a high sensitivity to prevent further unnecessary surgical explorations with the associated risks of preoperative complications and postoperative hypoparathyroidism. Ideally, the specificity should also be as high as possible to reduce the necessity of reoperations, which carry the same risks as extensive exploration in the primary operation. The sensitivity/specificity ratio for predicting a physiologically acceptable cure was clearly improved by using a higher percentage of ioPTH decline. Furthermore, extending the measurements to 40 minutes after resection of the parathyroid glands influenced the predictive performance of ioPTH measurements, which seems to justify a further 20-minute delay, even though circulating PTH, which has a half-life of 3 to 5 minutes in patients with normal renal function, is delayed in CKD. Similarly, in another study, temporal extension of measurements led to a clinically relevant improvement, although the sample size in this study was small [6]. A limitation of the present ROC analysis is the different numbers of successful and unsuccessful operations; calculations of sensitivity and specificity are not equally accurate. Furthermore, missing values reduced the number of patients analyzed to 80 patients. However, ioPTH2 decline was a worse predictor of postoperative normalization of PTH than ioPTH3 decline, possibly due to the differences in the time needed for removal of all glands. It is reasonable to question whether the measurement of ioPTH is useful and if there is one optimal criterion for all patients with sHPT. It is conceivable that patients who are dialysis-dependent would have a different optimal criterion than patients with renal transplants with a mild-to-moderate degree of renal failure. Fig. 2 shows that the ioPTH data for the two outcome groups differed significantly. These data and the scatterplot data (Fig. 4) collectively suggest that the greater the reduction in ioPTH, the greater the chance of a surgical cure. However, it remains unclear why some patients with similar levels of reduction of ioPTH and histologic evidence of a successfully performed parathyroidectomy ultimately fall into different outcome groups. Chronic stimulation of unexcised or microscopic rests or autotransplanted parathyroid tissue may cause these rests to function as autonomous glands or hyperplasia, making it difficult to achieve a physiologically acceptable condition in these patients. With regard to recurrence or surgical failure due to the presence of autotransplanted parathyroid tissue, it would be helpful to identify the nodularity of the excised portion of the remnant parathyroid tissue by histopathologic examination [16]. Future use of the equation y = 6.755 + (-0.054)x derived from the scatterplot (Fig. 4) may make it possible to predict the follow-up PTH level (y) for any given percentage reduction in ioPTH (x). This method may predict a successful operation.
In conclusion, ioPTH measurement can be a useful tool for improving the cure rate of operations for sHPT. Because we chose 40 minutes (ioPTH3) as the optimal time for measuring PTH3 during the operation, we recommend using a criterion of >85% ioPTH decline at 40 minutes by ROC analysis. Patients with additional tissue removed would have an insufficient decline in PTH levels based on this criterion. Prospective analyses, including a cost-effectiveness study, are needed to validate this criterion.
Figures and Tables
 | Fig. 1Box and whiskers plot of parathyroid hormone (PTH) assays for all patients who underwent a parathyroidectomy during the study period. Intraoperative PTH (ioPTH), ioPTH2, and ioPTH3 were performed perioperatively; PTH assays were performed at the 1-year follow-up. ioPTH1, baseline levels of ioPTH; ioPTH2, ioPTH levels at 20 minutes after excision; ioPTH3, ioPTH levels at 40 minutes after excision. |
 | Fig. 2Box and whiskers plot comparing the percentage intraoperative parathyroid hormone (ioPTH) reduction between the two groups. |
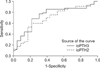 | Fig. 3Receiver operating characteristic curves from the percentage decline based on the ioPTH2 and ioPTH3 assay results. ioPTH2, ioPTH levels at 20 minutes after excision; ioPTH3, ioPTH levels at 40 minutes after excision. |
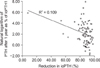 | Fig. 4Scatterplot showing the percentage reduction of intraoperative parathyroid hormone (ioPTH) vs. the natural logarithm of PTH after 1 year expressed as a percentage of ioPTH1. ioPTH1, baseline levels of ioPTH. |
Table 1
Patient characteristics and factors predicting successful operationa)

Values are presented as mean (range) or mean ± SD.
PTH, parathyroid hormone; Ca, calcium; P, phosphate; Total, total parathyroidectomy; subtotal, subtotal parathyroidectomy; ioPTH, intraoperative parathyroid hormone; SD, standard deviation.
a)Biochemical definition defined as a serum PTH concentration equal to or below 300 pg/mL for successful operation was used. b)Values are presented as mean. c)P < 0.05 for difference with successful operation.
References
1. Komaba H, Kakuta T, Fukagawa M. Diseases of the parathyroid gland in chronic kidney disease. Clin Exp Nephrol. 2011. 15:797–809.
2. Stracke S, Keller F, Steinbach G, Henne-Bruns D, Wuerl P. Long-term outcome after total parathyroidectomy for the management of secondary hyperparathyroidism. Nephron Clin Pract. 2009. 111:c102–c109.
3. Roshan A, Kamath B, Roberts S, Atkin SL, England RJ. Intra-operative parathyroid hormone monitoring in secondary hyperparathyroidism: is it useful? Clin Otolaryngol. 2006. 31:198–203.
4. Moor JW, Roberts S, Atkin SL, England RJ. Intraoperative parathyroid hormone monitoring to determine long-term success of total parathyroidectomy for secondary hyperparathyroidism. Head Neck. 2011. 33:293–296.
5. Maxwell PH, Winearls CG. Recurrence of autonomous hyperparathyroidism in dialysis patients. Nephrol Dial Transplant. 1997. 12:2195–2200.
6. Freriks K, Hermus AR, de Sevaux RG, Bonenkamp HJ, Biert J, den Heijer M, et al. Usefulness of intraoperative parathyroid hormone measurements in patients with renal hyperparathyroidism. Head Neck. 2010. 32:1328–1335.
7. Haustein SV, Mack E, Starling JR, Chen H. The role of intraoperative parathyroid hormone testing in patients with tertiary hyperparathyroidism after renal transplantation. Surgery. 2005. 138:1066–1071.
8. Richards ML, Grant CS. Current applications of the intraoperative parathyroid hormone assay in parathyroid surgery. Am Surg. 2007. 73:311–317.
9. Chou FF, Lee CH, Chen JB, Hsu KT, Sheen-Chen SM. Intraoperative parathyroid hormone measurement in patients with secondary hyperparathyroidism. Arch Surg. 2002. 137:341–344.
10. Echenique Elizondo M, Diaz-Aguirregoitia FJ, Amondarain JA, Vidaur F. Intraoperative monitoring of intact PTH in surgery for renal hyperparathyroidism as an indicator of complete parathyroid removal. World J Surg. 2005. 29:1504–1509.
11. Hargrove GM, Pasieka JL, Hanley DA, Murphy MB. Short- and long-term outcome of total parathyroidectomy with immediate autografting versus subtotal parathyroidectomy in patients with end-stage renal disease. Am J Nephrol. 1999. 19:559–564.
12. Gasparri G, Camandona M, Abbona GC, Papotti M, Jeantet A, Radice E, et al. Secondary and tertiary hyperparathyroidism: causes of recurrent disease after 446 parathyroidectomies. Ann Surg. 2001. 233:65–69.
13. Dotzenrath C, Cupisti K, Goretzki E, Mondry A, Vossough A, Grabensee B, et al. Operative treatment of renal autonomous hyperparathyroidism: cause of persistent or recurrent disease in 304 patients. Langenbecks Arch Surg. 2003. 387:348–354.
14. National Kidney Foundation. K/DOQI clinical practice guidelines for bone metabolism and disease in chronic kidney disease. Am J Kidney Dis. 2003. 42:4 Suppl 3. S1–S201.
15. Yamashita H, Cantor T, Uchino S, Watanabe S, Ogawa T, Moriyama T, et al. Sequential changes in plasma intact and whole parathyroid hormone levels during parathyroidectomy for secondary hyperparathyroidism. World J Surg. 2005. 29:169–173.
16. Tominaga Y, Tanaka Y, Sato K, Nagasaka T, Takagi H. Histopathology, pathophysiology, and indications for surgical treatment of renal hyperparathyroidism. Semin Surg Oncol. 1997. 13:78–86.




 ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download