Abstract
Purpose
The aim of this study was to evaluate screening methods in the lower extremities by measurement of the digital pulse oximetry (oxygen percent saturation [SpO2]) of toes for peripheral arterial disease (PAD).
Methods
A prospective study was performed among 49 patients (98 limbs) with lower extremity arterial occlusive disease. We attempted to measure the ankle-brachial index (ABI), digital pulse oximetry (SpO2), and computerized tomographic angiography (CTA). Patients were divided into three groups by the traditional Fontaine classification system by symptom and CTA criteria: 1) Critical limb ischemia (Fontaine III and IV), 2) Claudication; (Fontaine II), and 3) asymptomatic limbs (Fontaine I).
Results
The sensitivity, specificity, positive and negative predictive values between active treatment groups (group I and II; endovascular and open surgery) and conservative group (group III) are all statistically significant. ABI; 55.09%, 94%, 96.7%, 39.02% (R = 12.54, P < 0.000) SpO2; 87.06%, 87.8%, 84.3%, 90% (R = 40.11, P < 0.000). Pre-SpO2 and pre-ABI all show statistically significant correlation in group I vs. group II, symptomatic PAD (group I and II) vs. asymptomatic PAD (group III), and the total PAD comparison. The Pearson's correlation coefficient between SpO2 and ABI all show significant correlation in group II. Pre-SpO2 vs. Pre-ABI show strong positive correlation except asymptomatic group (group III).
The ideal screening test for PAD would be inexpensive, non-invasive, accurate, and easily administered in the physician's office. In the U.S., the number of adults affected by peripheral arterial disease (PAD) is as large as 8 million [1], and in Korea, 4.4% (50/1,150) is reported [2] in elderly men (≥65), a number expected to rise as the elderly population grows. Individuals with PAD have a three- to four-fold increased risk of cardiovascular disease morbidity and mortality compared to individuals without PAD [1]. Early detection of PAD allows the implementation of an effective treatment, which has been shown to reduce the morbid-mortality of cardiovascular patients. Currently recommended are several non-invasive tests include pulse palpation, the ankle-brachial index (ABI), transcutaneous oxygen tension, color-doppler ultrasonography, computed tomographic angiography (CTA), Angiography, and magnetic resonance angiography. Pulse palpation is easy to perform but has interobserver variability. Dorsalis pedis is congenitally absent in 4 to 12% of the population [3]. ABI measurement is simple, inexpensive, painless, reproducible and can be easily performed in a physician's office. But, for early detection of PAD, the ABI may not be as sensitive as reported. Carter [4] reported that in patients with severe arterial stenosis on arteriography, the ABI was abnormal in 80%, but when only mild arterial stenosis was present, the ABI was low in only 50%. In prior work, we found that digital pulse oximetry (oxygen percent saturation [SpO2]) performed with a standardized protocol in a pulmonary function laboratory at the time of arterial blood analysis was a useful tool for detecting hypoxia. But previous investigations of pulse oximetry to diagnose lower extremity arterial disease have produced mixed results. Joyce et al. [5] reported that patients with PAD had significantly lower arterial oxygen saturation (SaO2]) in the ischemic limbs. The SaO2] improved after revascularization. Jawahar et al. [6] found that pulse oximetry had low sensitivity to detect PAD when compared with the ABI used as the reference test. The patients in these studies were suspected of having arterial disease on clinical grounds, so pulse oximetry was not used as a screening test. The present study was undertaken to prospectively evaluate digital pulse oximetry as a non-invasive screening test for PAD.
We performed a prospective study of 49 patients (98 limbs) with PAD referred for initial PAD evaluation to the hospital between August 2009 and October 2010. Demographic, clinical, and laboratory data were recorded. SpO2 measurements were performed by clinic staff during the initial clinic evaluation by using a handheld Radical-7 Signal Extraction Pulse oximeter (Masimo Co., Irvine, CA, USA) applied to the index finger and both great toes with the patient in the sitting or supine position at room air. If the SpO2 signal was not obtainable due to necrosis or loss, the next toe's signal was used. And the SpO2 signal was compared to finger signals that have diminished due to other disease or condition such as severe COPD, cardiac failure, or room temperature. The ABI measurements were performed after the digital pulse oximetry measurements using a Non-invasive Vascular Screening Device VP-1000 (Model BP 230 RPE II, OMRON Healthcare Co., Kyoto, Japan). Three-dimensional CT-angiography analyses were performed for evaluation of stenosis and obstruction of the peripheral arteries of the lower extremities. The diagnosis of PAD was based on clinical and CTA criteria. The criteria used for identifying significant arterial stenosis or obstruction lesions. Patients were divided into three groups by the traditional Fontaine classification system by symptoms and CTA criteria. : 1) Critical limb ischemia (CLI); ischemic rest pain and ischemic ulceration/necrosis (Fontaine III and IV) with significant arterial disease; 2) Claudication; (Fontaine II) with significant arterial disease, and 3) asymptomatic limbs (Fontaine I).
Analysis was performed using SPSS ver. 18 (IBM, New York, NY, USA). Group variables were compared using one-way analysis of variance with post hoc multiple comparisons assuming homogenous variance. Significance was set at P = 0.05. Comparisons between SpO2 and ABI employed Pearson correlation coefficients with two-tailed significance set at P = 0.05.
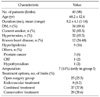
A total of 98 limbs were studied on 49 patients with PAD. The clinical characteristics of the patients participating in the study are summarized in Table 1. The majority of patients were male (41/49) and the mean age was 68.2 ± 12.4 years.
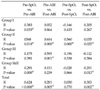
The screening tests were performed by digital pulse oximetry and ABI, and then the diagnosis and treatment planning with CTA. Active treatment for symptomatic limbs was performed in group I and II as open surgery and/or endovascular intervention. Conservative treatment for asymptomatic limbs was performed in group III as medication or observation. Most common lesion was identified in femoropopliteal arteries. The pre-treatment ABI (pre-ABI), post-treatment ABI (post-ABI), pre-treatment SpO2 (pre-SpO2), and post-treatment SpO2 (post-SpO2) are listed in Table 2. PAD diagnostic criteria of ABI were less than 0.9 and SpO2 less than 95% was considered abnormal. The sensitivity, specificity, positive and negative predictive values of ABI were 100%, 60.46%, 76.38%, 100% and Pearson chi-square is statistically significant (R = 11.77, P = 0.003). SpO2 were 44.4%, 96.1%, 96.9%, 38.4% and Pearson chi-square is not statistically significant (R = 3.02, P = 0.082). However, the sensitivity, specificity, positive and negative values between active treatment groups (group I and II) and medication group are all statistically significant. ABI; 55.09%, 94%, 96.7%, 39.02% (R = 12.54, P < 0.000) SpO2; 87.06%, 87.8%, 84.3%, 90% (R = 40.11, P < 0.000).
Table 3 demonstrates the correlation of SpO2 and the ABI between group I vs. II, group I, II vs. III, and in total limbs; Correlations show statistical significance in pre-ABI and pre-SpO2.
Table 4 and Fig. 1 demonstrates the Pearson's correlation coefficient (R) between SpO2 and the ABI; pre-ABI vs. pre-SpO2, pre-ABI vs. post-ABI, pre-SpO2 vs. post-SpO2, post-ABI vs. post-SpO2. Group I shows statistically strong correlation in pre-SpO2 vs. pre-ABI, group II in all comparisons of parameters, group III in only pre-ABI vs. post-ABI, group I,II; symptomatic groups in pre-SpO2 vs. pre-ABI and post-SpO2 vs. post-ABI, total groups in pre-SpO2 vs. pre-ABI, pre-ABI vs. post-ABI, and post-SpO2 vs. post-SpO2.
The purpose of this study was to analyze the usefulness of SpO2 of screening tests for PAD. Circumstances of discovery include intermittent claudication or distal trophic lesions, but some subjects were asymptomatic, and the condition was detected during routine physical examination [7,8]. The non-invasive screening techniques are fast, easy to perform, inexpensive and can be used in a primary health care population. When screening a population of PAD, a high-sensitivity is important [9].
ABI is the most recommended non-invasive screening test for PAD. Recent publications reported that the interval between 0.9 and 1.10, currently taken as normal, may not be so [10]. Actually, an ABI ≤0.9 has been recommended by the American Heart Association [11]. Among well-trained technicians, its reliability has been excellent, and the validity of the test for stenosis of ≥50% in leg arteries is high (sensitivity of 90% and specificity of 98%) [12]. However, the sensitivity of the ABI test varied widely among previous published studies. ABI detection in diabetes and the elderly yielded lower sensitivity, 15 to 20% [13], 63% [14], 68% [15], 69.3% [16], and 70.6% [17], suggesting that the test may be affected by diabetes status and aging. And Feigelson et al. [18] found that when they excluded patients with symptoms and signs of PAD, ABI values of less than 0.9 had a sensitivity of only 28.4%; and suggested that the ABI seems less accurate as a screening test in patients without symptoms or sings of PAD.
Pulse oximetry measures peripheral blood hemoglobin SaO2]. Low blood flow in an extremity produces lower SaO2] in the blood, a fact that vascular surgeons use to assess patency of arterial reconstructions [19]. Joyce et al. [5] compared the ABI, pulse oximetry measurement of the toes, and transcutaneous oxygen tension measurement with the arteriographic appearance in patients suspected of having limb ischemia. They found that pulse oximetry correlated best with the arteriographic appearance. Jawahar et al. [6] studied patients between suspected PAD group and non-suspected PAD group. Pulse oximetry results were defined as abnormal if there was a decrease of more than 2% in saturation at the toe from the finger or a decrease of more than 2% on elevation of the foot by 12-in. When an ABI less than 0.9 was considered as PAD, pulse oximetry had a sensitivity of only 16% [14]. Pulse oximetry is a well-established method for non-invasive evaluation of arterial oxygenation. Numerous studies have found that pulse oximetry is accurate and reliable for screening for hepatopulmonary syndrome [20], congenital heart disease [21], diabetes [14,22,23], and sepsis [24].
In this study, we divided patients by symptomatic criteria, not treatment modality, because recent publications reported no difference between endovascular treatment and open surgery in multi-level studies [25,26].
We compared the ABI, digital pulse oximetry measurement of the toes, and CTA appearance in patients suspected of PAD. An ABI less than 0.9 was considered as PAD. The mean pre-ABI in total patients as compared to post-ABI were significantly lower (0.7 ± 0.3 vs. 1.02 ± 0.6; R = 0.09, P < 0.000) and show very high sensitivity and negative predictive values. In a survey of each group, post-ABI shows improvement compared to pre-ABI in group I and group II. I; Acute ischemic limbs 0.37 ± 0.3 vs. 0.95 ± 0.1, II; Chronic limbs 0.8 ± 0.2 vs. 1.05 ± 0.9, III; Medication limbs 1.05 ± 0.1 vs. 1.04 ± 0.1 (R = 0.547, P < 0.000). In addition, the sensitivity and negative predictive values between active treatment groups (group I and II) and conservative group show the significant reduction (55.09%, 39.02%, R = 12.54, P < 0.000).
Pulse oximetry results were defined as abnormal if there was a decrease of more than 5% in saturation at the toe. The sensitivity, specificity, positive and negative predictive values of SpO2 are 44.4%, 96.1%, 96.9%, 38.4% and Pearson chi-square is not statistically significant (R = 3.02, P = 0.082). However, the sensitivity, specificity, positive and negative values of SpO2 between active treatment groups (group I and II) and conservative group are all statistically significant (87.06%, 87.8%, 84.3%, 90%, R = 40.11, P < 0.000). Overall, total patients show low sensitivity and negative predictive value of SpO2, whereas active treatment groups for symptomatic limbs show even levels.
In our study, the ABI and digital pulse oximetry measurements of the toes before and after treatment (endovascular treatment, open surgery, and medication) were compared. Group I vs. II, group I, II vs. III, and total PAD limbs show a significant difference at pre-SpO2 and pre-ABI. The Pearson's correlation between SpO2 and ABI show strong correlation. In group I, acute ischemic limbs show in pre-SpO2 vs. pre-ABI. Group II, claudication limbs show the difference in all comparisons. Group I and II, symptomatic limbs show the correlation in pre-SpO2 vs. pre-ABI and post-SpO2 vs. post-ABI.
Our results suggest that pulse oximetry is at least as accurate as ABI and is an effective additional method for screening patients with PAD.
In conclusion, these results suggest pulse oximetry may be a useful tool to screen for PAD in symptomatic patients.
Figures and Tables
 | Fig. 1(A) Pre-SpO2 vs. pre-ABI; Pearson's correlation coefficient R = 0.624 (P < 0.000) show strong correlation. (B) Pre-ABI vs. post-ABI; Pearson's correlation coefficient R = 0.281 (P < 0.005) show positive correlation but statistically significant. (C) Post-ABI vs. post-SpO2; Pearson's correlation coefficient R = 0.030 (P = 0.770) show no correlation nor statistically significant. (D) Post-SpO2 vs. post-ABI; Pearson's correlation coefficient R = 0.303 (P = 0.02) show positive correlation but statistically significant. Pre-SpO2, pre-treatment oxygen percent saturation; Pre-ABI, pre-treatment ankle-brachial index; Post-ABI, post-treatment ankle-brachial index; Post-SpO2, post-treatment oxygen percent saturation. |
References
1. Langham MC, Floyd TF, Mohler ER 3rd, Magland JF, Wehrli FW. Evaluation of cuff-induced ischemia in the lower extremity by magnetic resonance oximetry. J Am Coll Cardiol. 2010. 55:598–606.
2. Kim JY, Jeon YS, Cho SG, Kong E, Jung JE, Park SG, et al. Prevalence and characteristics of major vascular diseases of elderly men in the Incheon area. J Korean Surg Soc. 2010. 78:305–313.
3. Barnhorst DA, Barner HB. Prevalence of congenitally absent pedal pulses. N Engl J Med. 1968. 278:264–265.
4. Carter SA. Clinical measurement of systolic pressures in limbs with arterial occlusive disease. JAMA. 1969. 207:1869–1874.
5. Joyce WP, Walsh K, Gough DB, Gorey TF, Fitzpatrick JM. Pulse oximetry: a new non-invasive assessment of peripheral arterial occlusive disease. Br J Surg. 1990. 77:1115–1117.
6. Jawahar D, Rachamalla HR, Rafalowski A, Ilkhani R, Bharathan T, Anandarao N. Pulse oximetry in the evaluation of peripheral vascular disease. Angiology. 1997. 48:721–724.
7. Criqui MH, Fronek A, Klauber MR, Barrett-Connor E, Gabriel S. The sensitivity, specificity, and predictive value of traditional clinical evaluation of peripheral arterial disease: results from noninvasive testing in a defined population. Circulation. 1985. 71:516–522.
8. Hiatt WR. Medical treatment of peripheral arterial disease and claudication. N Engl J Med. 2001. 344:1608–1621.
9. Johansson KE, Marklund BR, Fowelin JH. Evaluation of a new screening method for detecting peripheral arterial disease in a primary health care population of patients with diabetes mellitus. Diabet Med. 2002. 19:307–310.
10. Gornik HL. Rethinking the morbidity of peripheral arterial disease and the "normal" ankle-brachial index. J Am Coll Cardiol. 2009. 53:1063–1064.
11. Hirsch AT, Haskal ZJ, Hertzer NR, Bakal CW, Creager MA, Halperin JL, et al. ACC/AHA 2005 Practice Guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease): endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; TransAtlantic Inter-Society Consensus; and Vascular Disease Foundation. Circulation. 2006. 113:e463–e654.
12. Ouriel K, McDonnell AE, Metz CE, Zarins CK. Critical evaluation of stress testing in the diagnosis of peripheral vascular disease. Surgery. 1982. 91:686–693.
13. Wikström J, Hansen T, Johansson L, Lind L, Ahlström H. Ankle brachial index <0.9 underestimates the prevalence of peripheral artery occlusive disease assessed with whole-body magnetic resonance angiography in the elderly. Acta Radiol. 2008. 49:143–149.
14. Parameswaran GI, Brand K, Dolan J. Pulse oximetry as a potential screening tool for lower extremity arterial disease in asymptomatic patients with diabetes mellitus. Arch Intern Med. 2005. 165:442–446.
15. Schröder F, Diehm N, Kareem S, Ames M, Pira A, Zwettler U, et al. A modified calculation of ankle-brachial pressure index is far more sensitive in the detection of peripheral arterial disease. J Vasc Surg. 2006. 44:531–536.
16. Niazi K, Khan TH, Easley KA. Diagnostic utility of the two methods of ankle brachial index in the detection of peripheral arterial disease of lower extremities. Catheter Cardiovasc Interv. 2006. 68:788–792.
17. Premalatha G, Ravikumar R, Sanjay R, Deepa R, Mohan V. Comparison of colour duplex ultrasound and ankle-brachial pressure index measurements in peripheral vascular disease in type 2 diabetic patients with foot infections. J Assoc Physicians India. 2002. 50:1240–1244.
18. Feigelson HS, Criqui MH, Fronek A, Langer RD, Molgaard CA. Screening for peripheral arterial disease: the sensitivity, specificity, and predictive value of noninvasive tests in a defined population. Am J Epidemiol. 1994. 140:526–534.
19. Szala K, Kostewicz W, Noszczyk W. Application of transcutaneous oxymetry in vascular surgery. Int Angiol. 1988. 7:301–304.
20. Arguedas MR, Singh H, Faulk DK, Fallon MB. Utility of pulse oximetry screening for hepatopulmonary syndrome. Clin Gastroenterol Hepatol. 2007. 5:749–754.
21. Koppel RI, Druschel CM, Carter T, Goldberg BE, Mehta PN, Talwar R, et al. Effectiveness of pulse oximetry screening for congenital heart disease in asymptomatic newborns. Pediatrics. 2003. 111:451–455.
22. Löndahl M, Katzman P, Hammarlund C, Nilsson A, Landin-Olsson M. Relationship between ulcer healing after hyperbaric oxygen therapy and transcutaneous oximetry, toe blood pressure and ankle-brachial index in patients with diabetes and chronic foot ulcers. Diabetologia. 2011. 54:65–68.
23. Potier L, Abi Khalil C, Mohammedi K, Roussel R. Use and utility of ankle brachial index in patients with diabetes. Eur J Vasc Endovasc Surg. 2011. 41:110–116.
24. Hummler HD, Engelmann A, Pohlandt F, Högel J, Franz AR. Decreased accuracy of pulse oximetry measurements during low perfusion caused by sepsis: Is the perfusion index of any value? Intensive Care Med. 2006. 32:1428–1431.
25. Kim MS, Joo YS, Park KH. Results of simultaneous hybrid operation in multi-level arterial occlusive disease. J Korean Surg Soc. 2010. 79:386–392.
26. Park HS, Lee T, Yoon CJ, Kang SK, Min SK, Ha J, et al. Outcomes of endovascular intervention and bypass surgery for femoral artery atherosclerosis. J Korean Surg Soc. 2010. 79:215–222.




 ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download