Abstract
Purpose
Locally advanced rectal cancer may require an intraoperative decision regarding curative multivisceral resection (MVR) of adjacent organs. In bulky tumor cases, ensuring sufficient distal resection margin (DRM) for achievement of oncologic safety is very difficult. This study is designed to evaluate the adequate length of DRM in multiviscerally resected rectal cancer.
Methods
A total of 324 patients who underwent curative low anterior resection for primary pT3-4 rectal cancer between 1995 and 2004 were identified from a prospectively collected colorectal database.
Results
Short lengths of DRM (≤1 cm) did not compromise essentially poor oncologic outcomes in locally advanced rectal cancer (P = 0.736). However, especially in rectal cancers invading adjacent organs, DRM of less than 2 cm showed poor survival outcome. In 5-year and 10-year survival analysis of MVR, a shorter DRM (<2 cm) showed 41.9% and 30.5%, although a longer DRM (≥2 cm) showed 72.4% and 60.2% (P = 0.03, 0.044). In multivariate analysis of MVR, poorly differentiated histology, ulceroinfiltrative growth of tumor, and short DRM (<2 cm) were significant factors for prediction of poor survival outcome, although short DRM was not significantly related to local and systemic recurrence.
Despite efforts to detect rectal cancer at an early stage, advanced rectal cancer invading adjacent organs is not uncommon. In up to 15% of cases, the primary tumor is adherent to adjacent organs as a result of direct malignant invasion or peritumoral inflammatory reaction. Intraoperative assessment of adhesions as malignant or benign has often been debated [1,2].
For patients' quality of life postoperatively, preservation of the sphincter was of significant importance and sphincter saving rectal surgery requires determination of the optimal length of the distal resection margin. In advanced primary tumors invading adjacent organs, curative en bloc resection and ensuring a sufficient length of distal resection margin are very difficult. The current National Comprehensive Cancer Network guidelines recommend a distal resection margin of 4 to 5 cm for partial mesorectal excision and 1 to 2 cm for total mesorectal excision, in patients with low rectal cancer [3]. However, careful pathologic studies have demonstrated that distal intramural spread (DIS) occurs in only 4% of patients with rectal cancer. DIS exceeds 1 cm in only 2 to 5% and 2 cm in 1 to 2% of cases, respectively [4,5]. Thus, distal resection margin of 1 to 2 cm or greater should theoretically be sufficient for the vast majority of patients. Recent reports have suggested that a distal margin of 1 cm may be sufficient [6]. In addition, some reports appear to demonstrate that the length of distal clearance has little importance in determination of local recurrences. While the focus has previously been concentrated on the distal mucosal margin, the clinical resection margin, or mesorectal margin has recently gained importance in rectal cancer surgery [7]. However, sufficient distal resection margin could be ensured by surgeons intraoperatively, instead the result of these margins could not be established during the operation and just could be gained by pathologists postoperatively.s
In cases involving invasion of adjacent pelvic organs, achievement of both a curative resection and sphincter preservation is a challenge for colorectal surgeons. This study is designed to assess the adequate length of distal resection margin in locally advanced rectal cancer requiring treatment with curative multivisceral resection.
A total of 577 consecutive patients, who underwent a low anterior resection for treatment of rectal cancer at the department of surgery, between 1995 and 2004, were identified from a prospectively collected colorectal database. Palliative resection and positive distal resection margin were excluded. Excluding pT1-2 patients, a total of 324 pT3-4 patients were enrolled.
Cancer stage was determined with a surgical specimen by a pathologist according to the 6th edition of the American Joint Committee on Cancer TNM staging system. Follow-up was conducted every 3 months for 2 years after surgery, and every 6 months for 3 years after that. At the time of follow-up, a physical examination, including interview and digital rectal examination, was performed. Serum careinoembryonal antigen level was checked and a simple chest X-ray was taken at 2 to 3 month intervals. Abdominal computed tomography and colonoscopic examinations were performed at 1-year intervals. Recurrence and survival of patients were followed up based on outpatient medical records. The recurrence pattern was classified based on the area where the recurrence was detected for the first time, and local recurrence was defined as tumors that recurred in the pelvic cavity and the anastomotic area. When both of local and systemic recurrence were detected simultaneously, cases were classified into systemic recurrence group.
In general, operative reports did not reliably contain information on adequacy of resection, therefore, distal margins were measured and recorded by the pathologist prior to tissue fixation in the unpinned specimen. The "donuts" created by circular intraluminal staplers were not included in measurement of distal margin length, however, they were examined and found to be negative for tumor in all cases.
Survival rate analysis was performed using a Kaplan-Meier survival curve, and for risk factors affecting survival rate, a Cox regression model was used. A multivariate logistic regression test was performed for analysis of risk factors for recurrence.
Of 324 patients, 270 (83.3%) patients with pT3-4 rectal cancer were treated with standard low anterior resection (standard resection, SR) and 54 (16.7%) patients underwent multivisceral resection (MVR). Mean follow-up period was 49.3 ± 1.4 months. Mean age of patients was 60.1 ± 0.7 years. In SR, male gender was dominant, 162 (60%), while in MVR female was dominant, 41 (75.9%) (P < 0.001). Table 1 showed that ulceroinfiltrative pattern of tumor growth (UI) was shown more frequently in the MVR group (P = 0.005). Also, recurrence rate was higher in the MVR group. However, there were no differences in relation to age, tumor size, distance from anal verge, radiation therapy, perineural invasion / lymphovascular invasion, anastomotic leakage, and histologic grade between the two (Table 1). Multivariate analysis using Cox regression model showed that UI and anastomotic leakage were related significantly to poor overall survival outcome. Additionally, mutivisceral resection affected to shorter disease free survival (Table 2).
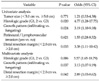
Of MVR, 17 patients showed tumor infiltration to adjacent organs and 37 patients showed inflammatory cellular response. Female was the dominant gender, and the uterus was the most common organ involved by rectal cancer. Patients with systemic recurrence were significantly younger comparing to patients without recurrence (61.7 ± 1.8 vs. 56.1 ± 1.8, P = 0.038) among the MVR group. Within the MVR group, predictive factor for systemic recurrence were younger age, UI and advanced stage (Table 3). In multivariate analysis using Cox regression model for poor survival outcome, poorly differentiated histology (PD), UI and shorter DRM were significantly predictive factors (Table 4).
In a total of 324 patients, short DRM of less than 1 cm did not compromise essentially oncologic poor outcome (Fig. 1A, B) and recurrence. However, a length of less than 2 cm was significantly related to poor survival outcome in the MVR group (Fig. 1C). As commented in Table 4, PD, UI and shorter DRM were significantly predictive factors for poor survival outcome. Among the MVR group, in cases without unfavorable factor (PD and / or UI) there were not significantly different results in survival outcome, although it had shorter DRM (<2 cm) (Fig. 2B). However, In cases with unfavorable factors there was significant differences between shorter and longer DRM group for survival outcome (Fig. 2A).
Multivisceral resection is planned before surgery in only a few patients. The decision to extend the resection to include adjacent organs or structures is made during surgery in most cases. Whether infiltration to adjacent organs was caused by true tumor infiltration or as a result of inflammatory celluar response could not be determined based on histopathological findings after surgery [3]. Adherence of the tumor to adjacent structures demonstrated histological tumor invasion in approximately 50 to 85% of cases [1,8-11]. Among our cases, 28 of 54 (51.9%) had adhesion due to direct tumor infiltration. This finding has led some to suggest dissection of the rectum free from structures that appear to be macroscopically infiltrated, extending the operation, only if separation is not feasible [12]. Goals of treatment of rectal cancer are to cure and to maintain good quality of life, including urinary and sexual function. For achievement of these goals, ensuring an adequate length of distal resection margin for preservation of the anal sphincter was an essential challenge to colorectal surgeons.
Traditionally, the shortest curative distal clearance (DC) has been said to be 2 cm from the outer edge of the tumor [13], while some reports have suggested that a DC of 1 cm may be sufficient [4]. In addition, recent reports appear to demonstrate that length of the distal clearance has little importance in determination of local recurrence, while the clinical resection (CRM), lateral resection margin, has recently gained importance in rectal cancer surgery [7,14]. In this study, this finding led to some limitations of absence of CRM, because CRM was a relatively recent concept and has only been recently applied. Regarding an explanation for CRM, in our institute there has been no case of a cancer positive doughnut as a resection margin and insufficient margin of a cancer positive doughnut was included as an incomplete resection of palliative surgery and was excluded in this study.
Recently, it has been postulated that down-staging of low rectal cancer after preoperative radiation might reduce distal intramural spread to less than 1 cm [4,15]. Two studies have reported distal intramural spread after chemoradiotherapy of greater than 0.5 cm in 9% and 40% of patients, while spread of 1 cm was present in only 0% and 5% [6,16]. However, in this study, preoperative chemoradiation therapy was performed in only a small number of patients. This was a second limitation of our study, because patients with a locally advanced cancer and with a higher risk of distal intramural spread, like infiltrative growing pattern, were generally selected for preoperative radiation in other studies [17,18]. This might result in reduction of the number of patients with significant intramural spread and its actual extent.
Nevertheless, in intraoperative decision making to include the extent of resection, the length of DRM is important in deciding on preservation or scarification of the anal sphincter.
As commented in Fig. 2, poorly differentiated histology and ulceroinfiltrative pattern of tumor growth was important factor for prediction of poor survival outcome. And surgeons can make a decision for these two factor preoperatively using colonoscopy, pathologic report of colonoscopic biopsy, and abdominal imaging. So, especially in cases of T4 rectal cancer with unfavorable factors, above mentioned, surgeons should make a every effort to ensure a sufficient resection margin.
In conclusion, our data suggests that a distal margin of 2 cm or more could ensure oncologic safety in cases of locally advanced rectal cancer invading to adjacent organs and early conversion to abdominoperineal resection could provide an opportunity to compensate for an initial inappropriate decision regarding low anterior resection with insufficient resection margin. In addition, further evaluation should be needed in order to assess the adequate length of DRM and CRM in cases of locally advanced rectal cancer treated with multivisceral curative resection.
Generally, a short length of distal resection margin in locally advanced rectal cancer did not compromise essentially poor oncologic outcome. However, the length of less than 2 cm in the MVR may compromise unadequate resection. Tumors which involved adjacent organs has a character of infiltrative growth and poorly differentiated histology. And these factor are related to a poor survival course. Therefore, in treating locally advanced rectal cancer invading to adjacent organs, every effort should be made for ensuring sufficient length of distal resection margin.
Figures and Tables
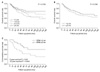 | Fig. 1Comparison of overall survival benefit according to the length of distal resection margin. (A) Categorized distal resection margin (DRM) in all patients. (B) <2 cm vs. ≥2 cm in all patients. (C) In the multivisceral resection group, significance of the length more than 2 cm as an adequate length of distal resection margin. |
 | Fig. 2Analysis of predictive factor for poor survival outcome in the multivisceral resection group. (A) In cases with poorly differentiated histology and/or ulceroinfiltrative pattern of tumor growth, shorter distal resection margin (DRM) (<2 cm) was related to poor survival outcome. (B) In cases without unfavorable factors, shorter DRM did not essentially compromise poor outcome. |
Table 2
Univariate and multivariate analysis using a Cox regression test adherent to disease free and overall survival

References
1. Lehnert T, Methner M, Pollok A, Schaible A, Hinz U, Herfarth C. Multivisceral resection for locally advanced primary colon and rectal cancer: an analysis of prognostic factors in 201 patients. Ann Surg. 2002. 235:217–225.
2. Lopez MJ. Multivisceral resections for colorectal cancer. J Surg Oncol. 2001. 76:1–5.
3. National Comprehensive Cancer Network (NCCN). Colon cancer and rectal cancer guidelines, ver. 1. 2007. Washington: National Comprehensive Cancer Network (NCCN).
4. Moore HG, Riedel E, Minsky BD, Saltz L, Paty P, Wong D, et al. Adequacy of 1-cm distal margin after restorative rectal cancer resection with sharp mesorectal excision and preoperative combined-modality therapy. Ann Surg Oncol. 2003. 10:80–85.
5. Kwok SP, Lau WY, Leung KL, Liew CT, Li AK. Prospective analysis of the distal margin of clearance in anterior resection for rectal carcinoma. Br J Surg. 1996. 83:969–972.
6. Guillem JG, Chessin DB, Shia J, Suriawinata A, Riedel E, Moore HG, et al. A prospective pathologic analysis using whole-mount sections of rectal cancer following preoperative combined modality therapy: implications for sphincter preservation. Ann Surg. 2007. 245:88–93.
7. Birbeck KF, Macklin CP, Tiffin NJ, Parsons W, Dixon MF, Mapstone NP, et al. Rates of circumferential resection margin involvement vary between surgeons and predict outcomes in rectal cancer surgery. Ann Surg. 2002. 235:449–457.
8. Lopez MJ, Monafo WW. Role of extended resection in the initial treatment of locally advanced colorectal carcinoma. Surgery. 1993. 113:365–372.
9. Eisenberg SB, Kraybill WG, Lopez MJ. Long-term results of surgical resection of locally advanced colorectal carcinoma. Surgery. 1990. 108:779–785.
10. Gall FP, Tonak J, Altendorf A. Multivisceral resections in colorectal cancer. Dis Colon Rectum. 1987. 30:337–341.
11. Heslov SF, Frost DB. Extended resection for primary colorectal carcinoma involving adjacent organs or structures. Cancer. 1988. 62:1637–1640.
12. Montesani C, Ribotta G, De Milito R, Pronio A, D'Amato A, Narilli P, et al. Extended resection in the treatment of colorectal cancer. Int J Colorectal Dis. 1991. 6:161–164.
13. Pollett WG, Nicholls RJ. The relationship between the extent of distal clearance and survival and local recurrence rates after curative anterior resection for carcinoma of the rectum. Ann Surg. 1983. 198:159–163.
14. Kim SJ, Choi YJ, Kang JG. Clinicopathologic analysis of mesorectal spread of rectal cancer with whole mount section. J Korean Surg Soc. 2010. 78:298–304.
15. Kuvshinoff B, Maghfoor I, Miedema B, Bryer M, Westgate S, Wilkes J, et al. Distal margin requirements after preoperative chemoradiotherapy for distal rectal carcinomas: are < or = 1 cm distal margins sufficient? Ann Surg Oncol. 2001. 8:163–169.
16. Kinoshita H, Watanabe T, Yanagisawa A, Nagawa H, Kato Y, Muto T. Pathological changes of advanced lower-rectal cancer by preoperative radiotherapy. Hepatogastroenterology. 2004. 51:1362–1366.
17. Shirouzu K, Isomoto H, Kakegawa T. Distal spread of rectal cancer and optimal distal margin of resection for sphincter-preserving surgery. Cancer. 1995. 76:388–392.
18. Williams NS, Dixon MF, Johnston D. Reappraisal of the 5 centimetre rule of distal excision for carcinoma of the rectum: a study of distal intramural spread and of patients' survival. Br J Surg. 1983. 70:150–154.




 ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download