Abstract
Purpose
Postsurgical anemia is one of the common unpleasant postoperative sequels during the early postoperative period after gastrectomy, for which no standard care has been established. To facilitate proper management, we investigated the clinical features of postsurgical anemia and sought to identify the factors affecting its subsequent recovery.
Methods
A retrospective review of 406 consecutive gastric cancer patients who underwent gastrectomy without systemic chemotherapy between August 2008 and September 2009. Clinical courses of postsurgical anemia were monitored at 3, 6, and 12 months post-surgery. Clinicopathological factors affecting recovery of postsurgical anemia were analyzed using a multivariate logistic regression model.
Results
The study subjects consisted of 265 males and 141 females (mean age, 61.8 years). After operation, 318 (78.3%) presented with postsurgical anemia, and 217 (66.7%) and 47 (11.6%) had mild or moderate anemia, respectively, at the time of discharge. During the follow-up, 173 (54.4%) of the 318 with postsurgical anemia showed a spontaneous recovery at 3 months post-surgery, but no significant changes were observed in postsurgical anemia at 6 or 12 months post-surgery. Univariate and multivariate analysis revealed that old age (≥60 years), preoperative anemia, anemia severity (moderate anemia), and total gastrectomy were independent factors that adversely affect the spontaneous recovery of post-surgical anemia after gastrectomy.
Despite its decreasing global incidence over the past few decades, gastric carcinoma remains one of the most common malignancies in many East Asian countries [1]. In Korea, gastric carcinoma is the most prevalent malignant neoplasm and continues to affect over 2,500 patients per year [2]. However, with widespread implementation of screening programs, early gastric cancer accounts for nearly 50% of all gastric cancers, and 5-year survival has reached up to 63 to 73% after curative resection [3-5]. Given advances in the treatment techniques and the early diagnosis of gastric cancer, proper management of functional and nutritional impairments after gastric cancer surgery has also become a primary treatment concern in gastric cancer [6].
Postsurgical anemia is frequently encountered during the early postoperative period after gastrectomy and may impair physical performance and postoperative recovery. However, no standard care for postsurgical anemia, such as, concerning the use of iron or the best route for iron supplementation, has been established so far [7,8]. In the studies regarding orthopedic or cardiac surgery, oral or intravenous iron supplementation showed little efficacy for postsurgical anemia [9-12]. However, unlike patients undergoing orthopedic or cardiac surgery, patients with gastrectomy inevitably suffer from poor iron absorption from the gastrointestinal tract, and thus, this may adversely affect the physiologic recovery from postsurgical anemia [13]. Therefore, the use of iron supplementation for postsurgical anemia needs to be further evaluated in the subset of patients undergoing gastrectomy.
To facilitate proper management of postsurgical anemia, a comprehensive understanding about its clinical features is essential. Its prevalence, subsequent evolution, and the factors affecting the recovery should be taken into consideration when planning a treatment for postsurgical anemia. Therefore, we investigated clinical features of postsurgical anemia after gastrectomy, and sought to identify clinicopathological factors that affect its subsequent recovery.
Between August 2008 and September 2009, 649 patients underwent curative surgery for gastric carcinoma at our institute. Of these patients, 198 patients that underwent preoperative or postoperative chemotherapy, 12 with combined resection of other organs, and 40 that experienced disease recurrence during the follow-up were excluded. Finally, 406 patients that received gastrectomy alone for the treatment of gastric carcinoma and followed for at least one year after surgery were enrolled in the present study. Patient data, such as, demographic characteristics, pathologic results, operative details, postoperative morbidity and mortality, and hospital courses were prospectively constructed using our electronic database recording system.
Postsurgical anemia was defined according to the World Health Organization definition based on hemoglobin (Hgb) value (Hgb < 13 g/dL for males and < 12 g/dL for females). The severity of anemia was also classified as mild (Hgb ≥ 10 g/dL), moderate (7 g/dL ≤ Hgb < 10 g/dL), or severe (Hgb < 7 g/dL) based on postoperative Hgb concentration [14].
During the follow-up, all patients were monitored until 12 months post-surgery, with regular blood test on 3, 6, and 12 months post-surgery. No specific treatment was given to patients with postsurgical anemia. Instead, additional laboratory test for iron deficiency, including serum iron and ferritin and total iron biding capacity, was carried out when patients showed microcytic or hypochromic anemia on regular blood test from postoperative 3 months, and oral iron supplementation was indicated only for postsurgical anemia with an evidence of iron deficiency. Consequently, 11 patients received oral iron supplementation during the follow-up.
Distal or total gastrectomy with regional lymph node dissection was performed in all patients. D2 lymph node dissection, as outlined by the Japanese Gastric Cancer Association, was the standard procedure used for advanced gastric cancer, and D1 plus beta lymph node dissection the standard procedure for early gastric cancer [15]. Laparoscopic surgery was indicated for patients with a preoperative diagnosis of cT1-2N0 gastric cancer. Billroth I reconstruction was the primary procedure used after distal gastrectomy, and Billroth II or Roux-en Y gastrojejunostomy when gastroduodenostomy was not feasible because of concerns about anastomosis failure or the need for wide stomach resection. Roux-en Y esophagojejunostomy without a pouch, was performed routinely after total gastrectomy.
Patients were perioperatively managed using a standardized clinical pathway protocol. For example, no preoperative bowel preparation or nasogastric tube was used. Patients were administered an oral diet from postoperative day 1, and intravenous fluid was restricted to 20 to 25 mL/kg/day during the first three postoperative days. Prophylactic antibiotics were administered before skin incision and continued until 12 hours after surgery. Laboratory tests, such as, complete blood cell counts and blood chemistry, were regularly performed on postoperative days 1, 3, and 5. Transfusion was indicated for anemia with Hgb concentration of <6 g/dL or active postoperative bleeding [16]. Hospital discharge was targeted for postoperative day 8, and objective discharge criteria were used to make decisions, that is, no sign of postoperative complications, the ability to ambulate without assistance, tolerable pain on oral analgesia, able to consume more than 70 per cent of meals, and a willingness to go home.
Continuous data were converted into means (standard deviations [SDs]) and analyzed using the Student's t-test. The chi-square test was used to analyze categorical data. When analyzing risk factors, continuous data were dichotomized into categorical data, which enables the chi-square test and logistic regression analysis to be used for univariate and multivariate analysis, respectively. All statistical analyses were performed using SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA). P-values of < 0.05 were regarded statistically significant.
The demographic and treatment characteristics of the 406 patients are summarized in Table 1. The study subjects consisted of 265 males and 141 females of mean age (SD) 61.8 (11.2) years. One hundred and fifty five (38.2%) had underlying medical comorbidities at the time of operation. Distal gastrectomy was performed in 342 (84.2%), and total gastrectomy in 64 (15.8%) patients. Laparoscopic surgery was performed in 222 (54.75%) patients. Based on final pathologic examinations and the seventh edition of the Union for International Cancer Control tumor-node-metastasis classification, there were 326 stage IA and 80 stage IB patients.
Postoperatively, 318 (78.3%) patients presented with postsurgical anemia, and these included 30 (7.4%) patients with a postoperative bleeding complication. Mean estimated intraoperative blood loss (mL) was 175 ± 39, and mean change in Hgb concentration immediately after surgery was 2.3 ± 1.4 g/dL. Forty one (10.1%) patients received a blood transfusion postoperatively. Because we sought to monitor the postoperative recovery of serum Hgb level from the baseline level at the time of discharge, we decided to include the patients receiving perioperative blood transfusion based on their last blood test results. Finally, at the time of discharge from hospital (based on the last blood test before discharge), 271 (66.7%) patients had mild and 47 (11.6%) had moderate postsurgical anemia, but no patient had severe anemia.
Of the 341 patients without preoperative anemia, 253 (74.2%) developed postsurgical anemia. Table 2 summarizes the risk factors of developing postsurgical anemia in patients without preoperative anemia. Univariate analysis showed that old age, female sex, lower body mass index (BMI), open surgery, D2 lymph node dissection, and total gastrectomy were significantly associated with the development of postsurgical anemia after gastrectomy. As for reconstruction types, Roux-en Y esophagojejunostomy was significantly related to the development of postsurgical anemia, but patients with distal gastrectomy showed no significant difference of postsurgical anemia according to the reconstruction techniques (P = 0.589, Fisher's exact test). Therefore, reconstruction type was excluded in the multivariate analysis. Multivariate analysis revealed that old age (≥60 years; odds ratio [OR], 1.87; 95% confidence interval [CI], 1.10 to 3.16), a female sex (OR, 1.89; 95% CI, 1.05 to 3.40), lower BMI (< 23; OR, 2.26; 95% CI, 1.21 to 4.24), and total gastrectomy (OR, 6.61; 95% CI, 1.95 to 22.41) were independent risk factors of developing postsurgical anemia after gastrectomy.
Table 3 present postoperative courses of postsurgical anemia up to 12 months post-surgery. Of the 318 patients with postsurgical anemia, 173 (54.4%) achieved a spontaneous recovery at 3 months post-surgery without specific treatment. Patients with mild postsurgical anemia showed significantly better spontaneous recovery by 3 months post-surgery than those with moderate postsurgical anemia (59.4% vs. 25.5%; P < 0.001). However, no significant change in the recovery of postsurgical anemia was observed at 6 or 12 months postoperatively for both patient groups with mild and moderate postsurgical anemia. During the follow-up, only 11 (3.5%) of 318 patients with postsurgical anemia showed microcytic or hypochromic anemia with iron deficiency based on the blood test from the postoperative 3 months, and received oral iron supplementation.
Interestingly, of the 88 patients that did not develop postsurgical anemia after operation, only 9 (10.2%) newly developed anemia by postoperative 3 months, and 6 of them presented with anemia until 12 months post-surgery.
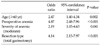
As we mentioned earlier, 11 postsurgical patients with iron deficiency received oral iron supplementation during the follow-up, and thus these patients were excluded from the analysis of factors affecting the recovery of postsurgical anemia to exclude the effects of iron treatment. Table 4 presents a summary of our analysis of predictors of persistent postsurgical anemia by 12 months postoperatively. According to univariate analysis, old age, the presence of preoperative anemia, severity of anemia (moderate), reconstruction type, and total gastrectomy were significantly associated with persistent postsurgical anemia by 12 months. In the subgroup analysis of patients with distal gastrectomy, there was no significant difference in the recovery of postsurgical anemia between different types of reconstruction procedure (P = 0.140, fisher's exact test). Finally, multivariate analysis revealed that old age (≥60 years; OR, 2.47; 95% CI, 1.40 to 4.34), preoperative anemia (OR, 4.87; 95% CI, 2.48 to 7.96), moderate postsurgical anemia (OR, 2.19; 95% CI, 1.03 to 4.63), and total gastrectomy (OR, 4.14; 95% CI, 2.15 to 7.97) were independent risk factors that adversely affect the spontaneous recovery of postsurgical anemia (Table 5).
Postsurgical anemia is common postoperative sequel during the early postoperative period after gastrectomy, and probably adversely affects physical performance and recovery. However, no clear consensus has been reached regarding the treatment of postsurgical anemia after gastrectomy, such as, whether to use iron or to determine the optimum route of iron supplementation [17]. The proper management of postsurgical anemia after gastrectomy may be best approached from a comprehensive understanding of its clinical features, but little is known about this condition. This study was performed as a pilot study for planning a treatment of postsurgical anemia after gastrectomy. In this study, we found that nearly 40% of patients with postsurgical anemia achieved a spontaneous recovery at 3 months post-surgery, but after then no significant recovery was observed until postoperative 12 months. This may suggest that spontaneous recovery of postsurgical anemia can be expected until 3 months post-surgery, but proper intervention may be required for postsurgical anemia persisting until 3 months postsurgery. However, no studies have evaluated proper treatment of postsurgical anemia, such as the efficacy of iron supplementation or the best route of iron supplementation, in patients undergoing gastrectomy. Therefore, proper management for postsurgical anemia needs to be further evaluated in further clinical trials.
In the present study, old age, preoperative anemia, severity of anemia (moderate anemia), and total gastrectomy were found to be independent factors adversely affecting the recovery of postsurgical anemia. This is probably because elderly patients or patients that undergo total gastrectomy are more likely to suffer from iron malabsorption due to poor oral intake and malnutrition [18,19]. Furthermore, patients with preoperative anemia possibly have underlying predisposition for the development of anemia. Therefore, our study suggests that the treatment of postsurgical anemia may require tailored approaches for these patients, such as an earlier active intervention or intravenous iron supplementation rather than oral supplementation. However, this also should be evaluated by clinical trials.
The treatment of postsurgical anemia, especially with respect to the efficacy of postoperative iron supplementation is an issue of long-standing debate [6,7]. Inflammatory response after surgery reduces serum iron and transferrin and increases serum ferritin, which is indicative of a state of functional iron deficiency [20,21], and these physiologic changes may negate the effects of iron supplementation during the postoperative period. In fact, several studies have failed to identify a benefit of iron supplementation for the treatment of anemia after non-abdominal surgeries [9-12]. However, unlike patients undergoing orthopedic or cardiac surgery, patients with gastrectomy inevitably suffer from poor iron absorption from the gastrointestinal tract, and thus, this may adversely affect the physiologic recovery from postsurgical anemia [22]. These arguments urge that the efficacy of iron supplementation during the treatment of postsurgical anemia and the optimal route of iron supplementation needs to be determined in patients undergoing gastrectomy.
It is well known that iron absorption is impaired in a multifactorial manner after gastrectomy, and reduced food intake, low gastric acidity, rapid gastric emptying, and bypass of the upper gastrointestinal tract have all been reported to contribute [22]. However, the extent and clinical consequences of iron malabsorption have not been fully investigated. In the present study, only six of 88 patients that did not develop postsurgical anemia developed anemia at 12 months postoperatively. This observation suggests that iron metabolism is relatively well conserved in normal patients despite gastrectomy. Turnberg [23], in a experimental study of iron absorption in patient with gastrectomy, found that iron absorption was greater in a gastrectomy group than in a non-anemic control volunteer group. Kimber et al. [24] also concluded that iron malabsorption does not necessarily follow gastrectomy. Based on these previous studies and our results, we consider that the extent of iron malabsorption after gastrectomy is less likely to result in impaired hematopoiesis in normal patients, but that it has a serious impact on the physiological compensation required for recovery from postsurgical anemia.
Old age, lower BMI, and total gastrectomy were independent risk factors of developing postsurgical anemia after gastrectomy. It may be due to the increased risk of intraoperative bleeding or increased vulnerability to hemodilution by perioperative intravenous fluid administration in the patients with these characteristics. The amount of intraoperative bleeding is undoubtedly the most important factor for developing postsurgical anemia. However, accurate measurement of the amount of intraoperative bleeding is seldom available in many clinical settings and sometimes even inconvincible. Therefore, we could not include the amount of intraoperative bleeding in our study, and thus independent risk factors, like old age, lower BMI, and total gastrectomy, are possibly related the intraoperative or postoperative bleeding rather than its independent correlation with the development of postsurgical anemia. However, under the clinical circumstances where accurate measurement of intraoperative or postoperative blood loss is not readily available, these factors can be used to predict the risk of developing the postsurgical anemia after gastrectomy.
In summary, based on our results, a spontaneous recovery of postsurgical anemia can be expected until 3 months post-surgery, but proper intervention may be required for postsurgical anemia persisting until postoperative 3 months. In addition, factors adversely affecting the recovery of postsurgical anemia should be taken into consideration in treatment planning for postsurgical anemia. Considering the differences in postoperative physiology of iron metabolism in patients undergoing gastrectomy, proper treatment of postsurgical anemia, such as the efficacy of the use of iron or the optimum route of iron supplementation, needs to be further evaluated in future clinical trials.
Figures and Tables
Table 2
Univariate and multivariate analysis of risk factors of developing postsurgical anemia in patients without preoperative anemia

ACKNOWLEDGEMENTS
This study was supported by the Chonnam National University Hospital Research Institute of Clinical Medicine (grant no. CRI 11-066-1).
References
1. Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010. 127:2893–2917.
2. Jung KW, Park S, Kong HJ, Won YJ, Boo YK, Shin HR, et al. Cancer statistics in Korea: incidence, mortality and survival in 2006-2007. J Korean Med Sci. 2010. 25:1113–1121.
3. Ahn HS, Lee HJ, Yoo MW, Jeong SH, Park DJ, Kim HH, et al. Changes in clinicopathological features and survival after gastrectomy for gastric cancer over a 20-year period. Br J Surg. 2011. 98:255–260.
4. Choi IJ. Gastric cancer screening and diagnosis. Korean J Gastroenterol. 2009. 54:67–76.
5. Kitano S, Shiraishi N, Uyama I, Sugihara K, Tanigawa N. Japanese Laparoscopic Surgery Study Group. A multicenter study on oncologic outcome of laparoscopic gastrectomy for early cancer in Japan. Ann Surg. 2007. 245:68–72.
6. Schölmerich J. Postgastrectomy syndromes--diagnosis and treatment. Best Pract Res Clin Gastroenterol. 2004. 18:917–933.
7. Beris P, Muñoz M, García-Erce JA, Thomas D, Maniatis A, Van der Linden P. Perioperative anaemia management: consensus statement on the role of intravenous iron. Br J Anaesth. 2008. 100:599–604.
8. Goodnough LT, Shander A, Spivak JL, Waters JH, Friedman AJ, Carson JL, et al. Detection, evaluation, and management of anemia in the elective surgical patient. Anesth Analg. 2005. 101:1858–1861.
9. Bernière J, Dehullu JP, Gall O, Murat I. Intravenous iron in the treatment of postoperative anemia in surgery of the spine in infants and adolescents. Rev Chir Orthop Reparatrice Appar Mot. 1998. 84:319–322.
10. Karkouti K, McCluskey SA, Ghannam M, Salpeter MJ, Quirt I, Yau TM. Intravenous iron and recombinant erythropoietin for the treatment of postoperative anemia. Can J Anaesth. 2006. 53:11–19.
11. Madi-Jebara SN, Sleilaty GS, Achouh PE, Yazigi AG, Haddad FA, Hayek GM, et al. Postoperative intravenous iron used alone or in combination with low-dose erythropoietin is not effective for correction of anemia after cardiac surgery. J Cardiothorac Vasc Anesth. 2004. 18:59–63.
12. Muñoz M, Naveira E, Seara J, Palmer JH, Cuenca J, García-Erce JA. Role of parenteral iron in transfusion requirements after total hip replacement. A pilot study. Transfus Med. 2006. 16:137–142.
13. Stevens AR Jr, Pirzio-biroli G, Harkins HN, Nyhus LM, Finch CA. Iron metabolism in patients after partial gastrectomy. Ann Surg. 1959. 149:534–538.
14. Clark SF. Iron deficiency anemia. Nutr Clin Pract. 2008. 23:128–141.
15. Nakajima T. Gastric cancer treatment guidelines in Japan. Gastric Cancer. 2002. 5:1–5.
16. Simon TL, Alverson DC, AuBuchon J, Cooper ES, DeChristopher PJ, Glenn GC, et al. Practice parameter for the use of red blood cell transfusions: developed by the Red Blood Cell Administration Practice Guideline Development Task Force of the College of American Pathologists. Arch Pathol Lab Med. 1998. 122:130–138.
17. Tovey FI, Clark CG. Anaemia after partial gastrectomy: a neglected curable condition. Lancet. 1980. 1:956–958.
18. Bae JM, Park JW, Yang HK, Kim JP. Nutritional status of gastric cancer patients after total gastrectomy. World J Surg. 1998. 22:254–260.
19. Bozzetti F, Ravera E, Cozzaglio L, Dossena G, Agradi E, Bonfanti G, et al. Comparison of nutritional status after total or subtotal gastrectomy. Nutrition. 1990. 6:371–375.
20. van Iperen CE, Kraaijenhagen RJ, Biesma DH, Beguin Y, Marx JJ, van de Wiel A. Iron metabolism and erythropoiesis after surgery. Br J Surg. 1998. 85:41–45.
21. Weiss G, Goodnough LT. Anemia of chronic disease. N Engl J Med. 2005. 352:1011–1023.
22. Geokas MC, McKenna RD. Iron-deficiency anemia after partial gastrectomy. Can Med Assoc J. 1967. 96:411–417.
23. Turnberg LA. The absorption of iron after partial gastrectomy. Q J Med. 1966. 35:107–118.
24. Kimber C, Patterson JF, Weintraub LR. The pathogenesis of iron deficiency anemia following partial gastrectomy. A study of iron balance. JAMA. 1967. 202:935–938.




 ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download