Abstract
Purpose
S-plasty for pilonidal disease reduces the tension on the midline by distributing it diagonally and flattening the natal cleft. The aim of this study was to evaluate the outcomes of S-plasty on simple midline primary closure and the clinical features of pilonidal patients in a low incidence country.
Methods
S-plasty was applied on 17 patients from July 2008 to October 2010. Data of these patients were collected with computerized prospective database forms during a perioperative period and via telephone interview for follow-up. Surgical site infection (SSI) was defined according to the Center for Disease Control guidelines. The severity of surgical site infection was graded.
Sacrococcygeal pilonidal disease is an inflammatory broad spectrum disorder in the intergluteal region [1,2]. It is prevalent in Mediterranean countries, but rare in East Asia [2]. The treatment depends on status of pilonidal disease, various treatments have been described [3,4], and the surgical removal of devitalized tissue remains a definitive treatment [4-6]. Though closure on the excised wound remains controversial, a primary closed wound heals more rapidly than a laying open wound and needs simple dressing, and also the primary closure is more simple and easier than the flap surgery [6]; however, the primary closed wound have been reported with a high impaired healing rate or recurrence caused by the tension perpendicular to the gluteal midline. For this reason, off-midline closure [5,7,8] and oblique fusiform incision [9] have been introduced, but these procedures are vulnerable to perpendicular tension for these are basically fusiform excision. During these procedures, the normal tissue much larger than the lesion must be inevitably removed [10]. To reduce the tension of fusiform excision by distributing the force in multiple directions and minimize the loss of normal tissue, S-plasty can be applied [10,11]. A low impaired healing or recurrence was reported with S-plasty and bilateral gluteus maximus fascia advancing flap [10], but the procedures including a flap surgery are not as easy as the primary closure and needs caseload to gain proficiency [12]; especially in a low incidence area, gaining of proficiency is difficult so a simple procedure with low complication is necessary. The aim of this study was to present the outcomes of S-plasty without a flap as simple as the midline primary closure and the clinical features of pilonidal patients in a low incidence country.
A consecutive series of 17 patients with pilonidal disease undergoing S-plasty at the Hospital (the final referral military hospital, in South Korea) from July 2008 to October 2010 included in the study. The diagnostic criteria for inclusion were chronic discharge and suppuration from the midline primary pits, or acute pilonidal abscess. All procedures of S-plasty were performed under spinal anesthesia. Data of these patients were collected with computerized prospective database forms during a perioperative period and via telephone interview for follow-up. Data included patient demographics, whether each patient's treatment had been for primary or recurrent disease, duration of symptom, numbers of previous treatment, length of hospital stay, and time to completion of treatment. The healing time defined as days from the day of starting treatment to the last day of dressing or treatment. The degree of hairiness in lower back was graded by the Ferriman-Gallwey (FG) scoring system [13]. A score of 0 to 4 assigned, based on the visual density of terminal hairs, a score of 0 represented the absence of terminal hair, and a score of 4 extensive terminal hair. In this study, we modified the hairiness grade; we considered more than 3 of FG score as hairy but lower than 2 not hairy. With regard to the follow-up telephone interviews (all performed in December 2010), each patient was asked to answer postoperative course and to whether further treatment was needed. The surgical site infection (SSI) was defined according to the Center for Disease Control (CDC) guidelines [14]. The severity of surgical site infection was graded [15,16]. Grade I was defined as a wound infection treated by opening of the wound at the bedside. Grade II was the same as for I but needed antibiotics. Grade IIIa complication was closed dehiscent wound under local anesthesia. Grade IIIb was defined as the complete wound dehiscence or wound needed to be closed under spinal or general anesthesia. Statistical analysis was performed with SPSS ver. 15 (SPSS Inc., Chicago, IL, USA). A P-value of less than 0.05 was regarded statistically significant. Mann-Whitney U test were used for non-parametric variables.
The initial treatment for acute pilonidal abscess was performed in the prone jackknife position. Under local anesthesia, incision and drainage was done; the skin incision should be made where pus could drain effectively and as close as to the primary pit in order to reduce incision length at a delayed surgery. The wound was dressed once daily. Nine to 15 days later, the definitive surgery was performed.
S-plasty was performed for the definitive treatment of pilonidal disease (Fig. 1). We used ultrasonogram for demarcating the lesion especially when no secondary openings were found. Under spinal anesthesia, the patient was placed in the prone jackknife position. After shaving off the hair, S-plasty was designed, and the cheeks of buttocks taped apart. The longitudinal axis of incision depended on the axis of devitalized tissue or the secondary openings; the upper end of incision located on the same side of the secondary opening to reduce incision length. To improve wound healing by approximating fresh skin to the midline cleft, the lower end was incised away from the cleft. Excision included the primary sinus and the secondary fistula opening or the previous incision and drainage site; completely removed unhealthy tissue without cutting into it. After achieving hemostasis, a suction drain was placed, and the tapes for traction were removed. While the wound edges were being approximated with hands, we drew lines perpendicular to the wound to match the margin. The wound was closed with mattress sutures of 2-0 Nylon through the epidermis, subcutaneous fat, and postsacral fascia, but nylon sutures left unknotted to help approximate the wound edges. After subcutaneous tissue was sutured with 2-0 or 3-0 absorbable polyglycolic acid, the subcutaneous suture was knotted while the wound edges were being approximated with the neighboring nylon sutures, and then the nylon sutures were knotted from the upper to the lower. The patient was recommended neither lying supine nor sitting for 2 weeks to reduce the shearing force on sacrococcygeal area [17]. Intravenous antibiotics (Cefoxitine) were used for 2 or 3 days, and then oral antibiotics were prescribed for 1 week. Daily dressing on the wound and drainage was done. The drain was removed within 7 days postoperatively or when it was less than 1 mL for 2 consecutive days. The stitches were removed 8 to 14 days postoperatively.
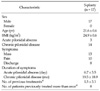
All of 17 patients were male (Table 1), with a mean age of 21 years (range, 19 to 30 years). A palpable mass or swelling was presented in 13 (76.5%), and a history of pain was presented in 10 (58.8%) cases. The mean body mass index (BMI) was 24.9. Three (17.6%) patients were treated with incision and drainage for an acute pilonidal abscess, while 14 patients (82.4%) had chronic disease. The average duration of symptoms from onset to admission was 6.7 days (range, 3 to 10 days) for acute abscess, and 16.1 months (range, 0.5 to 60 months) for chronic pilonidal disease. Among the chronic patients the average numbers of previous treatment were 1.5 (range, 0 to 12), and 8 (57.1%) patients were previously treated more than once, but no patient had undergone any definitive treatment; incision and drainage had been performed in 7 cases, one had been treated with excision of the secondary opening.
Sixteen of 17 patients were hairy (FG score ≥ 3) in lower back (Table 2). Nine (52.9%) patients, hairs were seen in the bisected specimen. The secondary opening was found in 10 (58.8%) cases. Bacterial culture of the discharge or cyst cavity was performed in 8 (47.1%) patients, bacteria were identified in 5 (62.5%) among these patients; Staphylococcus aureus, Staphylococcus capitis, Streptococcus sanguinis, Escherichia coli, and Morganella morganii. No bacteria were cultured in 3 cases.
S-plasty was performed 11.7 days (range, 9 to 15 days) after incision and drainage in the acute abscess patients. The average healing time after S-plasty was 18.1 days, was similar between the acute and the chronic patients (18.7 days vs. 17.9 days, P = 0.68) (Table 3), but it was significantly different between the patients with and without complication (P = 0.002) (Table 4); 14.4 days in 13 patients without complication, but 30 days in 4 patients with complication. The hospital stay after S-plasty was 28 days and different between patients with and without complication (P = 0.006); 20.9 days in 13 patients without complication, but 33.3 days in 4 patients with complication.
All of 17 patients were treated with the primary S-plasty without conversion to other procedure, but 4 patients had a surgery related complication (SSI, and seroma). Two (11.7%) patients developed SSI, one was graded as I, and the other was graded as II. The healing time after S-plasty was 22 days for grade I and 33 days for grade II. Two patients suffered from seroma. There was neither grade IV (life-threatening complication) nor grade V (procedure related death) in this study.
The average follow-up period was 13.5 months (range, 6 to 33 months). No recurrences were observed. No carcinomas were found in pathologic examination.
In this study we presented the surgical outcomes of primary S-plasty as simple and easy as the primary midline closure for the treatment of pilonidal disease and the clinical features of patients in a low incidence country. We found that SSI rate of primary S-plasty is 11.7%, comparable range of reported SSI rates in other procedures, and complication prolongs a healing time.
All of our patients were treated with the primary S-plasty without conversion to other procedure, but 4 patients (23.4%) developed impaired wound healing (SSI, and seroma). The SSI occurred in 2 patients. The SSI rate in this study was upper range of reported SSI rates in the flap surgery (4.9 to 12.8%) [18,19] and consistent with the SSI rate (12.4%, range 0 to 38.5%) of the primary midline closure in 35 studies [20], but it was lower than the SSI rate (33%) in the recent report [21], SSI fulfilled the CDC guidelines. Besides the rate was acceptable, all SSI were low grade, and no severe complication and wound dehiscence occurred. This result may support that S-plasty reduce the tension of midline gluteal cleft by distributing the force in multiple directions. The SSI occurred in lower end of the suture line when it was inappropriately close to the midline cleft by retraction and lost the property of S shape incision. For that reason, we designed the S shape as mentioned above in methods to help the lower end of the incision keep away from the natal cleft and the anus.
Two patients (11.7%) suffered from seroma, and each was treated with drainage or a repeated aspiration. In initial 3 cases of our patients, excision extended down to the postsacral fascia, and we closed the wound only with mattress sutures of 2-0 Nylon through the epidermis, subcutaneous fat, and postsacral fascia. Two of them developed seroma on postoperative days 10 and 12 (one or two days after stitch out). Afterwards, to prevent seroma complication, we did not completely shave off the postsacral fascia and as possible as left healthy tissue over the sacrum [1], and subcutaneous tissue was sutured with absorbable polyglycolic acid [22], and then there was no seroma complication.
The surgical complication prolonged a healing time [21]. The healing time without complication was 14 days, comparable to the range reported in off-midline closure (10 to 15 days) [22,23]. Though a mean healing time was doubled when complication occurred, it was shorter than the duration of open wound healing in the literature (41 to 91 days) [23]. The average healing time after S-plasty was similar between the acute and the chronic disease. The healing time after the initial treatment of acute pilonidal abscess was 30 days, also it was shorter than the duration of open wound healing [23]. The postoperative hospital stay (24 days) in the army corresponds to the time to normal activity in general population, reported to a range from 8 to 30 days in the flap surgery [2,24]. The postoperative hospital stay was relatively long in this study, because all patients were military soldiers and an officer, and they had to be hospitalized without paying money and were discharged from the hospital when they were fit for duty and physical training. Though prolonged hospital stay was weak point of this study, we could precisely observe the process of the wound healing during that period.
The recurrence was reported from 5.6 to 11 percent during oblique excision [9,20,22], and 0.7 percent in S-plasty and bilateral gluteus maximus fascia advancing flap [10]. In our study, no recurrence was developed during 13.5 months (range, 6 to 33 months); even it was relatively a short term and might be a limitation of the present study, but 25 to 100% of recurrence reported within 8 months in the recent studies [9,10,22,24]. Another limitation was that we followed up the patients via a telephone interview, for the former soldiers discharged from military service cannot be physically examined in the army hospital.
For rarity in Korea and lacking of knowledge about pilonidal disease, no patients with the chronic disease had undergone a definitive treatment, and more than half of patients previously treated more than once because of misdiagnosis. The incidence of pilonidal disease varies from races, explained with different hair characteristics and hairiness among races [22]. In general population, males of East Asia were less hairy than Euroamericans counterparts [25], and most of Korean men are not hairy in lower back and hip, but most of our patients were hairy in that region. A mean BMI was 24.9, upper limit of the World Health Organization BMI cut-off point for normal body weight [26], but for overweight in Asian population [27]. These findings may support that hairiness and obesity are predisposing factors in pilonidal disease.
In a low incidence area, pilonidal disease could be misdiagnosed, and this causes morbidity and repeated treatments and may disturb the normal activity of patients. Therefore the precise diagnosis is mandatory and the treatment must be simple and easy, and also the postoperative outcomes should be acceptable.
In this study, we have described that the primary S-plasty for pilonidal disease is as simple as the primary midline closure, and the surgical outcomes are compatible to the results of other surgical treatment including the flap surgery. S-plasty for pilonidal disease can reduce the tension on the excised wound, decrease buttock friction by flattening the natal cleft, and reduce the risk of fecal contamination by keeping the distal end of incision away from anus. We present the primary S-plasty as a feasible treatment option for pilonidal disease in a low incidence country.
Figures and Tables
Fig. 1
S-plasty for pilonidal disease. (A) Decide on area to be excised and mark at outer vertical and horizontal points using ultrasonogram. (B) Draw 1/4 circle (radius is 2 times bigger than width of excision area) from (x) to upper end and from (y) to lower end. (C) Close incision line. Trim line smoothly. (a) Ultrasonogram shows 2.4 × 1.5 × 6 cm pilonidal sinus (ovoid shape hypoechoic lesion). (b) Complete excision of devitalized tissue. (c) After drawing lines perpendicular to wound in order to match margin, wound was closed with mattress sutures of 2-0 Nylon and with 2-0 or 3-0 absorbable polyglycolic acid. (d) Comparing with (Fig. 1D), wound closed with S-plasty reduces tension on midline by distributing it diagonally, flattens the natal cleft, and keeps distal end of incision away from anus.

References
1. Allen-Mersh TG. Pilonidal sinus: finding the right track for treatment. Br J Surg. 1990. 77:123–132.
2. Thompson MR, Senapati A, Kitchen P. Simple day-case surgery for pilonidal sinus disease. Br J Surg. 2011. 98:198–209.
3. Aldemir M, Kara IH, Erten G, Taçyildiz I. Effectiveness of collagenase in the treatment of sacrococcygeal pilonidal sinus disease. Surg Today. 2003. 33:106–109.
4. Armstrong JH, Barcia PJ. Pilonidal sinus disease. The conservative approach. Arch Surg. 1994. 129:914–917.
5. Karydakis GE. Easy and successful treatment of pilonidal sinus after explanation of its causative process. Aust N Z J Surg. 1992. 62:385–389.
6. Washer JD, Smith DE, Carman ME, Blackhurst DW. Gluteal fascial advancement: an innovative, effective method for treating pilonidal disease. Am Surg. 2010. 76:154–156.
7. Karydakis GE. New approach to the problem of pilonidal sinus. Lancet. 1973. 2:1414–1415.
8. Kitchen PR. Pilonidal sinus: experience with the Karydakis flap. Br J Surg. 1996. 83:1452–1455.
9. Mentes O, Bagci M, Bilgin T, Coskun I, Ozgul O, Ozdemir M. Management of pilonidal sinus disease with oblique excision and primary closure: results of 493 patients. Dis Colon Rectum. 2006. 49:104–108.
10. Krand O, Yalt T, Berber I, Kara VM, Tellioglu G. Management of pilonidal sinus disease with oblique excision and bilateral gluteus maximus fascia advancing flap: result of 278 patients. Dis Colon Rectum. 2009. 52:1172–1177.
11. Paolo B, Stefania R, Massimiliano C, Stefano A, Andrea P, Giorgio L. Modified S-plasty: an alternative to the elliptical excision to reduce the length of suture. Dermatol Surg. 2003. 29:394–398.
12. Hallock GG. Is there a "learning curve" for muscle perforator flaps? Ann Plast Surg. 2008. 60:146–149.
13. Ferriman D, Gallwey JD. Clinical assessment of body hair growth in women. J Clin Endocrinol Metab. 1961. 21:1440–1447.
14. Horan TC, Andrus M, Dudeck MA. CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control. 2008. 36:309–332.
15. Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009. 250:187–196.
16. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004. 240:205–213.
17. Russell L. Physiology of the skin and prevention of pressure sores. Br J Nurs. 1998. 7:10841088–1092. 1096 passim
18. Mentes O, Bagci M, Bilgin T, Ozgul O, Ozdemir M. Limberg flap procedure for pilonidal sinus disease: results of 353 patients. Langenbecks Arch Surg. 2008. 393:185–189.
19. Unalp HR, Derici H, Kamer E, Nazli O, Onal MA. Lower recurrence rate for Limberg vs. V-Y flap for pilonidal sinus. Dis Colon Rectum. 2007. 50:1436–1444.
20. Petersen S, Koch R, Stelzner S, Wendlandt TP, Ludwig K. Primary closure techniques in chronic pilonidal sinus: a survey of the results of different surgical approaches. Dis Colon Rectum. 2002. 45:1458–1467.
21. Popeskou S, Christoforidis D, Ruffieux C, Demartines N. Wound infection after excision and primary midline closure for pilonidal disease: risk factor analysis to improve patient selection. World J Surg. 2011. 35:206–211.
22. Akinci OF, Coskun A, Uzunköy A. Simple and effective surgical treatment of pilonidal sinus: asymmetric excision and primary closure using suction drain and subcuticular skin closure. Dis Colon Rectum. 2000. 43:701–706.
23. McCallum IJ, King PM, Bruce J. Healing by primary closure versus open healing after surgery for pilonidal sinus: systematic review and meta-analysis. BMJ. 2008. 336:868–871.
24. Can MF, Sevinc MM, Hancerliogullari O, Yilmaz M, Yagci G. Multicenter prospective randomized trial comparing modified Limberg flap transposition and Karydakis flap reconstruction in patients with sacrococcygeal pilonidal disease. Am J Surg. 2010. 200:318–327.
25. Ewing JA, Rouse BA. Hirsutism, race and testosterone levels: comparison of East Asians and Euroamericans. Hum Biol. 1978. 50:209–215.
26. Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. 2000. 894:i–xii. 1–253.
27. Wen CP, David Cheng TY, Tsai SP, Chan HT, Hsu HL, Hsu CC, et al. Are Asians at greater mortality risks for being overweight than Caucasians? Redefining obesity for Asians. Public Health Nutr. 2009. 12:497–506.




 ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download